-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 79-87
doi:10.5923/j.ajmms.20251501.14
Received: Dec. 22, 2024; Accepted: Jan. 15, 2025; Published: Jan. 18, 2025

Evaluation of the Corrective Effect of Laparoscopic Longitudinal Gastrectomy on Metabolic Parameters and Concomitant Diseases in Patients with Morbid Obesity
Murоdov Alijon Salimovich
PhD, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Murоdov Alijon Salimovich, PhD, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

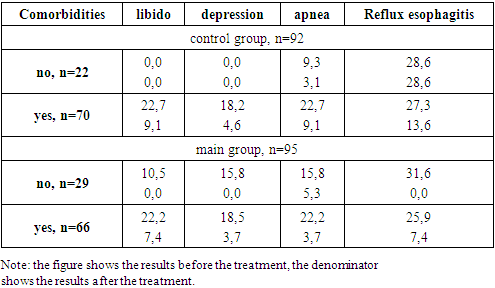
To study the corrective effect of laparoscopic longitudinal gastric resection (LLGR) on obesity-related metabolic disorders in morbidly obese patients. This scientific work is based on the results of a comprehensive examination and treatment of 187 patients treated for morbid obesity in our clinical bases from 2021 to 2023. Analysis of comorbidities in the compared groups showed that 64% of the comparison groups had metabolic disorders. The majority of these patients were patients with 3rd degree of obesity. Positive changes in lipidogram analysis were observed in patients after LOBR procedure. Also, when hemostasis indicators were studied, convincing positive changes were observed in the 1st and 3rd stages of coagulation hemostasis. In patients with chronic obesity, our recommended modification of LOBR increased cardio esophageal and gastric stapler line strength, eliminating the 2.2% stapler line failure observed in our control group in our main cohort. It also led to a reduction in gastroesophageal reflux disease symptoms from 14% to 6.1%. In conclusion, these pathological changes are closely related to obesity, and the elimination of obesity led to the elimination of these metabolic disturbances.
Keywords: Metabolic syndrome, Morbid obesity, Bariatric surgery, Concomitant diseases, Laparoscopic longitudinal gastric resection
Cite this paper: Murоdov Alijon Salimovich, Evaluation of the Corrective Effect of Laparoscopic Longitudinal Gastrectomy on Metabolic Parameters and Concomitant Diseases in Patients with Morbid Obesity, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 79-87. doi: 10.5923/j.ajmms.20251501.14.
1. Introduction
- Obesity is a chronic metabolic disease, manifested by excessive development of adipose tissue, progressing in its natural course, having a certain range of complications and having a high probability of relapse after completion of treatment [2]. The disease depends on the interaction of several factors, such as genetic, endocrine, metabolic, environmental (social and cultural), behavioral and psychological components [25]. Recently, obesity has become one of the most important public health problems worldwide in all age groups [23]. Obesity is the most dangerous and serious risk factor for the life of patients. More than 1 billion adults are overweight and at least 300 million people are obese (BMI over 30 kg/m2) [22]. Morbid obesity is a condition characterized by excessive fat accumulation in the body, defined as BMI ≥40 kg/m2 or BMI ≥35 kg/m2, and the presence of serious obesity-related complications [30,14]. The disease depends on the interaction of several factors, such as genetic, endocrine, metabolic, environmental (social and cultural), behavioral and psychological components [16]. It has been scientifically proven that people with certain degrees of obesity (I, II or III) are at higher risk of obesity-related diseases, comorbidities, lower quality of life and increased mortality to a greater extent than people in the normal BMI range (18, 5–24,9) [4,27].Morbid obesity and metabolic syndrome is a worldwide health problem that affects children, adolescents and adults and is accompanied by comorbidities such as hypertension, dyslipidemia, type 2 diabetes, cancer, osteoarthritis and sleep apnea [11,21]. Obesity, according to expert estimates, leads to a 4-fold increase in the risk of cardiovascular mortality and 2-fold increase in mortality due to cancer [13,17].We know that prevention is the long-term solution to this vital public health problem, but prevention may not always be successful and sustainable. In addition, current conservative therapies, including non-drug and drug treatments, fall far short of the desired success in long-term weight loss [1,28].Long-term results of conservative treatment of obesity remain unsatisfactory, and today the most effective and reliable methods of treating morbid obesity are surgical, both in terms of the achieved reduction in body weight and in the improvement of metabolic parameters [6,7]. Many authors have scientifically and clinically proven that bariatric surgery in adult morbidly obese patients may be the most appropriate treatment option for sustaining weight loss and obesity-related management [29].Bariatric surgery is recommended in patients with morbid obesity and a combination of the above comorbidities [8,9,24,26]. Recently, the most frequent bariatric surgeries are laparoscopic sleeve gastrectomy (LSG), mini gastric bypass (MGB), Roux-en-Y gastric bypass (RYGB), and duodenal switch (DS). Laparoscopic sleeve gastrectomy can give results such as MGB, RYGB and DS without malabsorption problems [2,10,19]. Sleeve gastrectomy is an important bariatric operation used in the treatment of patients with morbid obesity [31]. Sleeve gastrectomy is a new, safe and effective method of surgical treatment of obesity with higher survival rates and low patient complication rates [3,28]. Initially, this operation was introduced into clinical practice as part of duodenal switch biliopancreatic diversion [12]. Sleeve gastrectomy is currently widely performed as an independent laparoscopic operation [15]. Since its first introduction in 2004 as a stand-alone laparoscopic procedure in bariatric surgery, LSG has proven to be effective in sustained, long-term weight loss and improvement in comorbidities [18].Purpose of the study: Improvement of operative treatment results in patients with morbid obesity through the corrective effect of modified laparoscopic longitudinal gastric resection on existing metabolic disorders and comorbidities.
2. Materials and Methods
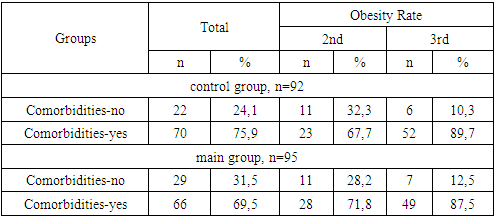
- This scientific work is based on the results of examination and treatment of 187 patients with morbid obesity (MO), who were treated at the clinical bases of the Department of Surgical Diseases of Family Medicine of the Tashkent Medical Academy from 2021 to 2023. Depending on the treatment, the patients were conditionally divided into 2 groups: the 1st (control group) included 92 patients who underwent the traditional method of laparoscopic longitudinal gastrectomy; in group 2 (main group) there were 95 patients who underwent our proposed modified laparoscopic longitudinal gastrectomy [20,30]. When the distribution of the patients of our research group by age was studied, it was found that the main group of patients are young and middle-aged women. The average age of patients was 36±0.92 years in the control group, 34±0.7 years in the main group. 81.8% of patients aged 18 to 44, 15.5% from 45 to 59 years, 2.7% from 60 to 74 years. The analysis shows that the patients who underwent surgery are mostly under 45 years old, which is considered to be the working age (Fig. 1).
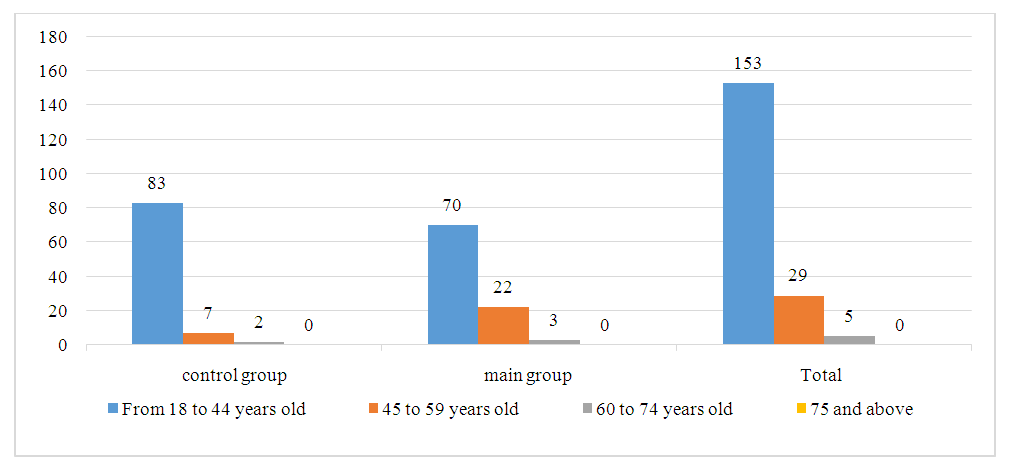 | Figure 1. Distribution of patients by age |
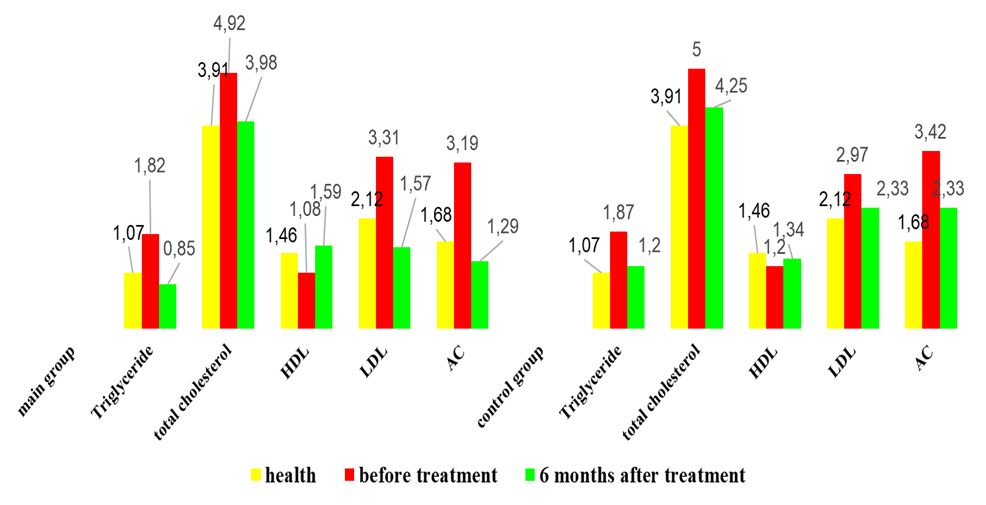 | Figure 2. Serum lipid metabolism indicators after LOBR surgery in control groups, M±m |
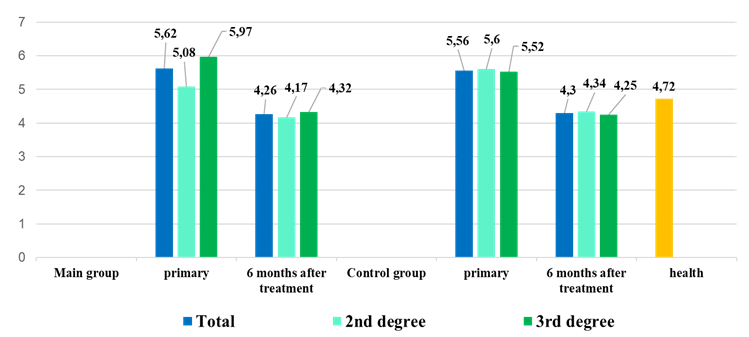 | Figure 3. Indicators of carbohydrate metabolism in blood serum after LOBR surgery in control groups, M±m |
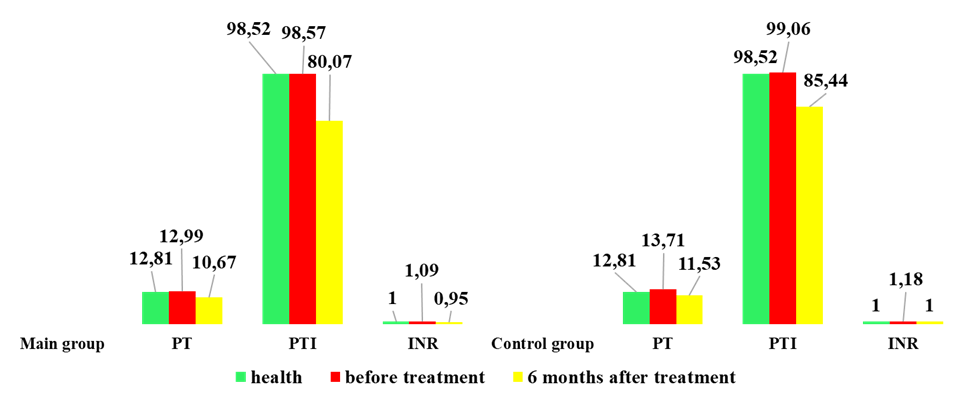 | Figure 4. Changes in hemostasis indicators in our patients of the comparison group |
|
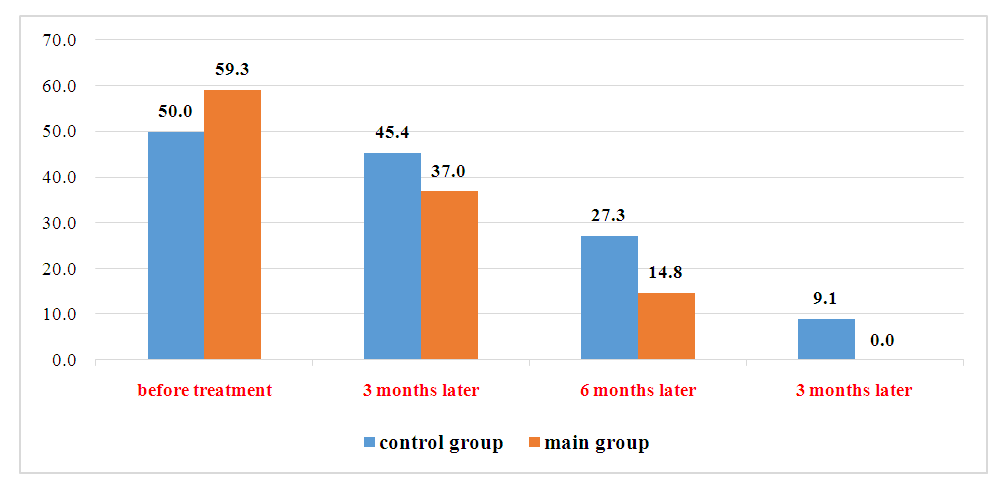 | Figure 5. Dynamic changes in the incidence of concomitant arterial hypertension with morbid obesity in the control and main groups 3, 6 and 12 months after surgery |
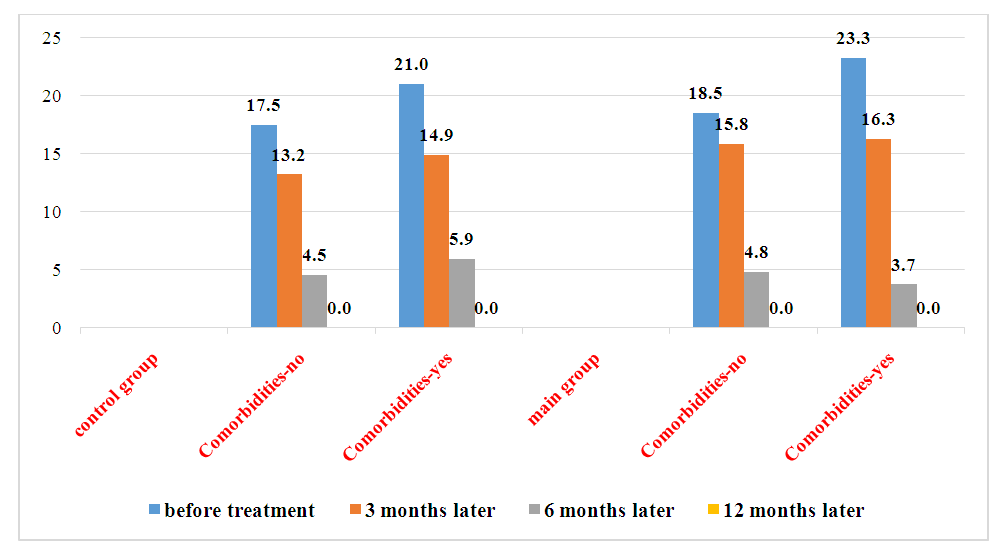 | Figure 6. Dynamic changes in the incidence of arthralgia associated with morbid obesity in control and main groups 3, 6, and 12 months after surgery |
|
3. Conclusions
- 1. After 6 months of bariatric treatment, total cholesterol, cholesterol in LDLs, atherogenic coefficient, and especially triglycerides decreased, cholesterol increased in HDLs, and such positive changes were clearly identified in the main group of patients. If hypo-a-lipoproteinemia, type IIb of dyslipidemia and type IV of dyslipidemia were not detected after the proposed method, hypo-a-lipoproteinemia was not detected in the control group, type IIb of dyslipidemia remained in 8.9%, and type IV of dyslipidemia remained in 2.2% of patients left. 2. As a result of the corrective effect of gastric longitudinal resection on existing metabolic indicators in patients suffering from morbid obesity, it improves the course of patients in the early period and concomitant diseases, and has a positive effect on the clinical course of not only prediabetes, but also diabetes. 3. Significant statistically significant positive changes were observed in the 1st and 3rd-stages of coagulation hemostasis after longitudinal resection of the stomach compared to the hemostasis parameters of the control group. Surgery performed in the main group showed that the treatment was effective regardless of the degree of obesity in patients.4. In morbid obesity, the combination of concomitant diseases (arterial hypertension, reflux esophagitis, gallstone disease and chronic bronchitis) leads to a high incidence of severe obesity, a 2-3 times increase in the development of pathognomic symptoms, and the formation of a "dangerous circulation".5. In morbid obesity, the addition of concomitant diseases leads to further deepening of metabolic disorders, increased changes in blood vessels and the development of serious complications for the patient’s life.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML