-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 135-139
doi:10.5923/j.ajmms.20251501.25
Received: Jan. 2, 2025; Accepted: Jan. 22, 2025; Published: Jan. 24, 2025

Gastropathy Induced by Non-Steroidal Anti-Inflammatory Drugs in Rheumatoid Arthritis
Djabbarova Miyassar Bobokulovna1, Saidova Mukhabbat Mukhidinovna2
1Senior Teacherof the Department of Traditional Medicine and Occupational Diseases of the Bukhara State Medical Institute named after Abu Ali ibn Sino, Uzbekistan
2Candidate of Medical Sciences Associate Professor, Bukhara, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. The article provides data on the incidence of gastropathy in patients with rheumatoid arthritis (RA) receiving therapy with non-selective and selective non-steroidal anti-inflammatory drugs (NSAIDs), which are the most popular means of relieving the symptoms of this disease. NSAIDs can cause serious complications from the gastrointestinal tract (GI) in the form of erosive ulcer lesions of the mucous membrane of the gastroduodenal zone and the development of esophagitis. Taking into account risk factors, prescribing safer selective NSAIDs and gastroprotectors can reduce the frequency of these complications.
Keywords: Rheumatoid arthritis, Nonsteroidal anti-inflammatory drugs (NSAIDs), Gastropathy, Erosive gastritis
Cite this paper: Djabbarova Miyassar Bobokulovna, Saidova Mukhabbat Mukhidinovna, Gastropathy Induced by Non-Steroidal Anti-Inflammatory Drugs in Rheumatoid Arthritis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 135-139. doi: 10.5923/j.ajmms.20251501.25.
1. Relevance
- Rheumatoid arthritis continues to be one of the most relevant pathologies in modern medical practice: on the one hand, this contributes to the prevalence of the disease - up to 2% in the general population; on the other handhigh social and economic importance process, based on high rates of permanent disability in patients and the significant cost of treatment and the necessary laboratory monitoring [12].According to the World Health Organization, 60% of the world's population has gastritis (2023). The frequency of morphological changes in the gastric mucosa is 80% among the adult population. About 40% of the adult population suffers (with more or less pronounced symptoms), but only 5% go to doctors with complaints. More than 30 million people in the world take NSAIDs daily, and in 2/3 of cases - without prescription or medical supervision [1].An annual increase in the number of hospitalizations and deaths associated with complications of NSAID therapy is reported, and the economic costs of their treatment are increasing. Thus, up to 60% of hospitalized patients with gastric bleeding indicate previous use of NSAIDs. The medical and social significance of the problem is such that rheumatologists often call NSAID gastropathy the “second rheumatic disease [13].”Rheumatoid arthritis (RA) is a chronic disease that requires long-term therapy and causes drug-induced pathology of the gastrointestinal tract (GIT). NSAIDs are an important component of complex therapy for rheumatic diseases (RD). At least 68.5% of patients with rheumatoid arthritis regularly take NSAIDs [12]. In the absence of effective therapy, life expectancy in patients with RA is 3 years lower in women and 7 years lower in men, primarily due to the high risk of developing comorbid diseases - cardiovascular pathology, osteoporosis, severe infections, interstitial lung disease, cancer [15].In many patients with RA, life prognosis is as poor as in lymphogranulomatosis, type 2 diabetes mellitus, three-vessel coronary artery involvement, and stroke. RA causes permanent disability in half of patients within the first 3-5 years from the onset of the disease, and after 20 years a third of patients become completely disabled [15].Rheumatoid arthritis (RA) is a chronic disease requiring long-term therapy and causing drug pathology of the gastrointestinal tract (GIT). In the mid-90s. XX century impressive statistics dictated the need to talk about the "epidemic" of this pathology. The use of non-selective NSAIDs has been shown to increase the risk of gastrointestinal bleeding by more than 4 times. The incidence of NSAID gastropathy reached 4% in regular NSAIDs, and the total number of deaths due to this pathology reached 5-15 per 100 thousand people per year [2].In recent years, significant advances have been made in the treatment of RA, which is associated with the expansion of the possibilities of early diagnosis of the disease and timely therapy with non-steroidal anti-inflammatory drugs (NSAIDs). However, their use is associated with the development of a number of side effects, the most common of which is NSAID gastropathy. This complication is characterized by the occurrence of erosive and ulcerative defects on the mucous membrane of the stomach and duodenum [2].Despite a large number of works devoted to the problem of diagnosis and prevention of NSAID gastropathy, the incidence of erosive-ulcerative lesions of the mucous membrane of the gastroduodenal zone and life-threatening complications remains high [2].The widespread introduction into clinical practice of safer selective cyclooxygenase-2 inhibitors (SOG-2) and effective "gastroprotective" drugs is of great preventive importance. Existing international consensus documents recommend stratifying patients taking NSAIDs into risk groups according to their risk factors, which makes it possible to determine the treatment and prevention of NSAID gastropathy [2].The aim of the study was to assess the risk of gastroduodenal SD erosive ulcers induced by NSAIDs based on clinical characteristics and morphological parameters of gastric SD in experimental animals with simulated rheumatoid arthritis with RA.
2. Materials and Methods
- The study was carried out in 3 stages: Retrospective, prospective and morphological experiment, we mainly focus on verified information using the prospective method. In the rheumatology department of the Bukhara Regional Multidisciplinary Medical Center, 138 patients treated with rheumatoid arthritis in 2022 were analyzed.
3. Results
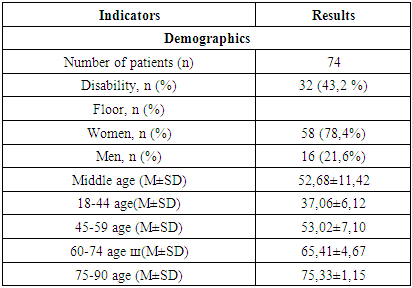
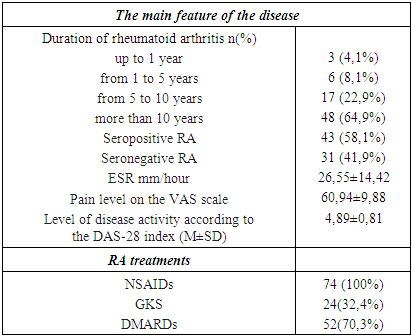
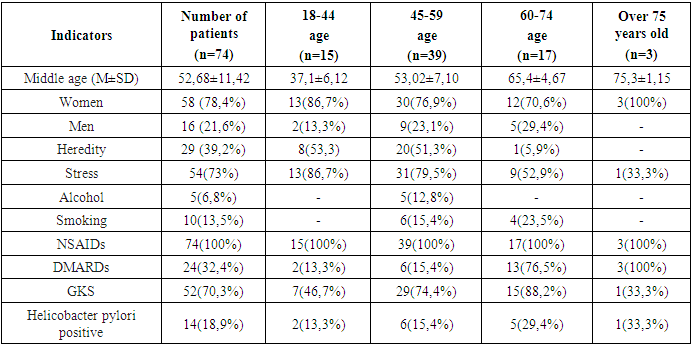
- During a study in the rheumatology department of the Bukhara Regional Multidisciplinary Medical Center, 138 patients aged 19-76 years who received inpatient treatment for rheumatoid arthritis were selected for 6 months (January-June) 2022. The diagnosis of Pevmatoid aptitis was made based on the ACR (1987) and ACR/EULAR (2010) tests. When identifying the disease, the following data were analyzed in detail: the age of the patient, the nature of the disease, its duration, the presence of asopate in the disease, the results and effectiveness of previous treatment, factors contributing to the occurrence of the disease. Disease was assessed based on multiple digit DAS-28 (Disease Activity Score).When determining the incidence of risk factors for gastropathy in patients with peumatoid apitis, the condition of the threads, gender, age, stress, alcohol consumption, smoking, detection of H. pylori, and detection of signs of gastropathy were also assessed. In an analysis of 138 patients undergoing a scientific study, signs of gastropathy were identified in 74 (53.6%) patients with rheumatoid arthritis, and special examinations were carried out.According to the analysis of the study, out of 74 (53.6%) patients, 58 (78.4%) were women, the average age of patients was 51.9±11.6, men - 16 (21.6%), the average age of patients was 51.9±11.6 the average age was 55.2±10.8. When analyzed by World Health Organization (WHO) age classification in 2021, 15 (20.3%) patients in the study were aged 18-44 years, 39 (52.7%) were aged 45-59 years , 17 (22.9%) were 60-74 years old, 3 (4.1%) were 75-90 years old (Table 1).
|
|
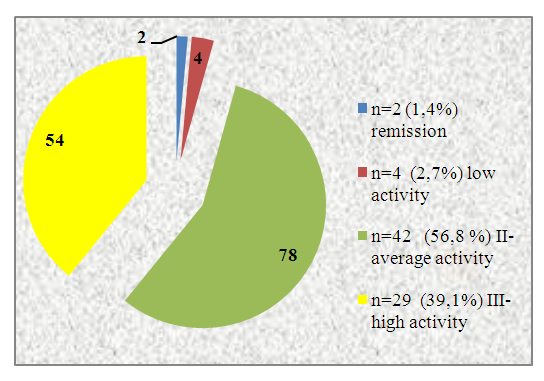 | Figure 1. PA activity level |
|
|
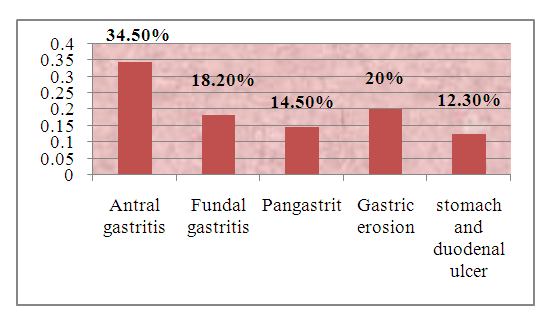 | Figure 2. Morphological changes in the gastric mucosa |
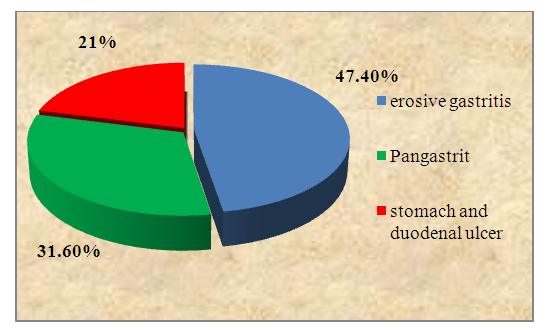 | Figure 3. Results of fluoroscopy in patients with gastropathy |
4. Conclusions
- 1. Gastropathy caused by NSAIDs is often detected in women in the presence of autoaggression factors (stress, heredity, gender, drug polyprogamy, the presence of H. pylori, taking antiplatelet agents), as well as when taking NSAIDs with water for more than five years;2. NSAID gastropathy is manifested predominantly by dyspeptic syndrome (85.1%), the absence of the usual pain syndrome and seasonality. When a pain syndrome was detected, it was found that its elimination was achieved not with food and antacid medications, but with the help of gastroprotective and antibacterial agents for 2-3 days;3. NSAID gastropathy is characterized by a discrepancy between the clinical and endoscopic manifestations of inflammation in the stomach. The mild symptomatic clinical course of NSAID gastropathy corresponds to clear endoscopic and morphological signs of antral gastritis activity;4. Endoscopic examination of patients with RA made it possible to describe in detail the clinical and functional state caused by the aggressive effect of NSAIDs and glucocorticosteroids on the gastric mucosa, to scientifically substantiate the inclusion of drugs that protect the gastric mucosa in the complex treatment of patients in order to prevent inflammation of the gastric mucosa and their subsequent severe complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML