-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 131-134
doi:10.5923/j.ajmms.20251501.24
Received: Dec. 29, 2024; Accepted: Jan. 21, 2025; Published: Jan. 24, 2025

Efficacy of Tubular Microdiscectomy with Flavoplasty in the Treatment of Lumbar Compression Radiculopathy
Akhmedjanov D. U., Karimov A. A.
Republican Specialized Scientific and Practical Medical Center of Endocrinology named after Academician Y.Kh. Turakulov, Tashkent, Uzbekistan
Correspondence to: Akhmedjanov D. U., Republican Specialized Scientific and Practical Medical Center of Endocrinology named after Academician Y.Kh. Turakulov, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The objective of this study was to increase the effectiveness of surgical treatment for lumbar compression radiculopathy (LCR) by assessing the outcomes of tubular microdiscectomy with flavoplasty. A total of 120 patients with LCR were analyzed, undergoing surgery using two approaches: traditional discectomy following W. Caspar's technique and tubular microdiscectomy. The results showed that the tubular method effectively reduces pain intensity, shortens postoperative recovery time, and significantly improves the quality of life for patients.
Keywords: Lumbar compression radiculopathy, Microsurgery, Tubular microdiscectomy, Pain syndrome, Rehabilitation, Flavoplasty
Cite this paper: Akhmedjanov D. U., Karimov A. A., Efficacy of Tubular Microdiscectomy with Flavoplasty in the Treatment of Lumbar Compression Radiculopathy, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 131-134. doi: 10.5923/j.ajmms.20251501.24.
Article Outline
1. Introduction
- One of the most complex and significant manifestations of vertebrogenic pain syndromes is lumbar compression radiculopathy (LCR). This condition is characterized by severe, persistent, and intense pain, leading to a substantial reduction in patient mobility [1].According to statistical data, between 25% and 80% of the European population suffer from back pain [2,3,4]. Furthermore, there is an observed increase in the incidence of conditions leading to disability and temporary loss of working capacity [5,6,7].Radicular back pain is a significant adverse factor as it reduces the quality of life, contributes to the development of chronic pain syndrome, and complicates recovery prognosis [8,11,14].Lumbar compressive radiculopathy (LCR), as a form of vertebrogenic syndrome, is one of the most severe consequences of lumbar spine osteochondrosis. This condition develops due to functional impairment of spinal nerve roots and is characterized by prolonged, intense pain, as well as motor, sensory, and reflex dysfunctions [9,17,18].The aim of the study is to enhance the effectiveness of surgical treatment for lumbar compressive radiculopathy through a prospective clinical and functional evaluation of tubular microdiscectomy and the optimization of tactical and technical approaches to its implementation.
2. Materials and Methods
- As part of the study, data from 120 patients who underwent surgical treatment for lumbar compressive radiculopathy between 2020 and 2023 were analyzed. All patients were divided into two groups:The main group (60 patients), where tubular microdiscectomy was used.Comparison group (60 patients), where discectomy was used according to the W. Caspar method.To assess the effectiveness of treatment, pain intensity was measured using a visual analogue scale (VAS), as well as an assessment of functional status using the Oswestry scale (ODI) in the early postoperative period.
3. Technical Aspects
- We have developed a technique for preserving the ligamentum flavum when performing tubular microdiscectomy, which includes: resection of the vertebral arch, mobilization of the ligamentum flavum from its attachment to the bone structures, its retraction with fixation on a ligature, and then return to its original position after removal of the hernial sequestration. A special feature of the method is its adaptation to the location of the hernial sequestrum:• When the sequestrum is located at the level of the intervertebral disc or when it migrates downward, the caudal edge of the ligamentum flavum is highlighted in the cranial direction while maintaining its attachment in the area of the arch of the overlying vertebra, forming a kind of “flap”.• When the sequestrum migrates upward, the cranial edge of the ligamentum flavum is released in the caudal direction while maintaining its attachment in the area of the arch of the underlying vertebra.This approach allows minimizing damage to the ligamentum flavum while maintaining its integrity and functional properties.The proposed method makes it possible to minimize surgical access, reduce the risk of the formation of gross scar-adhesive changes, reduce traction and intraoperative damage to nerve structures, and also shorten the duration of the rehabilitation period. This approach was successfully used in 60 patients included in the main study group.
4. Results and Discussion
- The postoperative dynamics of pain intensity measured by the VAS scale demonstrated a significant reduction in pain sensations among patients. Statistical analysis revealed both intragroup and intergroup differences. On the first day after surgery, the mean pain intensity score in the study group was 2.7±0.07, while in the control group, this score was higher at 3.8±0.09 (p<0.001), indicating a statistically significant difference in favor of the study group.The trend toward a more pronounced reduction in pain in the study group continued on the second and third days of the hospital stay, which confirms the advantage of the proposed treatment method (see Figure 1).
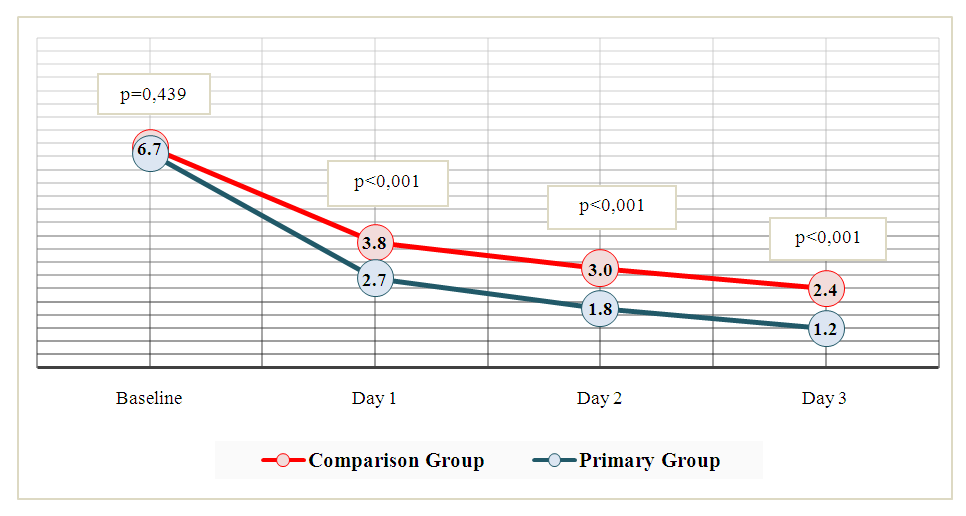 | Figure 1. Trends in Back Pain Intensity Scores on the Visual Analogue Scale (Primary Group n=60, Comparison Group n=60) |
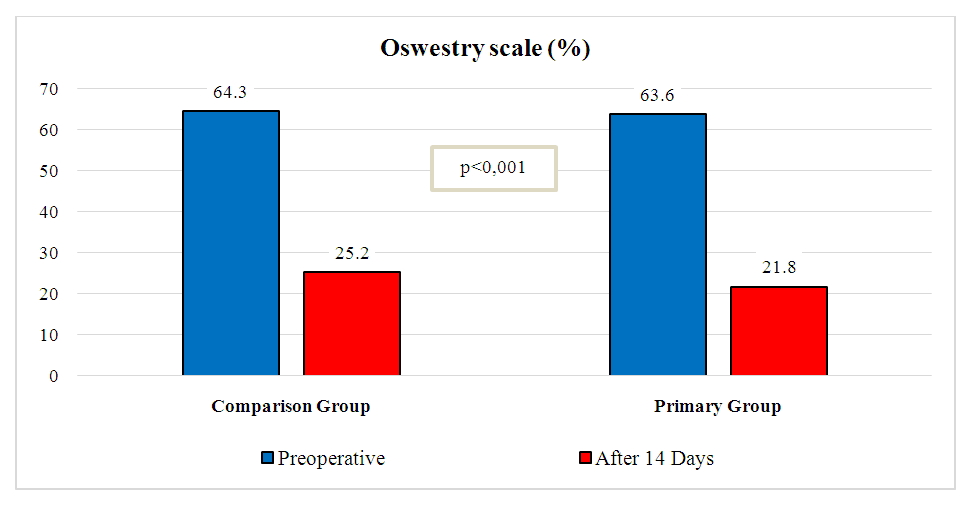 | Figure 2. Dynamics of the Oswestry Disability Index (%) in the Early Perioperative Period: Comparative Analysis (Primary Group, n=60; Comparison Group, n=60) |
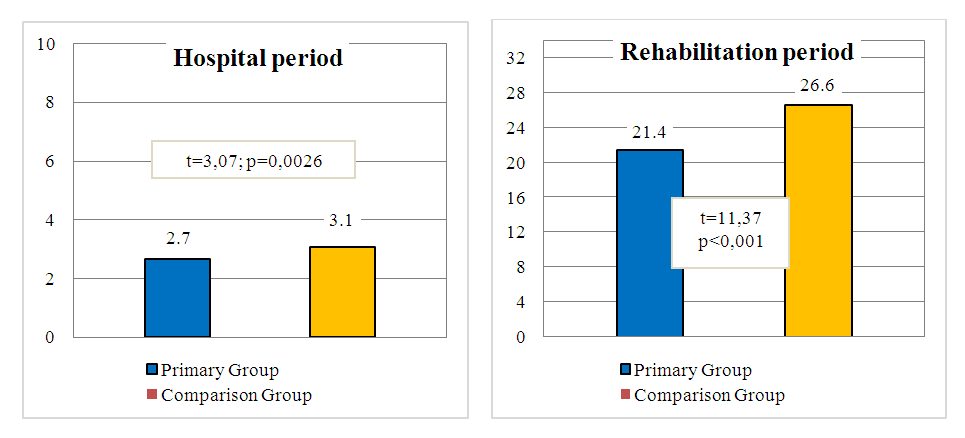 | Figure 3. Average Duration of Hospital Stay and Overall Rehabilitation Periods (in Days) (Primary Group: n=60; Comparison Group: n=60) |
5. Conclusions
- The proposed method of microsurgical treatment for lumbar disc herniation (LDH) involves the use of a tubular microdiscectomy technique with flavoplasty, which minimizes trauma to surrounding tissues, reduces postoperative scarring and pain syndrome, and enhances spinal stability. A comparative analysis of treatment outcomes in patients with LDH demonstrated that the tubular microdiscectomy technique, due to its minimally invasive nature, reduction in the size of the postoperative wound (from 2.6±0.18 cm to 1.7±0.11 cm; p=0.0005), and improved spinal stability, allowed for an enhancement in the functional status of patients. It also led to a significant decrease in pain intensity on the VAS scale (from 3.8±0.09 to 2.7±0.07 points; p<0.001), a reduction in hospital stay duration (from 3.1±0.09 days [range: 2–5] to 2.7±0.09 days [range: 2–4]; p<0.001), and a shortened overall postoperative recovery period until return to work (from 26.6±0.3 to 21.4±0.33 days; p<0.001).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML