-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3417-3419
doi:10.5923/j.ajmms.20241412.72
Received: Dec. 13, 2024; Accepted: Dec. 26, 2024; Published: Dec. 31, 2024

To Determine Changes in Inflammatory Cytokines IL-1β, IL-6 and Assess Liver Function in Middle-Aged and Elderly Patients with Non-Alcoholic Fatty Liver Disease in Middle-Aged and Elderly Patients Who Suffer COVID-19
Vokhid Z. Zokirov
Doctoral Student in the Specialty of Internal Medicine, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
Correspondence to: Vokhid Z. Zokirov, Doctoral Student in the Specialty of Internal Medicine, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Multiple pro-inflammatory factors - IL-1β, IL-1RA, IL-2, IL-4, IL-6, IL-8, IL-9, IL-13, FGFβ, G-KCF in the immune system of patients with COVID-19 , GM-KCF, INF-g, IP-10, MIP-1a, Delayed increase in MIP-1β, TNFα (Tumor necrosis factor), granulocyte colony-stimulating factor and other cytokines and growth factors causes a cytokine flood [1,2]. Cytokines hyperproduction and hypercoagulation induced by it, as well as leukocyte and neutrophil migration to the affected area and hypersecretion of prolytic substances. (neutrophils absorb lactase and other proteases in large quantities) [3,11] as a result, it damages not only the altered cells but also healthy cells and leads to organ failure. [4]. In COVID-19, immunopathological processes and the development of a cytokine storm occur in a sequence, with suppression or inhibition of interferon and other nonspecific immunity, direct (through inflammasome) and indirect (through self-damage to immunocytes) cytokine storms, and systemic inflammation. This destroys vascular endotheliocytes, induces hypercoagulability, and enhances secondary alteration of organs by immune cells. Various pathophysiological disturbances in the pathogenesis of COVID-19 lead to multiorgan failure by damaging various organs and organ systems.
Keywords: COVID-19, Non-alcoholic fatty liver disease, IL-1β, IL-6, Cytokine storm
Cite this paper: Vokhid Z. Zokirov, To Determine Changes in Inflammatory Cytokines IL-1β, IL-6 and Assess Liver Function in Middle-Aged and Elderly Patients with Non-Alcoholic Fatty Liver Disease in Middle-Aged and Elderly Patients Who Suffer COVID-19, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3417-3419. doi: 10.5923/j.ajmms.20241412.72.
1. Introduction
- IL-1β – It is a proinflammatory or inflammatory cytokine that belongs to the interleukin-1 family and is important in a variety of physiological functions and pathological processes, playing an important role in health and disease [5]. IL-1β plays a very important role in the body’s defense mechanism against pathogens through acute inflammation and the development of adaptive immunity [6]. IL-1β is produced by macrophages and is important in the development of chronic inflammation, obesity, and insulin resistance. Furthermore, IL-1β has been shown in several studies to be important in the pathophysiology of NAFLD through several mechanisms, particularly the development of steatosis, disruption of normal insulin signaling, and induction of fibrotic protein production. [7,8].Also, IL-6, a pro-inflammatory cytokine, is important in the development of the innate and adaptive immune response and is pathogen-specific by leukocytes and stromal cells. is produced as a result of the activation of the receptor (pattern recognition receptor). Dysregulation of IL-6 production is of important pathogenetic importance in the development of chronic inflammation and autoimmune diseases, including atherosclerosis, insulin resistance, and NAFLD [9,10].
2. Material and Methods
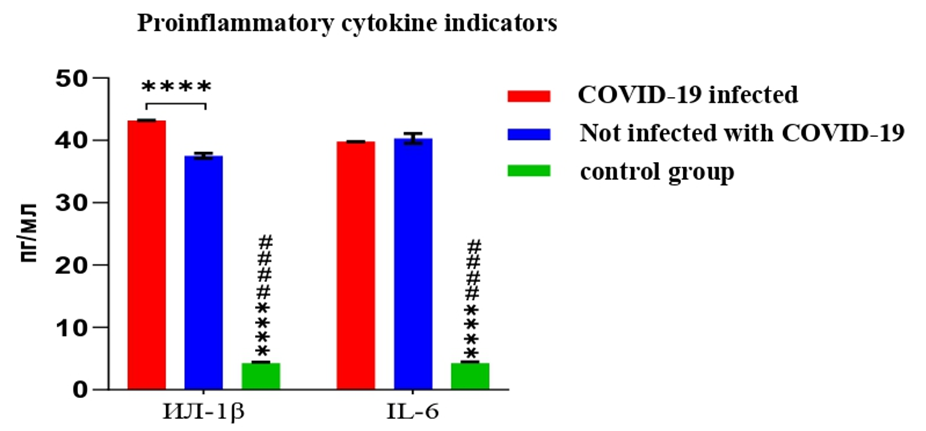
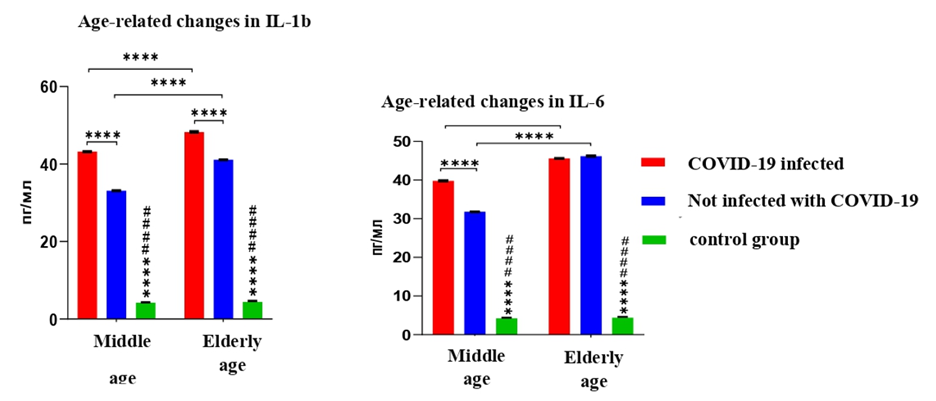
- Age classification of people developed by the World Health Organization (WHO) in 2015 was used to classify patients by age. In this classification, 25-44-year-old people form the youth group, 45-59-year-old people are middle-aged, 60-74-year-old people are old people, 75-90-year-old people are old people, and people over 90 years old are long-lifers. The study included 94 people who did not have COVID-19, of which 42 (44.7%) were middle-aged 45-59 (average 48.2±3.2), 52 (55.3%) were elderly 60-76 (65.2 ±4.2) patients. Also, out of 84 patients diagnosed with COVID-19, 34 (40.4%) are middle-aged (47.3±4.3), 50 (59.5%) are elderly (68.4±2.2).The main group (AG) of patients and control (NG) individuals are representative groups in terms of important demographic (age, gender, etc.), anthropometric (weight, body mass or Ketle index, etc.) indicators and other parameters divided.The study examined the general and/or specific role of IL-1β and IL-6 cytokines in disease progression, as well as their association with NAFLD levels and diagnostic efficacy in predicting the underlying disease, in patients with and without COVID-19 who had nonalcoholic fatty liver disease (NAFLD).During the study, patients with and without COVID-19, as well as healthy controls, The role of IL-1β and IL-6 cytokines in the development of COVID-19-related NAFLD and unrelated NAFLD was examined by comparing their levels (look at picture 1).
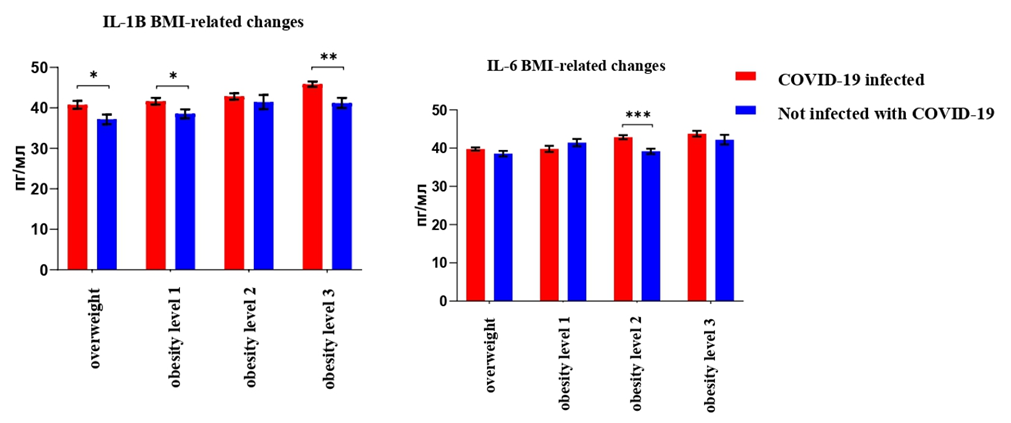 | Picture 3. Changes in pro-inflammatory cytokines in different groups depending on patients' BMI. Statistical significance level: * – P<0.05; ** – P<0.01; *** – P<0.001, **** – P<0.0001 |
3. Conclusions
- 1. The levels of IL-1β and IL-6 cytokines were found to be statistically significantly increased in patients with NAFLD, those with and without COVID-19, compared to the control group, and among both patient groups, only patients with COVID-19 had a statistically significant increase in the level of IL-1β cytokine.2. In patients with COVID-19, IL-1β and IL-6 levels were found to be 11.8% (P<0.0001) and 14.5% (P<0.0001) higher in elderly patients than in middle-aged patients, respectively, and 24.1% (P<0.0001) and 45.3% (P<0.0001) higher in elderly patients than in middle-aged patients, respectively, than in non-COVID-19 patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML