-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 96-100
doi:10.5923/j.ajmms.20251501.17
Received: Dec. 18, 2024; Accepted: Jan. 16, 2025; Published: Jan. 21, 2025

Assessment of the Morphological Picture of Bone Marrow and Peripheral Blood in the Early Days after Allogeneic Bone Marrow Transplantation
Ozoda Umarkulovna Achilova1, Kayumov Abdurakhman Abdumavlyanovich2, Khudaibergenov Zafar Safaralievich3, Gulchehra Zukhriddinovna Mahamadalieva4, Mukhammadiev Sardor Bakhtiyorovich5, Tashtemirov Farhod Ravshanovich5, Orazkhanov Doshan Orazhkanovich5
1PhD, Hematologist of the RSSPMCH Transplantation Department, Republican Specialized Scientific and Practical Medical Center for Hematology Ministry of Health of Uzbekistan
2DSc, Chief Physician of RSSPMCH, Republican Specialized Scientific and Practical Medical Center for Hematology Ministry of Health of Uzbekistan
3Pathologist of the RSSMPCH, Republican Specialized Scientific and Practical Medical Center for Hematology Ministry of Health of Uzbekistan
4PhD, Head of the RSSPMCH Transplantation Department, Republican Specialized Scientific and Practical Medical Center for Hematology Ministry of Health of Uzbekistan
5Hematologist of the RSSPMCH Transplantation Department, Republican Specialized Scientific and Practical Medical Center for Hematology Ministry of Health of Uzbekistan
Correspondence to: Ozoda Umarkulovna Achilova, PhD, Hematologist of the RSSPMCH Transplantation Department, Republican Specialized Scientific and Practical Medical Center for Hematology Ministry of Health of Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Hemablastosis is one of the most acute scientific problem in medicine. Bone marrow transplantation is currently a reliable method of tumor removal in leukemia. Although the story of transplantation is more than 50 years, the issues of bone marrow restore after allogeneic and autologous transplantation want in addition analyzing, which is the relevance of this topic. Objective: To observe the morphological picture of the bone marrow based on the results of ilium biopsies in patients after allogeneic bone marrow transplantation in the early post-transplantation period. Materials and Methods: A morphological evaluation of bone marrow biopsies from 30 patients after autologous bone marrow transplantation performed at RSSPMCH from 2023 to 2024. Results: From the facts obtained, it is obvious that after bone marrow transplantation, the cellularity of the bone marrow in none of the patients reached normal values even through the 30th day. In 22 (74%) patients, the bone marrow riches normal cellularity by day 60. In 8 (26%) cases, diagnosed hypocellularity in the bone marrow. The ratio of adipose bone marrow to myelokaryocytes was 0.5:0.9, indicating hematopoietic hypoplasia. A poor cellularity was persisted in 1/3 of patients within 60 days, which manifested as triple cytopenia in 7 (23%) patients. Conclusion: Based on these findings, we finish that despite highly stable peripheral blood values, it's far still too early to talk about сompletly engraftment of bone marrow stem cells, even via day 60.
Keywords: Bone marrow allotransplantation, Stem cells, Trepanobiopsy, Hematopoietic restoration
Cite this paper: Ozoda Umarkulovna Achilova, Kayumov Abdurakhman Abdumavlyanovich, Khudaibergenov Zafar Safaralievich, Gulchehra Zukhriddinovna Mahamadalieva, Mukhammadiev Sardor Bakhtiyorovich, Tashtemirov Farhod Ravshanovich, Orazkhanov Doshan Orazhkanovich, Assessment of the Morphological Picture of Bone Marrow and Peripheral Blood in the Early Days after Allogeneic Bone Marrow Transplantation, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 96-100. doi: 10.5923/j.ajmms.20251501.17.
1. Relevance
- Hemablastosis is one of the most acute medical issues these days. The development of pharmaceuticals and targeted drugs have progressed the results of chemotherapy. However, bone marrow transplantation (BMT) stays a reliable method for eradicating the tumor clone in leukemia [11]. Developing techniques in medicine, especially the appearance of the cells separators, have made bone marrow transplantations much less traumatic because of using cells from peripheral blood. High-dose chemotherapy accompanied by stem cell transplantation has made patients relapse-free survival upper than 30% [2]. However, the main results of treatment depends of the type of leukemia, on the timing of transplantation and the degree of the ailment. Molecular genetic analysis is also important. Cytogenetic strategies now play a unique role in predicting the final results of the disorder [1]. Allogeneic bone marrow transplantation surpasses the results received with polychemotherapy and using targeted drugs. The disease-free survival in patients who received allogeneic bone marrow transplantation during complete remission is 45-75%, and they relapse no greater than 15%. Therefore, in all patients with a match donor (HLA-equal), allogeneic bone marrow transplantation is an indisputable recommendation [2]. However, finding HLA-match donors is a hard assignment, and only 30% of patients may also have a related, appropriate sibling donor. In cases when no donor, patients can undergo myeloablative chemotherapy and support recovering hematopoiesis with an autologous transplant [3,5]. And in these cases, there may be no graft-versus-leukemia effect, and there is additionally a threat of contaminating the stem cells with tumor clones, which increases the likelihood of relaps of patients [7].Although the history of transplantation is more than 50 years, the issues of bone marrow repair after allogeneic and autologous transplantation stay poorly understood [8]. It is so few studies dedicated on the timing of the restoration of bone morrow parameters after transplantation and the morphological patterns of hematopoiesis. A limited number of publications about the character of hematopoiesis after allogeneic bone marrow transplantation based on bone trepan biopsies [5]. At the same time, it is obvious that bone marrow morphology data is needed to compare the picture of peripheral blood, and it is important to evaluate not only the number but also the quality of cells in the bone marrow [10]. The comparison of peripheral blood parameters and bone marrow cell morphology determines the relevance of this work.Study Aim: to study the morphological picture of bone marrow according to trepan biopsies in patients after allogeneic bone marrow transplantation during the early period.
2. Materials and Methods
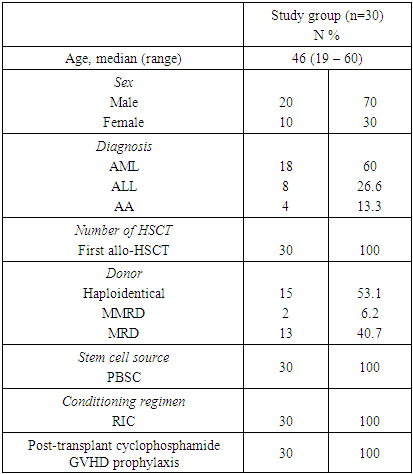
- The study included 30 patients with acute leukemia who were treated at the Republican Specialized Scientific and Practical Medical Center of Hematology in Uzbekistan (RSSPMCH) in the transplantation department from 2023 to 2024. 30 bioptates were analyzed on day +30 and on day +60 after alloBMT. Trepan biopsy was performed under local anesthesia from the posterior spine of the ilium. The staining of the preparations was carried out with hematoxylin-eosin, peripheral blood smears - by Romanovsky - Giemse. Statistical processing of the results was carried out in the Statistica 10.0 program for Microsoft. Conditioning before bone marrow transplantation was performed according to the low-intensity regime (RIC) FLUMEL protocol, which consisted of fludarabine 30 mg/m2 for 6 days, melfolan 140 mg/m2 on 2 consecutive days -3 and -2 of alloBMT. In cases with a 100% HLA-identical donor, chemoprophylaxis of the graft-versus-host reaction (GVHD) was performed by administration on +3 and +4 days of Cyclophosphamide at a dose of 25 mg/m2 simultaneously with the antidote Uromethoxane (mesna) in a ratio of 1:1.5. In haploidentical bone marrow transplantation (when HLA match is less than 9:10, but not less than 5:10), GVHD prevention began 15 days before transplantation. On day 15, the administration of Mycophenolate mofetil 30 mg/kg (but not more than 2 g/day) and Rituximab at a dose of 375mg/ m2 began. Cyclophosphamide was also administered on the same days and at the same dose as with alloBMT with a full match donor. On day 5, in both cases, Cyclosporine A was added intravenously at a dose of 3 mg/kg, then this drug continued until day 100 after alloBMT. All patients 30 (100%) in the study received native (non-frozen) peripheral blood stem cells from related donors. The average cell count of the transfused graft was 6.03±1.5*109/kg of cells (4.5-7.45*109/kg) p<0.0001.
3. Results
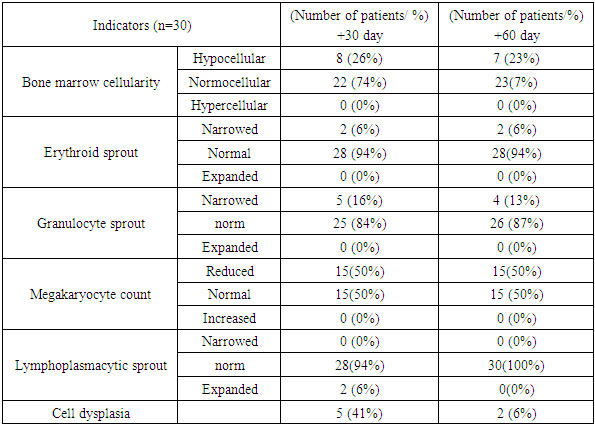
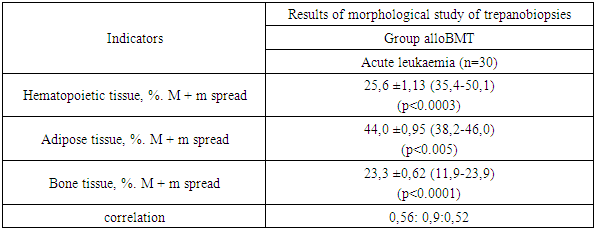
- Of the 30 patients who underwent allogeneic bone marrow transplantation (alloBMT) from related donors, 60 trepan biopsies were performed and 60 were analyzed. A biopsy of the ilium was performed at +30 and +60 days after alloBMT. The group consisted of patients with AML- 18(60%), ALL- 8(26.6%) and aplastic anemia 4 (13.3%). The average age of the patients was 46 (19-60), gender separation was male -20 (70%), female – 10 (30%). All patients in the study group received their first transplant – 30 (100%). Peripheral blood was used as a source of stem cells in all 30 (100%) patients. At the same time, there were 13(40.7%) full matches related, haploidentical 15(53.1%) and partial match 2(6.2%) donors. The characteristics of the patients are shown in Table 1.
|
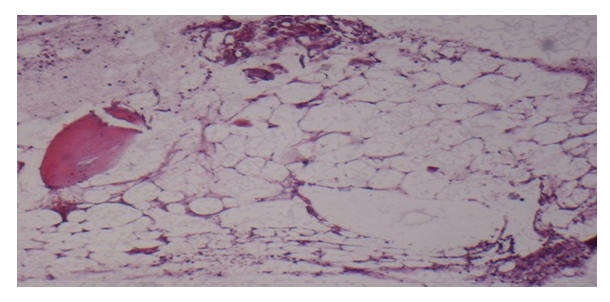 | Figure 1. Histological picture of bone morrow at +30 day after allogeneic bone marrow transplantation |
|
|
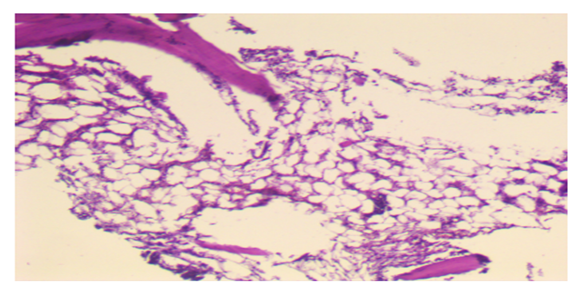 | Figure 2. Histological picture of bone morrow at +60 days after allogeneic bone marrow transplantation |
|
4. Conclusions
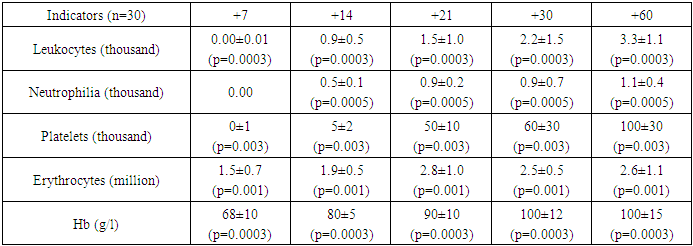
- As can be seen from the study, as early as day 21, the hemogram indicators are approaching the values that allow the patient to dispense with replacement therapy with blood components. During this period, patients with peripheral blood tests have stable indicators and have often already been discharged from the hospital. With a more detailed analysis of bone tissue, 1/3 of patients after alloBMT had cell dysplasticity on +30 and even on +60 days after BMT. Not all patients from the observation group had graft engraftment. Bone marrow hypocellularity was diagnosed in 7 (23%) patients, which manifested itself in the peripheral blood of 4 of them as 3 line cytopenia, 3 like isolated red cell insufficiency. From all this, it can be concluded that despite the relatively stable peripheral blood levels, even at +60 days, it is still too early to talk about complete bone marrow repair, and it is advisable to leave patients under outpatient supervision.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML