-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 38-42
doi:10.5923/j.ajmms.20251501.07
Received: Dec. 13, 2024; Accepted: Dec. 29, 2024; Published: Jan. 16, 2025

Comprehensive Therapy of Miscarriage Based on the Study of Immunohistochemical Markers of Inflammation and Receptiveness of the Endometrium
Matrizaeva Gulnara Djumaniyazovna1, Ikhtiyarova Gulchekhra Akmalovna2
1Candidate of Medical Sciences, Associate Professor, Head of the Department of Obstetrics and Gynecology, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan
2Doctor of Medical Sciences, Professor, Head of the Department of Obstetrics and Gynecology, Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Matrizaeva Gulnara Djumaniyazovna, Candidate of Medical Sciences, Associate Professor, Head of the Department of Obstetrics and Gynecology, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Miscarriage is defined as the spontaneous loss of pregnancy before the twenty-second week. About 15-25% of pregnancies end in spontaneous abortion, although abortion statistics vary greatly depending on the country and the timeliness of pregnancy diagnosis. Pregnancy loss before the 12th week (non-viable pregnancy, spontaneous abortion) accounts for 80% of all early reproductive losses. Miscarriages that occur before the thirteenth week of pregnancy are considered early abortions, the risk of miscarriage decreases from the fourteenth week. Between the third and sixth weeks, the probability of miscarriage is about 75%. Habitual pregnancy loss is defined as the loss of two or more pregnancies [2,5,6]. Pregnancy loss is a common complication in the early stages of gestation. The prevalence of spontaneous abortions is 5%. According to world authors, 13.5 percent of wanted pregnancies ended in fetal loss. Habitual pregnancy losses are less common [1]. Recurrent pregnancy loss is reported to affect approximately 1–2% of women and is characterized by three consecutive pregnancy losses before 20 weeks from the last menstrual period. Recurrent pregnancy loss has a significant emotional impact on women and their partners. Pregnancy loss is a significant negative life event, and the repetitive nature of common pregnancy losses can exacerbate the grief experienced [3,4,7]. The etiology includes genetic, endocrine, infectious and anatomical factors, as well as autoantibodies, abnormal prothrombotic status and other aspects. Endometrial receptivity can also be explained as the state of the endometrium that allows for embryo adhesion, invasion and implantation. Endometrial and subendometrium hypoxia caused by poor blood flow causes slow receptivity, which reduces embryo implantation and increases the likelihood of spontaneous abortion. Thus, for successful implantation, estrogen levels are increased and are responsible for follicular growth, endometrial proliferation, myometrial thickness and increased blood supply. Estradiol levels in early pregnancy may reflect the quality of the dominant follicle and the function of the corpus luteum, and contribute to the maintenance of the corpus luteum. A positive correlation was found between serum estradiol levels and gestational age at 4-8 weeks of pregnancy. Serum estradiol levels in pregnant women who underwent abortion were significantly lower than in normal pregnant women. Progesterone deficiency and a shortened luteal phase may lead to suboptimal endometrial development. On the other hand, progesterone deficiency, on the contrary, is a manifestation of the follicular phase, which should be optimized in advance [10]. Given the above circumstances, it is necessary to comprehensively study the endometrium, biochemical and hormonal profile of the blood in women with habitual miscarriage.
Keywords: Pregnancy, Habitual miscarriage, Endometrium, Biochemical and hormonal profile, Hypoxia, Progesterone
Cite this paper: Matrizaeva Gulnara Djumaniyazovna, Ikhtiyarova Gulchekhra Akmalovna, Comprehensive Therapy of Miscarriage Based on the Study of Immunohistochemical Markers of Inflammation and Receptiveness of the Endometrium, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 38-42. doi: 10.5923/j.ajmms.20251501.07.
Article Outline
1. Objective of the Study
- To develop a pathogenetically substantiated algorithm for the complex treatment of miscarriage based on the study of immunohistochemical markers of inflammation and endometrial receptivity.
2. Materials and Methods of the Study
- A prospective observational comparative controlled study was performed on 258 women of childbearing age. All study participants were permanent residents of urban and rural areas of the Khorezm region and the Republic of Karakalpakstan.The contingent of examined women was divided into two groups:1. The main group - 198 women with habitual miscarriage.2. The control group - 60 healthy women who sought medical abortion for personal reasons.This distribution of groups made it possible to conduct a comparative analysis between patients with habitual miscarriage and healthy women to identify key differences in clinical indicators and establish the causes of the pathology. The immunohistochemistry study was conducted in the RIO and RIATM Pathomorphology Department. Scrapings from the uterus were collected in the Perinatal Center of the Khorezm Region in the gynecology department from women with miscarriage after a miscarriage in the period 2021-2023.Among the examined women, the frequency of miscarriage in the anamnesis ranged from 1 to 8, the average number was 2.1 ± 0.02 cases. For the study, samples of uterine curettage were selected from 40 women with miscarriage (2 or more spontaneous miscarriages or fetal arrest) and from 20 women who had a medical abortion during a normally developing pregnancy at their own request. The main group included scrapings from patients with habitual miscarriage in the early stages of various etiologies (main group, n = 40). he gestational age is determined by the first day of the last menstruation.
3. Results
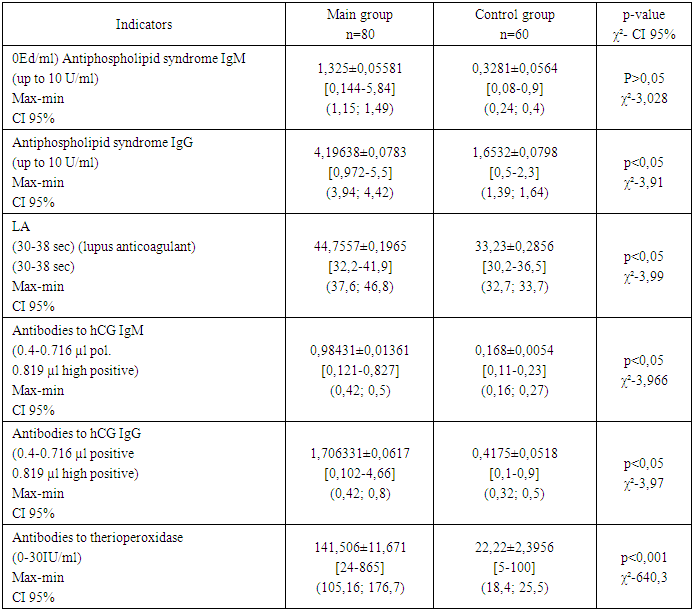
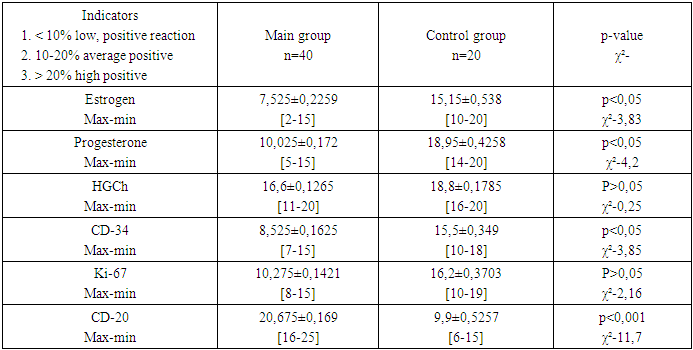
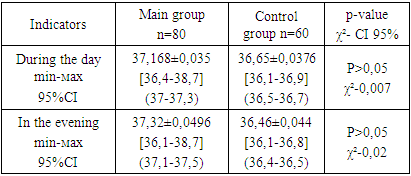
- Morphological examination are currently recognized as the gold standard worldwide. The histological block of cassettes taken from the incision from all patients was processed for immunohistochemical examination. The study used the radio transmission of the Bond Leica Australia immune processor (Australia), Ki67, CD34, estrogen and progesterone receptors, and XGCH monoclonal antibody were determined.In this study, using immunohistochemical analysis, we were able to identify the causes of early miscarriage at the cellular level. We studied the correspondence between the number of estrogen, progesterone and hCG receptors, the degree of cell proliferation, signs of inflammation and the state of molecular adhesion in the vessels. An analysis of the data of clinical, anamnestic and laboratory-instrumental methods of examining women with NB in the first trimester was carried out depending on the frequency of occurrence. Results of the study: The average age of the examined women in the main group was 28.6±0.39 years, in the control group 30.4±10.08 years. No statistically significant differences in age were found p>0.05.When distributing women in the main group by the frequency of observed miscarriages, it was found that the majority of women (almost two thirds) had 2 or 3 miscarriages (63.6%). The proportion of women with 4 or 5 miscarriages is also significant (36.4%). This may indicate a progressive inability to carry a pregnancy to term as the number of miscarriages increases. This indicates a high risk of recurrent miscarriage in women with a history of miscarriage. The control group (n=60) was represented by practically healthy women who had no miscarriages. Multiple miscarriages can increase the risk of future complications, such as infections associated with chronic inflammatory diseases of the reproductive organs. The probability of developing intrauterine adhesions also increases, which complicates implantation of the fertilized egg in subsequent pregnancies.In terms of the total number of pregnancies, patients with miscarriages had an advantage 758 (3.83±0.01) compared to women in the control group 173 (2.88±0.01) (p<0.001), while in the control group most pregnancies ended in full-term (term) births (157 cases (2.6±0.01)), while in the main group there were only 108 such births (0.55±0.01) (p<0.01). The number of miscarriages in the main group is extremely high - 624 (3.15±0.01) cases, which differs significantly from the control group, where only 2 (0.03±0.01) miscarriages were recorded (p<0.0001). Premature births were registered only in the main group (18 cases (0.09±0.01)). And this is associated with an increase in cases of ante- and postnatal fetal mortality. In the main group, there are cases of antenatal (20 cases (0.1±0.01)) and postnatal (22 cases (0.11±0.01)) fetal death. There are no such cases in the control group. The number of medical abortions in the main group is significantly lower (5 (0.025±0.01) versus 14 (0.23±0.01) than in the control group (p<0.01)), which may be due to the fact that women in the main group probably strive to keep the pregnancy despite the complications, while in the control group abortions could be performed at the woman's request. Thus, in the main group there is a clear tendency to multiple pregnancy losses (miscarriages and premature births), which leads to an increase in the number of pregnancies. However, successful outcomes (full-term births and live births) are observed significantly less frequently than in the control group. The high frequency of antenatal and postnatal fetal death in women of the main group indicates severe pathological processes occurring during pregnancy. The study of the general blood test revealed that patients with miscarriage have a significantly lower hemoglobin level of 90.4 g / l (CI 95% - 88.68; 92.1) compared to the control group 112.88 g / l; (CI 95% -109.4; 114.9), (χ² = 4.47; p<0.05). Our attention was drawn to another important point, the total number of leukocytes was increased by 1.5 times in the main group compared to the control, respectively 9.1181 ± 0.181 * 109 / l and 5.923±0.1167 * 109 / l. But did not exceed the reference values. Although during the examination, the women did not have symptoms indicating the presence of acute infectious processes. A tendency was revealed to increase the absolute number of leukocytes in women of group 1 during developing pregnancy, as the death of the fetus or spontaneous abortion occurred, leukocytes began to decrease. A decrease in the level of lymphocytes (20.151±0.6077%) in women with miscarriage compared to the control group (31.712 ± 0.51%) may indicate suppression of the immune system (χ² = 4.21; p<0.05). The frequency of occurrence of increased ESR in patients of the main group (16.112±0.429 mm / h) had a significant difference from the control group (9.883±0.6336 mm / h) (χ² - 3.92; p<0.05). This table 1 reflects the key immunological indicators that play an important role in the pathogenesis of miscarriage. Antiphospholipid antibodies of IgM class are significantly higher in the main group (1.325±0.05581 vs. 0.3281±0.0564 U/ml), the difference between the groups did not reach statistically significant difference (χ²=3.028; p>0.05), but the indicator has clinical significance. Antiphospholipid antibodies of IgG class are also significantly higher in the main group (4.19638±0.0783 U/ml; 95% CI- 3.94; 4.42 vs. 1.6532±0.0798 U/ml; 95% CI-1.39; 1.64). This indicates the presence of an autoimmune process in women with miscarriage, and has a statistically significant difference (χ²-3.91; p<0.05). Antiphospholipid antibodies IgG can interact with the membranes of vascular wall cells, leading to thrombus formation and impaired blood circulation in the placenta. Antibodies to hCG class IgM in the main group are significantly higher compared to the control group, respectively 0.98431±0.01361 μl; 95% CI-0.42; 0.5 and 0.168±0.0054 μl 95% CI-0.16; 0.27. This indicator has high statistical significance (χ²=3.966; p<0.05). High levels of antibodies to human chorionic gonadotropin (hCG) class IgG in the main group (1.706331±0.0617μl versus 0.4175±0.0518) are 4 times higher than in the control group, indicating violations of hormonal support of pregnancy. Statistically significant differences (χ²=3.97; p<0.05) confirm the clinical importance of this indicator. The highest level of Anti hCG IgG was 4.66μl, which was 11.7 times higher than the normal values. These antibodies can block the action of hCG, which will lead to a violation of implantation and fetal development.
|
|
|
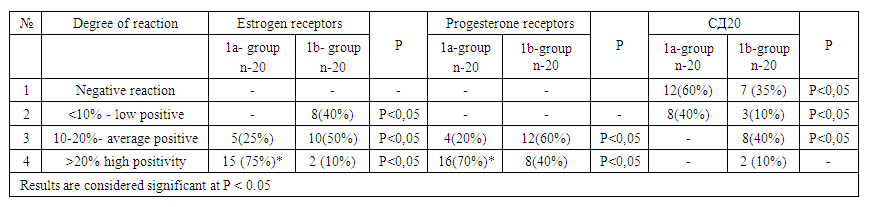 | Table 4. Expression of hormonal receptors in the endometrium after treatment |
4. Conclusions
- Thus, pregravid preparation has a significant effect on reducing the incidence of complications during pregnancy, such as retrochorial hematoma, non-viable pregnancy and spontaneous abortion. The threat of miscarriage and vomiting of pregnant women are also less common in women who have undergone preparation. Preparing the body for pregnancy, including hormonal correction, improving health, can be a key factor in successful gestation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML