-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 128-130
doi:10.5923/j.ajmms.20251501.23
Received: Dec. 26, 2024; Accepted: Jan. 22, 2025; Published: Jan. 24, 2025

Probiotic and Metabiotic Effects on Duodenal Morphology in Individuals with Peptic Ulcer Disease
Umarova G. O., Khamrabaeva F. I.
Centre for the Development of Advanced Professional Qualifications of Medical Workers of the Ministry of Health of the Republic of Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Duodenal ulcer disease remains one of the urgent problems of modern scientific and practical gastroenterology, and a high level of morbidity, disability and life-threatening complications due to this disease remains (Grigorev P.Ya., 2017, Tkachenko E.I. et al., 2015). Modern international recommendations suggest the treatment of Helicobacter pylori (N.r.) generalized stomach and O'IBIIa disease by introducing one of the proton pump inhibitors (PNIs) together with two or three antibacterial drugs. At the same time, the practical use of such therapy schemes is controversial, because, on the one hand, it leads to a decrease in the frequency of exacerbation and recurrence of gastric ulcer disease, and to an improvement in the quality of life of patients, but on the other hand, Nstrains (Ivashkin V.T. et al., 2009), and, accordingly, leads to a decrease in the effectiveness of the main therapy. Therefore, N.r. The formation of resistance to antibiotics is an inevitable phenomenon, which is difficult to prevent. This in turn encourages the creation of new antibiotics and the development of new treatment regimens. In such circumstances, N.r. The widespread use of antibacterial agents as the main method of treatment for diseases associated with There was a direct correlation between the development of these side effects within a short time after the initiation of eradication therapy. Thus, there is a need to improve the standard regimens of antihelicobacter therapy and supplement them with drugs, whose effect is aimed at preventing and correcting dysbiotic diseases and mobilizing the metabolic potential of normal intestinal microflora.
Keywords: Ulcer disease, Morphology, Practical gastroenterology, Helicobacter pylori infection
Cite this paper: Umarova G. O., Khamrabaeva F. I., Probiotic and Metabiotic Effects on Duodenal Morphology in Individuals with Peptic Ulcer Disease, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 128-130. doi: 10.5923/j.ajmms.20251501.23.
1. The Study's Goal
- The study's goal was to look at how probiotic and metabiotic treatment affected the mucous membrane around the borders of duodenal ulcers.
2. Material and Methodology
- The research included 60 individuals with intestinal dysbiosis (ID). There were 29 ladies and 31 guys. They were ages 18 to 65. All patients were diagnosed with ID. Patients were placed into three groups of 20 patients each: Patients who got Esomeprazole on 20/2/14 20, the second group got Amoxacillin 1000/2/14, Rifaximin 600/2/14, Bismuth tripotassium dicitrate 240/2/14, and Saccharomyces boulardii 2 drops/2/14, while patients who received Esomeprazole 20/2/14 The third group included 20, Amoxacillin 1000/2/14, Rifaximin, Bismuth tripotassium dicitrate 240/2/14, and Actoflor with 1 pipette/2/14. Eradication therapy was developed in accordance with the Maastricht VI consensus recommendations for the treatment of Helicobacter pylori infection (2022) [1].After endoscopic inspection and collection of material for histological evaluation, a detailed assessment of the general histological structure of the mucous membrane of the margins of duodenal ulcers was performed in 51 patients with ulcer defect localisation in the duodenum. The histological preparations were assessed in line with M. Dixon's (2006) current categorisation of chronic gastritis, as well as the suggestions of L.I. Aruin (2008) and V.Yu. Golofeevsky (2004) [2].When analysing histological preparations, the major focus was on the condition of the epithelium and the height of the villi and crypts (enterocytes, goblet cells), dystrophy, atrophy, and stomach metaplasia foci, as well as the condition of Brunner's glands, were evaluated [3].Furthermore, the stroma's state (the severity of neutrophilic, eosinophilic, lymphocytic, and plasmacytic infiltration) was evaluated qualitatively and semi-quantitatively (in ten fields of view), which is known to be directly involved in immune regulation, epithelial cell regeneration and differentiation, immune protection mechanisms, and the formation of acute and chronic inflammation [4].The main morphological signs in patients with peptic ulcers localised in the duodenal bulb were pronounced dystrophy of the enterocytes of the villi, a decrease in the number of goblet cells in the villi and crypts, a decrease in the height of the villi, and areas of gastric metaplasia of the villi [5].A link between morphological alterations and Helicobacter pylori infection was also found in patients. Thus, moderate and severe dystrophy occurred substantially more frequently in the presence of Helicobacter pylori infection (44.7% of patients). In the absence of Helicobacter pylori infection, only 8 individuals had epithelial dystrophy, and the degree of the dystrophic alterations was low. However, there were no significant variations in the prevalence of dystrophy and atrophy of the villi along the borders of duodenal bulb ulcers among the patient groups studied [6].
3. Result
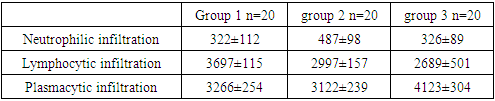
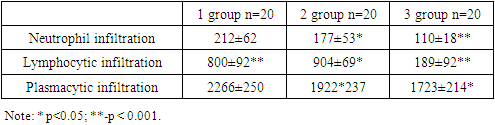
- As a result, the known facts that dystrophy and atrophy in the mucous membrane of the duodenal bulb are inherent morphological aspects of duodenal ulcers, particularly at its margins, have been verified. Apparently, this is why no fundamental link between these alterations and Helicobacter pylori infection was discovered. Gastric metaplasia of villous enterocytes was seen in 38 of 60 patients, however the prevalence of Helicobacter pylori infection discovered in this case had only a little tendency to be greater than in patients without gastric metaplasia. As a result, one should concur with the viewpoint that gastric metaplasia might serve as a compensatory morphological element in situations of bulbar mucous membrane inflammation and dystrophy in individuals with duodenal ulcers.In this context, the assessment findings are of particular relevance. stroma of the mucous membrane of the borders of the ulcers of the duodenal bulb and morphometry, inflammatory infiltration in the investigated individuals previously treatment (Table 1) and after treatment (Table 2) [7,8,9].
|
|
4. Discussion and Conclusions
- At the same time, the findings collected allow us to conclude that using components for colonic microbiome correction in treatment regimens results in a more marked beneficial change in the cellular composition of the duodenal mucosa. The density of neutrophilic (from 487±98-326±89 to 177±53-110±18, respectively, in the 2nd and 3rd groups, p<0.001) and lymphocytic (from 2997±157-2689±501 to 904±69*- 189±92, respectively, in the 2nd and 3rd groups, p<0.001) infiltration decreased significantly, indicating a decrease in the activity of inflammatory and immunoinflammatory processes. Including a metabiotic in eradication therapy considerably lowers plasma cell infiltration in the third group of patients (from 4123±304 to 1723±214, p<0.05).Morphological alterations such as microcirculation abnormalities (vasodilation, sludge, leukopedesis, and erythrocytopedesis) and mucous membrane stromal oedema are directly connected to inflammatory infiltration density. It is noteworthy that in the second and third groups, these alterations were nearly totally stopped during the control histological test. Thus, therapeutic regimens that include probiotics and metabiotics, including Saccharomyces boulardii and Actoflor C, by their morphological The effectiveness rates greatly outperformed the similarly targeted effects of traditional eradication treatment regimens, which included PPIs, bismuth potassium dicitrate, and two antibiotics.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML