-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3409-3413
doi:10.5923/j.ajmms.20241412.70
Received: Dec. 11, 2024; Accepted: Dec. 25, 2024; Published: Dec. 31, 2024

Results of Arthroplasty in Fractures of Proximal Femur in the Elderly Patients
Irismetov M. E., Alimov A. P., Sоpaev Z. E., Abdurakhimov S. N.
Republican Specialized Scientific Practical Medical Center of Traumatology and Orthopedics of the Ministry of Health of the Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to analyzing the results of arthroplasty for proximal femoral fractures in elderly patients. The study reviews clinical outcomes, complications, and the recovery process after endoprosthetic replacement in this group of patients. Special attention is paid to age-related features such as decreased bone strength, comorbidities and their influence on the results of surgery. Evaluation of functional results, rehabilitation time and the level of independence of patients after arthroplasty allows to reveal the effectiveness of the method in this age category. The results of the study show that arthroplasty is a highly effective method of treatment of proximal femur fractures in elderly patients, contributing to the improvement of the quality of life and functional activity.
Keywords: Arthroplasty, Hip fractures, Proximal femur, Elderly patients, Endoprosthesis, Rehabilitation, Clinical results, Functional outcomes, Osteoporosis, Age peculiarities, Complications
Cite this paper: Irismetov M. E., Alimov A. P., Sоpaev Z. E., Abdurakhimov S. N., Results of Arthroplasty in Fractures of Proximal Femur in the Elderly Patients, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3409-3413. doi: 10.5923/j.ajmms.20241412.70.
1. Introduction
- As is known, for fractures of the femoral neck over the age of 60, the operation of choice is a hip arthroplasty. An osteosynthesis methods in basal, pertrochanteric and intertrochanteric fractures in this age group does not always allow achieving the desired result from the operation, which is associated with low bone mineral density, the presence of diabetes mellitus, the development of complications (hypostatic pneumonia, bedsores, etc.) [3,4,20,26]. In a young patient, and historically in all patients, osteosynthesis was considered the gold standard for fractures of the proximal femur, regardless of the nature of the fracture, but common complications that have arisen in old age with fractures of the proximal femur, including the pseudarthrosis, improperly fused fractures and aseptic necrosis of the femoral head has led surgeons to perform arthroplasty, and the number of such interventions is growing [6,7,22,24,25,27,28-30].It should be noted that after surgical treatment the number of complications and unsatisfactory functional results remains very high and reaches 30%. Reoperations after osteosynthesis in fractures of proximal femur in the elderly patients are largely associated with errors in the choice of the treatment method, violation of the method of implantation of metal structures and the operation technique, and with improper postoperative management of the patient [8,9,12,15,17,18,19,31].Consequently, when choosing surgical tactics, it seems very important to be guided not only by the nature of the fracture itself and the presence of the individual's capabilities for osseointegration after osteosynthesis against the background of osteoporosis, degenerative-dystrophic diseases of the joint and metabolic syndrome [6,7,9,27,30]. Although stable fixation of the fracture can allow the fracture to heal and return to normal function in these patients, we must be aware of the significant risks associated with attempting fracture fixation in these patients with poor bone quality. There are several evolving techniques and materials that can assist in this endeavor, although it is important to keep in mind that for some types of fractures, total arthroplasty of the joints may more quickly return these patients to their pre-traumatic level of functioning [1].In general, the results of treatment with osteosynthesis of the proximal femur in posttraumatic arthrosis are worse than in primary indications. It is not possible to fix the fracture of the femoral neck, as a rule, is the result of a significant displacement of bone fragments, poor bone quality, the patient's age, or inadequate fixation technique [26].Long-term randomized controlled trial and meta-analysis involving nearly 1200 patients. Revealed favorable outcomes in the treatment of fractures of the proximal femur, which were treated with arthroplasty in elderly patients [4].
2. Material and Methods
- In the Department of Adult Traumatology of the RSSPO of the Ministry of health of the republic of Uzbekistan, patients aged 65 years and older with fractures of the proximal femur, depending on the state of bone mineral density, the presence of degenerative changes in the hip joint and metabolic syndrome, in 102 patients were used the arthroplasty system. Of the 102 patients, the vast majority were 85 women and 17 men, aged 60 to 80 years (mean age 70 years). We observed a basal fracture of the femoral neck in 39 patients, a pertrochanteric fracture of the femur - 42, an intertrochanteric fracture - 2, a fracture of the upper third of the diaphysis - 1 (rheumatoid coxarthritis on the side of the fracture). In 89 patients with fractures of the proximal femur according to the AO / ATO classification, they were unstable.All patients in the preoperative period underwent multislice computed tomography and X-ray densitometric studies. Multislice computed tomography made it possible to determine the nature of the fracture, the choice of the femoral component of the endoprosthesis. X-ray densitometry determined the indicators of bone mineral density; at low levels (osteoporosis, osteopenia with a risk of fracture of more than 20%), osteosynthesis was excluded and the choice was in favor of hip arthroplasty. The systemic assessment of bone mineral density was carried out by the method of dual-energy X-ray absorptiometry (DEXA) on the DMS Group “Stratus” apparatus (France, 2011) according to the standard program on the proximal femur. Digital radiography of the knee joints was performed using standard ROI (regions of interest, R1-5) points in frontal and lateral projections before surgery.Based on the recommendations of the WHO experts [WHO, 1994], osteoporosis and osteopenia in dual-energy X-ray densitometry were verified by the densitometric indicator - T-criterion, where, the value of standard deviations of the T-criterion up to - 0.1 is the norm; the value of standard deviations of the T-criterion from - 1.0 to - 2.5 - osteopenia; the value of standard deviations of the T-criterion is 2.5 and below - osteoporosis. Another indicator of densitometry T-score is higher or equal - 1.0 "there is an effect", if lower - 1.0 "there is no effect". The patients observed by us had densitometric indices within the limits of osteopenia and osteoporosis. For basal fractures of the femoral neck, standard designs of the femoral component of the total hip joint endoprosthesis were used; for transtrochanteric and intertrochanteric fractures of the femur, the Wagner stem of the Zimmer revision system endoprosthesis was used with the use of cerclage and, in some cases, for stable fixation, transfragmental vinasseous osteosynthesis was performed. The technical holes on the Zweimuller stem (Zimmer alloclassic) made it possible to fix the fragments of the greater trochanter with a lavsan or to carry out a wire suture, depending on the nature of the fracture fragments. In 3 patients with severe osteoporosis, a cement version of the hip joint endoprosthesis with a revision femoral component was used. In patients with severe clinical manifestations of concomitant somatic diseases, a bipolar arthroplasty system was used in order to reduce the trauma and the time of surgery.On the third or next day after the operation, the patients were allowed to move with the help of improvised support (most often a walker) without loading the operated lower limb and to carry out active movements in the adjacent joints. Earlier, the clinic used the Wagner, Zweimuller total arthroplasty system from Zimmer (USA), these were tapered legs with distal fixation, additionally cerclage and transfragmentary screws were used. In the postoperative observation of zo patients after endoprosthetics with these systems, we noted an increase in the duration of surgery, blood loss and aggravation of the general somatic condition due to the presence of concomitant diseases, especially in patients over 70 years of age. Further, in patients who underwent arthroplasty with the use of the Wagner femoral revision system in complicated cases of inflammation, performing the second stage of arthroplasty after infection presented large technical and material costs for both the patient and the doctor. In this regard, in order to minimize surgical intervention in patients with fractures of the proximal femur in old age, it was customary to use bipolar arthroplasty systems from MERIL (India). Therefore, for comparison, patients were divided into 2 groups with this injury using total and bipolar arthroplasty in this age aspect. Total arthroplasty was performed in 48 patients, bipolar arthroplasty in 54 patients.
3. Results and Discussion
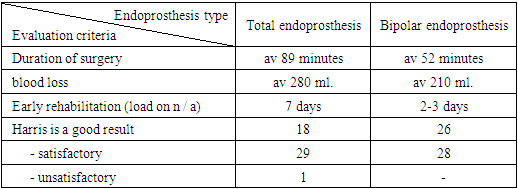
- The results of the performed surgical treatment were assessed using the Harris hip joint scale. According to this scale, with total arthroplasty using Zimmer systems (USA), good results were obtained in 18 patients, satisfactory in 29 cases and 1 unsatisfactory result (Table 1).
|
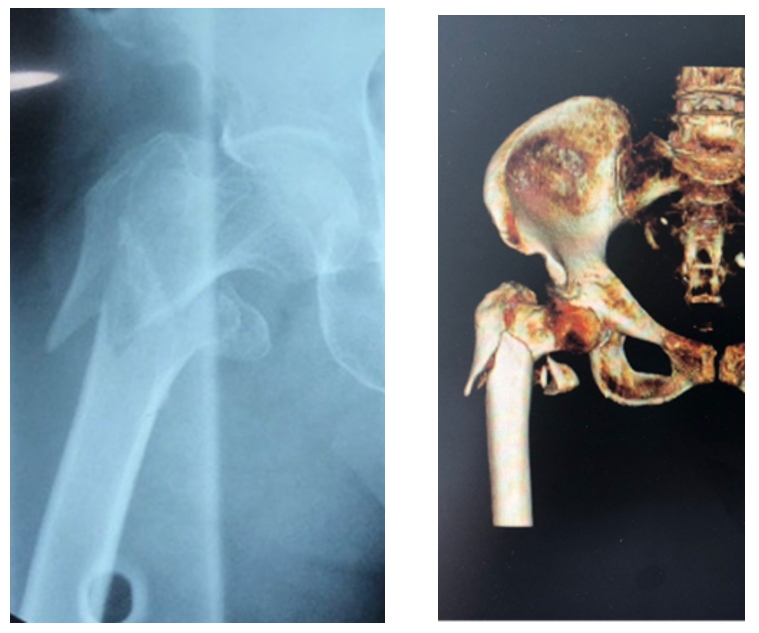 | Figure 1. X-ray and MCT of patient A.B. 78 before surgery |
 | Figure 2. Fixation of bone fragments |
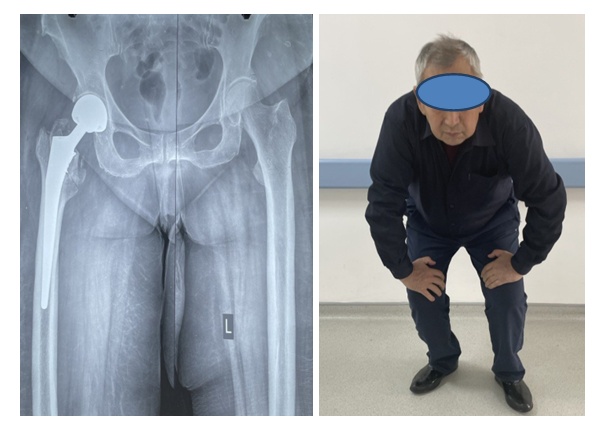 | Figure 3. Radiograph and view of the patient A.B. 78 after the surgery |
 | Figure 4. Radiograph of patient I.L. is 72 years old before surgery |
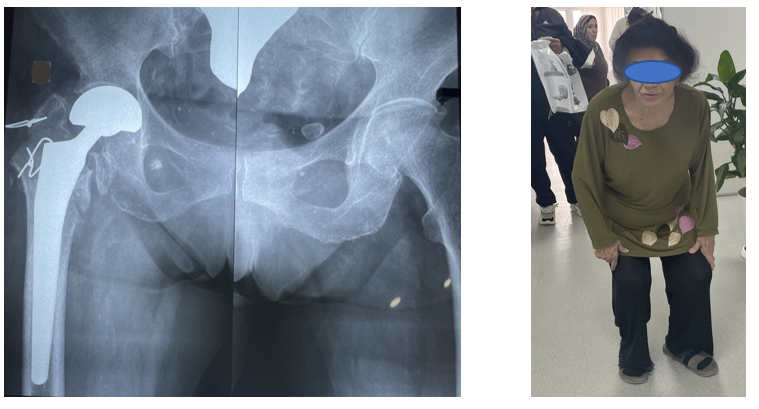 | Figure 5. Radiograph and patient view I.L. is 72 years after surgery |
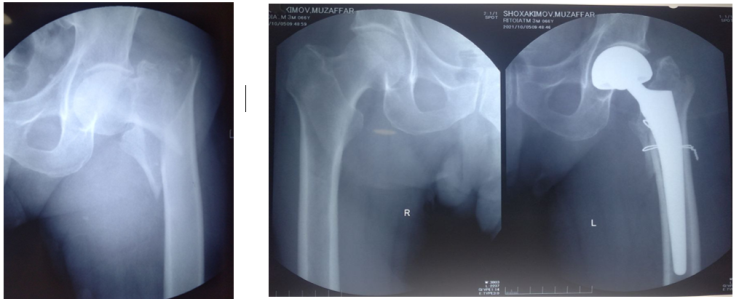 | Figure 6. Radiograph view Sh.M. 66 years old, X Ray before and after surgery |
4. Conclusions
- Endoprosthetics for fractures of the proximal femur in elderly patients is the most optimal method of surgical treatment in terms of the fastest restoration of the support ability and function of the lower limb in this category of patients. The system of femoral components of the Wagner (Zimmer) hip endoprosthesis allows stable fixation of bone fragments with cerclage and screws, but it takes more time and increases blood loss, which affects the outcomes of surgery. The use of femoral components with a bipolar head MERIL (India) in old age helps to reduce the volume and duration of surgery in patients with concomitant somatic diseases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML