-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 43-46
doi:10.5923/j.ajmms.20251501.08
Received: Dec. 13, 2024; Accepted: Dec. 30, 2024; Published: Jan. 16, 2025

Clinical Significance of Predictors of the Risk of Recurrence of Gastroduodenal Ulcer Bleeding
Usmonov A. Kh., Askarov P. A., Kurbaniyazov Z. B.
Samarkand State Medical University, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study included 120 clinical observations of patients with GDBUE, in whom EG methods were used to stop bleeding or prevent its recurrence. When analyzing this clinical material, RK was noted in 37 observations of patients with GDBUE, which amounted to 30.8% of their total number. The most significant prognostic factors for the risk of recurrence of gastroduodenal bleeding of ulcerative etiology are: a) bleeding intensity according to J.A. Forrest, b) antisecretory therapy, c) patient's age, d) blood hemoglobin level, d) ulcer localization features, e) ulcer size, g) presence of visible vessel in ulcer, h) nature of concomitant diseases, i) intake of nonsteroidal anti-inflammatory drugs, j) heart rate.
Keywords: Gastroduodenal bleeding of ulcerative etiology, Recurrence of bleeding, Risk predictors
Cite this paper: Usmonov A. Kh., Askarov P. A., Kurbaniyazov Z. B., Clinical Significance of Predictors of the Risk of Recurrence of Gastroduodenal Ulcer Bleeding, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 43-46. doi: 10.5923/j.ajmms.20251501.08.
Article Outline
1. Relevance
- The problem of gastroduodenal bleeding - a formidable, often fatal complication of ulcerative lesions continues to be one of the most urgent, still unresolved problems of urgent surgery. Gastroduodenal bleeding of ulcerative etiology (GDBUE) is characterized by a high frequency of development, it accounts for the majority (> 60%) of all bleeding from sources located in the upper gastrointestinal tract (GIT), moreover, in recent years there has been a tendency towards an increase in the frequency of GDBUE. To this day, the results of treatment of patients with GDBUE do not satisfy the surgical community. According to data from numerous studies, the levels of overall mortality among patients with GDBUE are within 10-17%, postoperative mortality - 4.8-35%, significantly increasing with recurrent bleeding (RB) - up to 30-45% and 30-80%, respectively.In the vast majority of cases, GDBUE develops in elderly and senile patients, characterized by polymorbidity and high surgical and anesthetic risk (SAR) [1], which often dictates the desire for maximum conservatism in the implementation of therapeutic measures. In the medical literature devoted to the problem of GDBUE, a significant place is devoted to the discussion of issues related to RK and measures to prevent them. According to the majority of domestic and foreign authors, RK is a factor that significantly exacerbates the relevance of the problem of GDBUE, being the main cause of unsatisfactory treatment results and high mortality rates, especially among elderly and senile patients. RK is an extremely unfavorable complication that develops in 10-30% of cases after successful primary endoscopic hemostasis (PEH), according to some data, RK is associated with a fivefold increase in mortality rates. The problem of predicting the probability of RC and reasoned determination of indications for surgical intervention remains unsolved. Many authors speak about the need to develop a new method for predicting recurrence of ulcerative bleeding, due to the lack of systems with high accuracy of prediction.Purpose of the study. To identify risk factors for the development of recurrence of bleeding in patients with gastroduodenal bleeding of ulcerative etiology.
2. Material and Methods of the Study
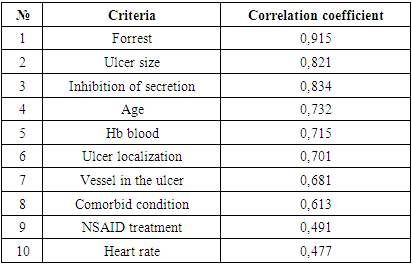
- The study included 120 clinical observations of patients with GDBUE, in whom EG methods were used to stop bleeding or prevent its recurrence. When analyzing the gender composition among patients with GDBUE, there were more men than women - 87 (72.5%) and 33 (27.5%), respectively (p < 0.01). The ratio of men and women = 2.4: 1. The age of patients ranged from 18 to 85 years, while the overall average age was 56.1 ± 14.4 years. The average age of women was significantly higher than that of men, respectively 61.2 ± 11.4 and 49.5 ± 15.2 years (p < 0.05). The most numerous group was represented by elderly people, who made up almost 1/3 (30.4%) of the total number of patients. More than half (53.1%) of patients with GDBUE were aged ≥ 60 years.According to our study, in 67 (55.8%) patients the source of ulcerative bleeding was localized in the duodenum, in 51 (42.5%) patients – in the stomach, and in 2 (1.7%) patients – in the gastroenteroanastomosis.The most common cause of bleeding were acute ulcers of various etiologies – 74 cases, accounting for 61.7% of the total number of observations. The incidence of bleeding due to complicated PU was 38.3% (in 46 patients). The same group included 11 patients with callous ulcers, the proportion of which was 9.2%.During the primary EGDS, one ulcer was detected in 74 (61.6%) patients with GDBUE [2], two in 18 (15.0%) patients, and three or more in 28 (23.4%) patients. Multiple lesions were usually detected in acute EUP.During EGDS, the ulcer diameter was measured in all patients, and it varied from 0.3 to 5.0 cm. The most common ulcers were those with a diameter of 0.6 to 1.0 cm (45.0%).During the analysis of this clinical material, RC was noted in 37 observations of patients with GDBUE, which amounted to 30.8% of their total number: the fact of RC was established in almost every third observation, and its development was noted on average within the first 2 days after a successful EG. In 7 (18.9%) of 37 patients, the fact of repeated RC was established during their stay in the hospital. The signs allowing to establish the development of RC were clinical, laboratory and endoscopic criteria. In 9 (24.3%) of 37 cases of RC, a fatal outcome subsequently developed. It follows that in almost every fourth observation of patients with GDBUE, RC developed, in turn, every third case of RC ended in a fatal outcome. All this clearly demonstrates the dominant role of RC in the unfavorable outcome of treatment of patients with GDBUE.In 23 (62.1%) cases, ulcers with recurrent bleeding were located in the duodenum, and only in 14 (37.9%) cases in the stomach (p<0.01). Most often (in 20 cases – 54.0% of the total number of cases), UC developed from acute ulcers, and in the remaining 17 (46.0%) cases, UC developed from chronic ulcers caused by peptic ulcer disease. When comparing the frequency of UC development depending on the nature of bleeding ulcers (acute or chronic), the differences are insignificant (p>0.05). Of the acute ulcers localized in the duodenum and stomach, UC development was noted in 10 and 11 cases, respectively (p>0.05), and in cases of chronic ulcers – in 11 and 5 cases, respectively (p<0.01). Thus, most often, RC developed from chronic ulcers of duodenal localization [4].Among the patients who developed RC, men predominated - 25 (67.5%) versus 12 (32.5%) women (p<0.01), this ratio reflects the gender structure (m/f) of all clinical material underlying this study (67.5% and 32.5%, respectively).In order to identify factors associated with a high risk of developing gastrointestinal bleeding, an analysis of clinical material was performed according to the following criteria: gender, age, time from the onset of gastrointestinal bleeding, history of ulcerative colitis, history of taking NSAIDs and anticoagulants, heart rate, blood pressure, severity of bleeding, timing of primary therapeutic and diagnostic endoscopy, nature of ulcerative lesion, bleeding intensity according to Forrest, localization (wall, level), quantity, size of ulcer, presence of periulcerous infiltration and visible vessel in the ulcer bottom, type of EG, number of attempts at thermocoagulation EG, hemoglobin level, hematocrit, erythrocytes, blood platelets, indicators of the state of the blood coagulation system, dosage and nature of administration of drugs used for antisecretory and hemostatic therapy, volume and type of infusion-transfusion therapy, nature and severity of concomitant pathology, degree of AAR, etc. The reliability of the influence was assessed by statistical processing. All these criteria for the development of RC using multivariate [3] statistical analysis methods (discriminant analysis and logistic regression) were used to select the most prognostically significant high-risk factors (p<0.05) associated with a high probability of developing RC, which are presented in Table 1.
|
3. Results and Their Discussion
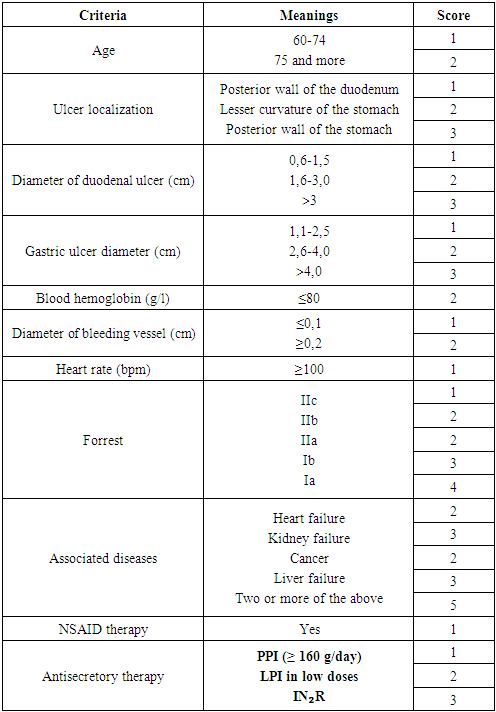
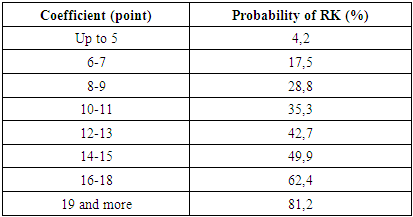
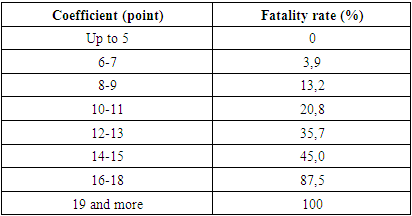
- These criteria are relatively independent of each other. As a result of a detailed consideration of the nature of the distribution of each criterion depending on the fact of development of RK and the correlation coefficient (r), we assigned each criterion the maximum quantitative rank (score) of the risk of RK, which was equal to the number of gradations (at p < 0.05) of this criterion. But, depending on the significance of gradation distributions in the development of RK, the values of the awarded points changed. Thus, we developed of scale for predicting the probability of recurrent bleeding SPPRB, consisting of different gradations of 10 predictors of high risk of developing RK (Table 2).
|
|
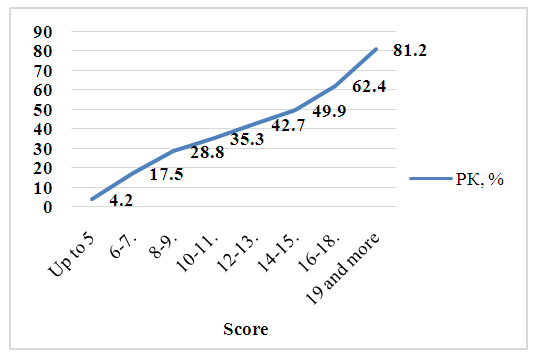 | Figure 1. Probability of developing RC depending on the scoring coefficient |
|
4. Conclusions
- 1. The most significant prognostic factors for the risk of recurrent gastroduodenal bleeding of ulcerative etiology are: a) the intensity of bleeding according to J.A. Forrest, b) the antisecretory therapy, c) the patient's age, d) the value of blood hemoglobin, d) features of the localization of the ulcer, e) the size of the ulcer, g) the presence of a visible vessel in the ulcer, h) the nature of concomitant diseases, i) taking non-steroidal anti-inflammatory drugs, j) heart rate. 2. The developed scale for predicting the probability of recurrent bleeding (SPPRB), which objectively stratifies patients by the risk of recurrent bleeding, allows for a reduction in treatment time in patients with a low risk of recurrent bleeding and, accordingly, the economic costs of unnecessary treatment and diagnostic measures, and, conversely, for patients with a high risk of recurrent bleeding, to carry out the entire range of necessary treatment and diagnostic measures in a timely manner.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML