-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(1): 9-14
doi:10.5923/j.ajmms.20251501.02
Received: Dec. 6, 2024; Accepted: Dec. 28, 2024; Published: Jan. 11, 2025

A Strategy for the Treatment of Patients with Diabetic Foot Gangrene Against the Background of Scheduling Hemodialysis
K. J. Matmurotov1, F. A. Safarov1, B. Sapaev2
1Tashkent Medical Academy, Tashkent, Uzbekistan
2Alfraganus University, Tashkent, Uzbekistan
Correspondence to: K. J. Matmurotov, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The results of the study and inpatient treatment of 147 patients with diabetic feet gangrene against the background of scheduling hemodialysis were analyzed, in which various surgical operations were carried out on the feet. Patients were in stationary treatment in the department of purulent surgery of the multidisciplinary clinic of the Tashkent Medical Academy in 2016-2023. Depending on the surgical tactics of the surgical method of treatment, patients are divided into 2 groups. Group 1 (comparison) was made up of 79 patients (53.8%) admitted to inpatient treatment in 2016-2018. In these patients, endovascular revascularization practices and small operations were performed in the traditional way without taking into account the damage nature of the foot and toe peripheral arteries. Group 2, which was considered the main, included 68 patients (46.2%) who were admitted to inpatient treatment in the same unit in 2019-2023.
Keywords: Diabetes, Diabetic foot syndrome, Gangrene, Amputation
Cite this paper: K. J. Matmurotov, F. A. Safarov, B. Sapaev, A Strategy for the Treatment of Patients with Diabetic Foot Gangrene Against the Background of Scheduling Hemodialysis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 1, 2025, pp. 9-14. doi: 10.5923/j.ajmms.20251501.02.
Article Outline
1. Introduction
- Diabetes mellitus is the most common endocrine disease in the world. According to the IDF Diabetes Atlas for 2023, 630 million diabetes patients are registered in the world, and according to predictions, 1 billion people suffer from diabetes by 2045 [1]. According to 2021 statistics, 3,582,865 patients in our country were diagnosed with DM [2,3]. Experts have been regularly studying the problem of diabetes and its complications for the past 20-30 years. During these years, various theories of DM etiopathogenesis have been proposed and the main factors in the development of the disease have been identified. By the end of the 20th century, most scientists had come to a general consensus that a number of tissues, organs and systems would be involved in the pathological process in diabetes at the same time. One of the most severe and dangerous complications of DM is foot damage [4,5,7]. It is known that at the expense of atherosclerotic lesions in the arteries of the feet, 27-43% of patients show distal flow disorders of the arterial system, which in turn indicates that joint stenosis or occlusion of small and medium-sized arteries may occur in the areas below the knee [8]. In this case, atherosclerosis of the calf arteries can occur between them for a long time without clinical symptoms due to the developed collateral network. There may be no ischemic symptoms if at least one of the tibial arteries is unchanged i.e. performs its function fully [9,10]. Over the past decades, "evolution" of atherosclerosis has been observed and treatment strategies have changed to some extent. The number of patients with multiple occlusions and damage to the knee arteries is increasing, which reduces the chances of conventional vascular surgery. For this reason, more than 30% of patients do not have the opportunity to perform standard reconstructive surgery [11]. As a result of this, the implementation of primary high amputations of the legs is observed along with an increase in mortality and reaches 21-44% [12].Critical limb ischemia (CLI) is constant pain for two weeks (rare exacerbation), characterized by the presence of trophic injuries on the toes, which in turn corresponds to stages 3-4 under the Fontaine-Pokrovsky grade and 4-6 under the Rutherford classification. It was mentioned that the frequency of morbidity with CLI on the Earth is 50-100 cases per 100,000 people per year [13]. In patients of this contingent, critical ischemia to the tibial arteries (in most cases, each artery below the knee) is indicated as the cause of critical ischemia observed in the feet in 25-30% of cases [14]. Only 23-80% of patients in this condition manage to carry out the restoration of arterial circulation only in cases, and in the general case 16% of patients are forced to carry out a primary above the knee amputation [15].The purpose of the study was to improve the results of the treatment of patients with diabetic gangrene of the feet against the background of scheduling hemodialysis.
2. Material and Methods
- In this research work, the results of the surgical treatment of 147 patients with diabetic feet gangrene against the background of scheduling hemodialysis were analyzed, in which various surgical operations were carried out on the feet. Patients were in stationary treatment in the department of purulent surgery of the multidisciplinary clinic of the Tashkent Medical Academy in 2016-2023. Depending on the surgical tactics of the surgical method of treatment, patients are divided into 2 groups. Group 1 (comparison) was made up of 79 patients (53.8%) admitted to inpatient treatment in 2016-2018. In these patients, endovascular revascularization practices and small operations were performed in the traditional way without taking into account the damage nature of the foot and toe peripheral arteries. Group 2, which was considered the main, included 68 patients (46.2%) who were admitted to inpatient treatment in the same unit in 2019-2023. In them, endovascular revascularization practices in the peripheral arteries of the feet were carried out according to the combined method improved taking into account the damage nature of the tibial arteries. In addition to surgery, against the background of the hemodialysis program, all patients with diabetic foot gangrene received an intensive complex of systemic antibacterial, double antiagregant, therapy and treatment measures for vasoconstriction. It should also be noted that all patients are in scheduling hemodialysis, which complicated our surgical treatment tactics in terms of conducting adequate infusion therapy and catheter therapy, since there is no possibility of hemodialysis in our medical complex, and every 3 days patients were forced to go to another medical institution. When choosing a strategy for surgical procedure in patients in the comparison group, the degree of damage to peripheral arterial flow, the nature of the pathological process and the effectiveness of bacterial flora on antibacterial drugs were taken into account. Endovascular Surgery in patients in the main group was carried out according to our improved methodology, taking into account the damage nature of the tibial arteries, which are described in detail in this dissertation. In principle, the patients examined were assessed as having a severe course of DM, with clinical signs of complications against the background of organic changes in target organs and systems.
3. Results and Discussion
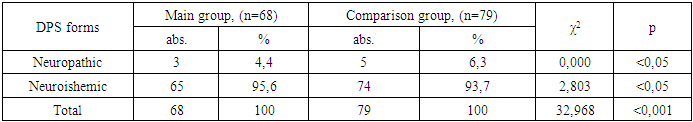
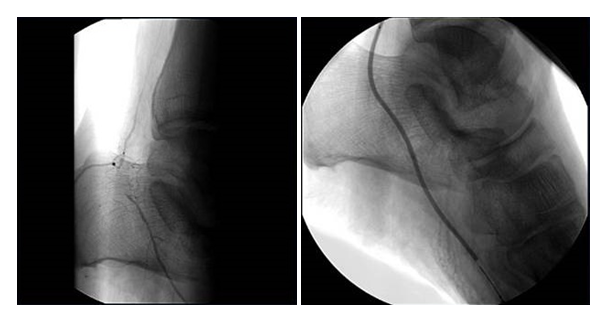
- Despite adjustments to treatment tactics aimed at improving affected limbs, these patients were required to receive appropriate preoperative training and conduct in a special manner during the postoperative period. There were 4 (3.8%) of patients who were not diagnosed with deviations in members other than affected toes. Thanks to long-term full-complex treatment, much more positive results were achieved in them. Patients undergoing endovascular revascularizing surgery against the background of scheduling hemodialysis were diagnosed with ischemic and neuroishemic forms of DFS (Table 1).
|
|
 | Figure 1. The initial appeal is the appearance of the foot toe |
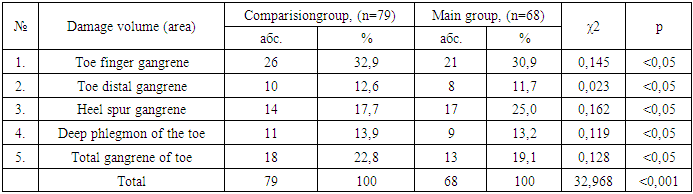
 | Figure 2. Subintimal angioplasty via sub knee access |
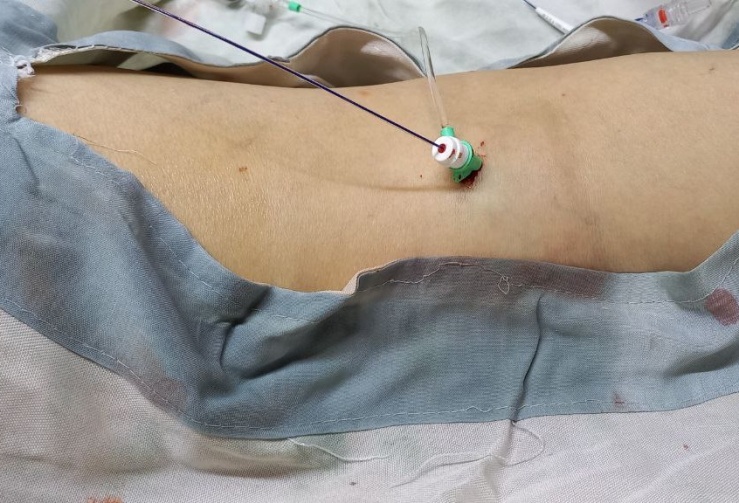
 | Figure 3. Angiography before and during the implementation subintimal angioplasty |
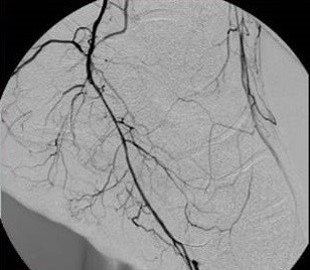 | Figure 4. Vascular appearance after SBAP implementation |
 | Figure 5. Toe view 1.5 months after SBAP implementation |
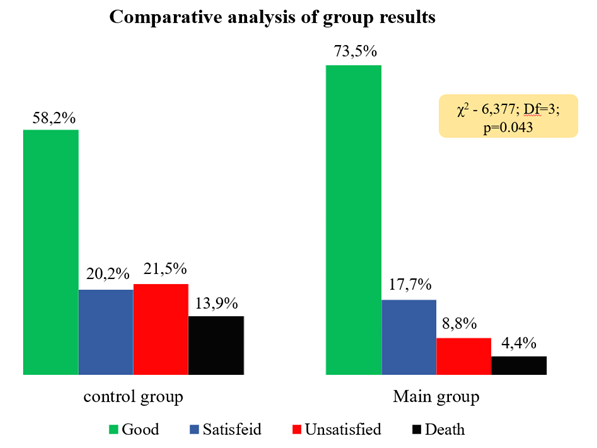 | Figure 6. Efficacy indicators of combined endovascular treatment in diabetic gangrene of the toes |
4. Discussion
- In most cases, it is necessary to carry out a above-the-knee amputations of the legs as a result of improperly performed operationalization or a selective tactic that is not suitable for the treatment of patients with purulent-necrotic processes of the toe against the background of DFS. After above-the-knee amputations, most patients lose their social status and experience mental emotional stress, with a very high probability of losing even the second leg in the next 2 years. Therefore, this study is relevant in terms of the social status of patients and the prevention of severe complications in patients with ulcerative defects against the background of DFS.Thus, we have improved the technique of performing a combined endovascular operation. In this case, the localization of the purulent-necrotic lesion or the nature of damage to the peripheral arteries is strictly taken into account. In patients with a severe purulent process (wet gangrene) on the toe, second stage operation was carried out: the first stage - surgical dating of the pathological hearth with maximum preservation of suspicious tissue around the wound, the second stage-examination of peripheral arteries with endovascular revascularization, followed by reconstructive plastic surgery, taking into account local tissues in the toe part and localization of lesion. The time for the implementation of the second stage was determined individually and averaged 3-10 days. In the case of critical ischemia (such patients in the studied groups 96.3%), we first tried to carry out revascularization of the peripheral arteries of the legs (balloon angioplasty) (in the main group, only subintimal balloon angioplasty), dating of the postiniratory-necrotic lesion, and then reconstructive surgery.In almost half of patients with amputated legs, a state of depression is observed: in 52% - mild, in 8% - severe (on the Hamilton Depression Rating Scale). This once again emphasizes how important it is for the patient to maintain the support activity of his legs and the possibility of returning to normal social life.Summarizing these cited data, it should be noted that according to the affected part of the toe and the nature of the arterial basin lesions of the legs, the results of treatment were significantly improved in terms of maintaining the functional and musculoskeletal functions of the foot using an improved method developed to perform combined endovascular operations. The main effect of the improved method was achieved by reducing the number of patients with whom above-the-knee amputations were performed, which ensured the preservation of the optimal base function of the paw. Properly selected surgical strategy and technically based on the affected parts of the toe contributed to the smooth course of the post-revascularization operation, which made it possible to achieve positive treatment results.
5. Findings
- 1. In terms of the volume of arterial nutrition of the toe and the possibility of compensating for circulatory disorders in the etiopathogenesis of the occurrence and development of gangrene of the ankle in DFS, the posterior large tibial artery plays a key role, since the probability of the occurrence of a purulent-necrotic process in the toe in isolating damage to the posterior tibial arterial basin is 59.9% (p>0.05).2. An improved surgical strategy for the execution of combinatorial ьштшьфд штмфқшму operations (main group (n=68)) resulted in good results in 73.5% of cases p>0.05), which is significantly higher in comparison group patients (58.2%). As a result of these surgical tactics, a low rate of mortality was recorded in the post - operative period - 4.4% (n=3) (in the comparison group-13.9% (n=11)) (r>0.05).3. In patients with toe gangrene with DFS against the background of chronic renal failure, the implementation of combined endovascular operations reduces the preservation of functional activity of the toe from 59.4 to 72.3% (r>0.05), improves musculoskeletal activity from 78.3 to 90.7% (p>0.05), and in turn reduces the frequency of above-the-knee amputations of the legs from 21.5 (n=17) to 8.8% (n=6) (p>0.05).
Consent
- It is not applicable.
Ethical Approval
- It is not applicable.
Competing Interests
- Authors have declared that no competing interests exist.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML