-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 15-20
doi:10.5923/j.ajmms.20251501.03
Received: Dec. 9, 2024; Accepted: Dec. 26, 2024; Published: Jan. 11, 2025

Mri-Based Diagnostics of Tandem Stenosis in Cervical and Lumbar Spinal Regions
A. A. Ablyazov1, O. V. Ablyazov2, Z. Sh. Madumarova1, Sh. Sh. Turgunov1, G. B. Khalibaeva2
1Andijan State Medical Institute, Andijan, Uzbekistan
2Center for the Development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Tandem spinal stenosis, a type of narrowing of the spinal motion segment, is most commonly observed in the cervical and lumbar regions. It may present with clinical symptoms in one region while remaining asymptomatic in another, complicating diagnosis and treatment. Methods: This study aimed to evaluate the effectiveness of radiological methods for diagnosing tandem spinal stenosis in the cervical and lumbar regions using the specialized MRI Spine Volumetry program integrated into MRI systems. A total of 85 patients with various presentations of tandem spinal stenosis were analyzed. Results: Tandem spinal stenosis was categorized into three clinical variants: symptomatic lumbar stenosis with asymptomatic cervical stenosis, symptomatic cervical stenosis with asymptomatic lumbar stenosis, and symptomatic stenosis in both regions. The severity of tandem stenosis was optimally assessed by measuring the cross-sectional area of the spinal canal using the MRI Spine Volumetry program. Conclusion: MRI Spine Volumetry provides a precise and reliable method for determining the severity of tandem spinal stenosis, supporting its utility in the diagnostic evaluation of this complex condition. Its application enables accurate assessment of both symptomatic and asymptomatic regions, aiding in comprehensive clinical management.
Keywords: Tandem spinal stenosis, Cervical and lumbar spinal regions, MRI diagnostics, MRI Spine Volumetry program
Cite this paper: A. A. Ablyazov, O. V. Ablyazov, Z. Sh. Madumarova, Sh. Sh. Turgunov, G. B. Khalibaeva, Mri-Based Diagnostics of Tandem Stenosis in Cervical and Lumbar Spinal Regions, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 15-20. doi: 10.5923/j.ajmms.20251501.03.
Article Outline
1. Introduction
- Degenerative processes in the spinal segment, including intervertebral disc protrusion, hypertrophy, and ossification of the posterior longitudinal and yellow ligaments, as well as other intra- and extra-canal spinal pathologies, progressively reduce the size of the spinal canal, ultimately leading to spinal stenosis [1] [2] [5] [6] [11]. Spinal stenosis is a common pathological condition that can significantly impact patients’ quality of life by causing symptoms such as pain, numbness, motor deficits, and functional impairment. Among its various forms, tandem spinal stenosis represents a unique subset characterized by the coexistence of stenotic lesions at multiple levels of the spine—most commonly the cervical and lumbar regions, and more rarely, all three levels including the thoracic spine [3] [4] [8] [10]. Although tandem stenosis affecting all three levels is exceptionally rare, it poses a unique diagnostic and therapeutic challenge.Tandem stenosis of the cervical and lumbar regions is more prevalent, comprising approximately 5-25% of spinal stenosis cases. In these scenarios, symptoms of neural compression often dominate in one region, overshadowing subtler manifestations in the other affected areas [1] [7] [12]. However, in some cases, clinical symptoms may be minimal or even absent at one level, further complicating accurate diagnosis [9] [13]. This diagnostic complexity underscores the necessity of advanced imaging modalities that can reliably identify and quantify stenotic changes across the spinal axis.Given the increasing prevalence of degenerative spinal conditions in an aging population, precise diagnostic methods are essential to ensure timely and effective interventions. Radiological imaging, particularly magnetic resonance imaging (MRI), remains the cornerstone for evaluating spinal stenosis. In this study, we sought to evaluate the utility and effectiveness of a specialized MRI-based Spine Volumetry program, which is integrated into modern MRI systems, in diagnosing tandem stenosis of the cervical and lumbar spinal regions. By providing precise volumetric measurements of the spinal canal and its contents, this program may enhance diagnostic accuracy and aid in the clinical management of patients with suspected tandem stenosis.
2. Materials and Methods
- Between 2021 and 2023, a study was conducted at the Andijan Multidisciplinary Regional Hospital and the “Star Med Center” in Tashkent using MRI systems, specifically the “Brivo MR 355” (USA) and PHILIPS (Netherlands) machines with a magnetic field strength of 1.5 Tesla. The study included 60 control subjects (30 with cervical spine scans and 30 with lumbar spine scans) and more than 3250 individuals with various spinal pathologies. Among these, 978 patients were identified with isolated stenosis in either the cervical or lumbar spinal canal. Of these, 85 patients (approximately 8.7% of the isolated stenosis cases) presented with symptoms of spinal canal stenosis and had undergone prolonged conservative treatment without significant improvement. These patients, suspected of having tandem stenosis of the cervical and lumbar spinal canal, became the focus of this study.Tandem stenosis was classified into three clinical variants: 31 patients presented with active lumbar stenosis symptoms and asymptomatic cervical stenosis; 28 patients had active cervical stenosis symptoms with asymptomatic lumbar stenosis; and 26 patients exhibited active neurological symptoms of tandem stenosis in both regions. The narrowing of the spinal canal in these patients was attributed to intervertebral disc herniation, hypertrophy of the ligamentous apparatus within the canal, and other intracanal pathologies.To assess the severity of tandem stenosis, the following parameters were measured for all three clinical variants: midsagittal and frontal dimensions of the osseous and soft tissue contours of the spinal canal, the vertical height of intervertebral discs, the cross-sectional area of the osseous and soft tissue contours, and the vertical height of vertebral bodies. These measurements were compared with normative parameters for the cervical and lumbar spinal regions.
3. Results
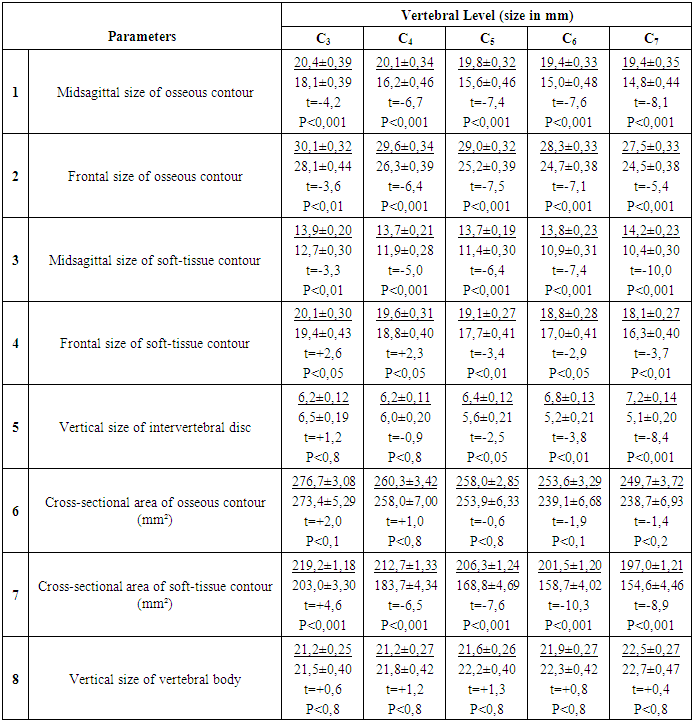
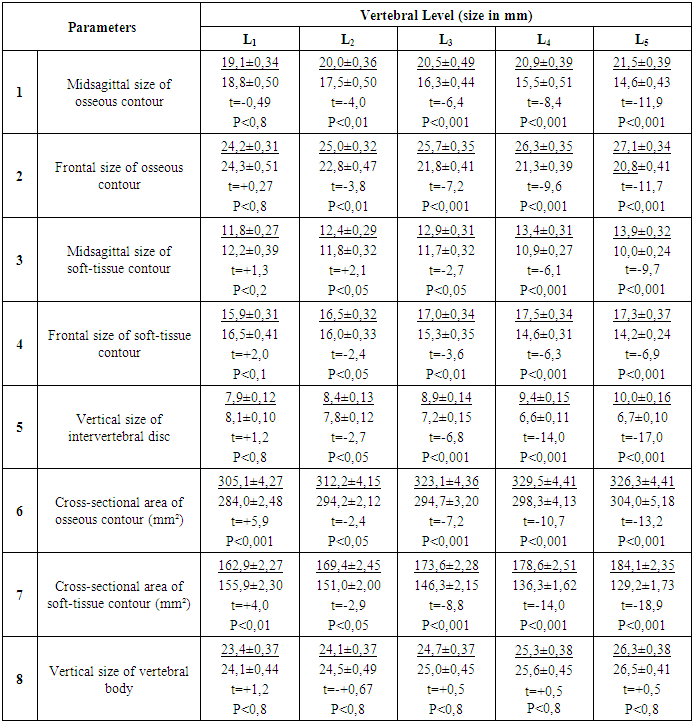
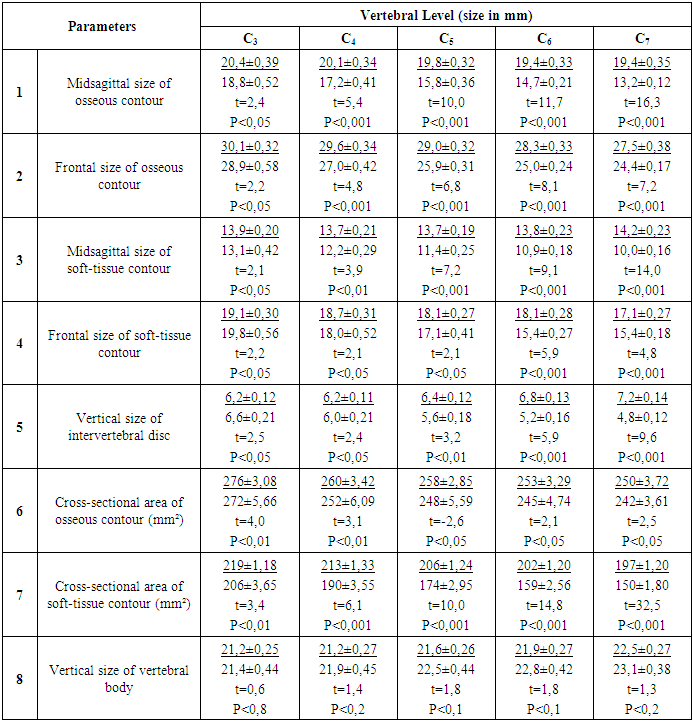
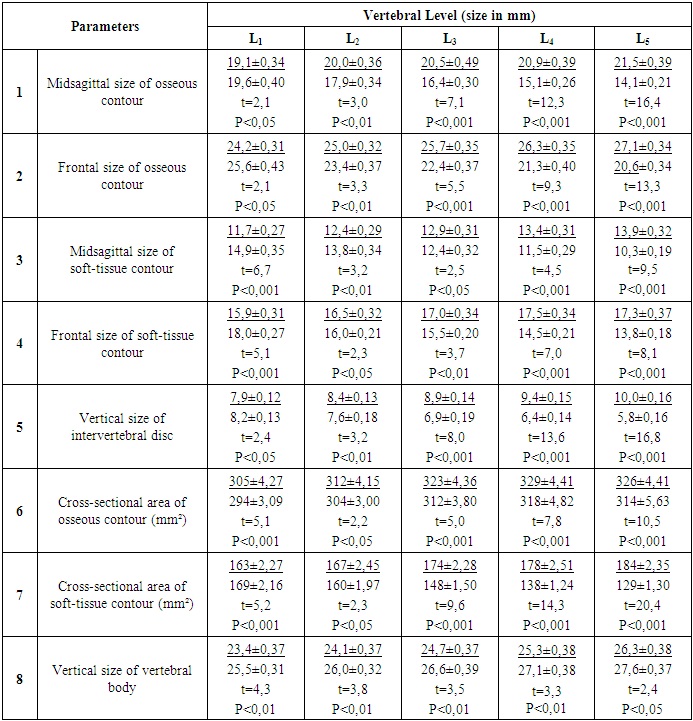
- In the first clinical variant, all 31 patients reported limitations in walking distance and varying degrees of pain in the lumbar spine upon consultation. These patients were diagnosed with degenerative lumbar spinal stenosis and had undergone prolonged conservative treatment without significant improvement. MRI scans of their cervical spine (Table 1) revealed that the midsagittal and frontal dimensions of the osseous and soft tissue contours were significantly reduced compared to normal values (P<0.05 to P<0.001): C3 by 11.3%, 8.6%, 10.6%, and 8.5%; C4 by 19.4%, 11.1%, 13.1%, and 9.1%; C5 by 21.1%, 15.4%, 16.8%, and 12.3%; C6 by 22.7%, 17.8%, 21.0%, and 16.7%; and C7 by 23.7%, 19.1%, 26.8%, and 19.9%, respectively. Vertical intervertebral disc heights at C3 and C4 were not significantly reduced (P<0.8), but significant reductions were observed from C5 to C7 (P<0.05 to P<0.001). The cross-sectional area of the soft tissue contour, measured using MRI Spine Volumetry, was significantly reduced (P<0.001) across all levels: C3 by 12.3%, C4 by 13.6%, C5 by 18.0%, C6 by 23.5%, and C7 by 26.3%. The cross-sectional area of the osseous contour and vertebral body heights showed no significant deviations from normal (P<0.8).
|
|
|
4. Discussion
- The clinical presentation of degenerative processes in the cervical and lumbar spine is multifaceted, encompassing various pathomorphological forms manifested as isolated or combined (tandem) stenosis. Isolated spinal canal stenosis, as a distinct nosological form of spinal pathology, was comprehensively described by H. Verbiest in the 1950s [12]. Verbiest introduced the terms "relative" and "absolute" stenosis, categorizing them based on the midsagittal diameter of the spinal canal. A canal diameter of up to 12 mm was classified as "relative" stenosis, while a diameter of 10 mm or less was defined as "absolute" stenosis. According to Yu.E. Pedachenko (2009), the evaluation of spinal stenosis should consider not only the reduction in the midsagittal diameter but also the cross-sectional area of the spinal canal, measured using an approximated triangular shape [3]. The authors classify stenosis as "relative" when the midsagittal diameter of the spinal canal decreases to 12 mm and its cross-sectional area to 100 mm² (normal value exceeding 145 mm²). It is defined as "absolute" when the midsagittal diameter reduces to 10 mm or less, and the cross-sectional area decreases to 75 mm² or less.To assess the severity of spinal canal stenosis, we identified some inaccuracies in the methodologies proposed by H. Verbiest (1954) and Yu.E. Pedachenko (2009) [12] [3]. Determining stenosis severity solely based on the reduction of the midsagittal diameter fails to account for narrowing caused by a reduction in the frontal diameter. Intracanal pathologies, such as paramedian and posterolateral disc herniations, hypertrophy and ossification of the ligamentum flavum, intracanal mass lesions, and osteophytes, predominantly affect the lateral areas of the spinal canal, leading to unaccounted reductions in the frontal diameter.Similarly, measuring the spinal canal area using an approximated triangular shape is inherently flawed, as portions of the canal outside the triangle's boundaries are excluded, resulting in incomplete assessment of stenosis severity.These limitations highlight the ongoing challenges in defining the severity of isolated and combined (tandem) spinal stenosis. Current criteria insufficiently correlate clinical and neurological symptoms with compressive factors visualized through radiological methods. This underscores the need for further investigation into the formation and progression of degenerative tandem spinal stenosis.To address these gaps, we utilized the specialized MRI Spine Volumetry program, available in MRI systems with a magnetic field strength of 1.5 Tesla. This program measures the perimeter of the osseous and soft tissue contours, subsequently calculating the cross-sectional area of the spinal canal for these contours automatically.The normal cross-sectional area for the cervical spinal canal ranged from 250-270 mm² for osseous contours and 190-220 mm² for soft tissue contours. For the lumbar spinal canal, the corresponding normal values were 300-325 mm² and 165-185 mm², respectively. A reduction in the cross-sectional area of the cervical and lumbar spinal canal by 15% was classified as "relative" stenosis, while a 30% reduction was classified as "absolute" stenosis for both isolated and tandem cases.
5. Conclusions
- 1. Due to the ambiguous clinical manifestations of tandem stenosis, effective diagnosis requires close collaboration between neurologists, neurosurgeons, and radiology specialists.2. In cases of degenerative isolated spinal stenosis, a comprehensive assessment of the clinical presentation and imaging results is essential for accurately interpreting the complex manifestations of tandem stenosis.3. The optimal method for determining the severity of isolated and tandem stenosis is measuring the cross-sectional area of the spinal canal using the specialized MRI Spine Volumetry program, available in MRI systems with a magnetic field strength of 1.5 Tesla.
ACKNOWLEDGEMENTS
- The authors thank all the participants in this study.
Conflict of Interest
- The authors declare no conflicts of interest.
References
| [1] | Byval'tsev VA, Shepelev VV, Nikiforov SB, Kalinin AA. Isolated and combined degenerative tandem stenoses of the cervical and lumbar spinal canal: literature review. Hirurgia Pozvonochnika. 2016; 13(2): 52-61. |
| [2] | Kariev MH, Norov AU, Ishmukhamedov SN, Yugay IA. Clinical features of intervertebral disc herniation in degenerative lumbar stenosis. Voprosy Neyrokhirurgii Im N.N. Burdenko. 2001; (3): 14-15. |
| [3] | Pedachenko YuE. Lumbar spinal stenosis. Ukrayinskiy Neyrokhirurgicheskiy Zhurnal. 2009; (4): 9-14. |
| [4] | Prodan AI. Pathogenesis of lumbar spinal stenosis: modern concepts. Vestnik Travmatologii i Ortopedii Im N.N. Priorova. 2008; (2): 88-93. |
| [5] | Feniksov VM, Zelenkov PV. Tandem spinal stenosis: clinical features, diagnostics, and surgical tactics. Association of Neurosurgeons of Russia. 2021; 23: 146-153. |
| [6] | Alvin MD, Alentado VJ, Lubelski D, et al. Cervical spine surgery for tandem spinal stenosis: the impact on low back pain. Clin Neurol Neurosurg. 2018; 166: 50-53. |
| [7] | Costandi S, Chopko B, Mekhail M, et al. Lumbar spinal stenosis: therapeutic options review. Pain Pract. 2015; 15(1): 68-81. |
| [8] | Freedman BA, Hoffler CE, Cameron BM, et al. A comparison of computed tomography measures for diagnosing cervical spinal stenosis associated with myelopathy: a case-control study. Asian Spine J. 2015; 9: 22-29. |
| [9] | Hong CC, Liu KPG. A rare case of multiregional spinal stenosis: clinical description, surgical complication and management concept review. Global Spine J. 2015; 5(1): 49-54. |
| [10] | Inoue T, Ando K, Kobayashi K, et al. Primary cervical decompression surgery may improve lumbar symptoms in patients with tandem spinal stenosis. Eur Spine J. 2021; 30: 899-906. |
| [11] | Shabat S, Miller LE, Block JE, et al. Minimally invasive treatment of lumbar spinal stenosis with a novel interspinous spacer. Clin Interv Aging. 2011; 6(8): 227-233. |
| [12] | Verbiest H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br. 1954; 36(6): 230-237. |
| [13] | Yamada T, Yoshii T, Yamamoto N, et al. Clinical outcomes of cervical spinal surgery for cervical myelopathic patients with coexisting lumbar spinal canal stenosis (tandem spinal stenosis): a retrospective analysis of 297 cases. Spine. 2018; 43(4): E234-E241. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML