-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3394-3397
doi:10.5923/j.ajmms.20241412.67
Received: Dec. 1, 2024; Accepted: Dec. 21, 2024; Published: Dec. 31, 2024

Comparative Analysis of Minimally Invasive and Traditional Surgical Methods for the Treatment of Choledocholithiasis
Tukhtaboev Bekzod1, Shengeliya G. Levan2
1Department of Faculty Surgery named after I.I. Grekov, I.I. Mechnikov State Medical University, Russian Federation
2A.A. Rusanov Department of Faculty Surgery Saint-Petersburg State Pediatric Medical University, Russian Federation
Correspondence to: Tukhtaboev Bekzod, Department of Faculty Surgery named after I.I. Grekov, I.I. Mechnikov State Medical University, Russian Federation.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

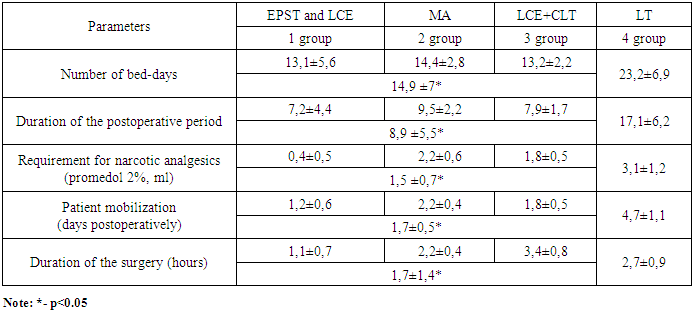
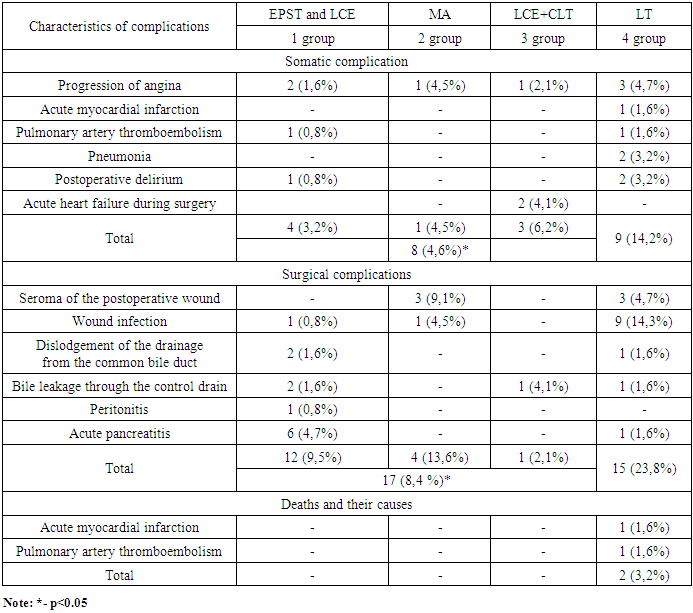
Choledocholithiasis is a common complication of gallstone disease that requires effective treatment to prevent severe complications. Modern, minimally invasive approaches, including Endoscopic Papillosphincterotomy (EPST) and Laparoscopic Cholecystectomy (LCE) offer alternatives to traditional methods. However, their comparative effectiveness needs further clarification. To evaluate the safety of four different treatments for choledocholithiasis: a two-stage approach (EPST + LCE), single-stage laparoscopic intervention, minilaparotomy and traditional open surgeries. This retrospective study included 261 patients with choledocholithiasis treated at a multidisciplinary hospital between 2013 and 2023. The patient were categorized into four groups according to the treatment methods. The analysis focused on evaluating invasiveness parameters (duration of surgery, postoperative recovery time, duration of hospitalization, and analgesic requirements) and safety outcomes (com-plication rates and mortality). Statistical analysis was conducted with a significance threshold р<0,05. A comparison of the methods revealed that endoscopic papillosphincterotomy with laparoscopic cholecystectomy (EPST+LCE) demonstrates the least traumatic: minimal operation duration (1,1±0,7 hours), early patient mobilization (1,2±0,6 days)and the lowest need for narcotic analgesics (0,4±0,5 ml). the incidence of somatic (3,2%) and surgical (9,5%) complications was also minimal. Simultaneous laparoscopic interventions showed similar effectiveness but were associated with a high conversion rate (20,8%). Minilaparotomy was characterized by longer rehabilitation time but remained a safe alternative. Traditional laparotomy procedures exhibited the highest complication rate (23,8%) and mortality (3,2%). EPST followed by LCE is the preferred method for treating choledocholithiasis due to its low invasiveness and high safety. Simultaneous laparoscopic interventions require a highly qualified surgeon. Minilaparotomy remains a reserve method, while laparotomy procedure are only justified when minimally invasive approaches are not feasible.
Keywords: Choledocholithiasis, Laparoscopy, Endoscopic papillosphincterotomy, Mini-laparotomy, Laparotomy
Cite this paper: Tukhtaboev Bekzod, Shengeliya G. Levan, Comparative Analysis of Minimally Invasive and Traditional Surgical Methods for the Treatment of Choledocholithiasis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3394-3397. doi: 10.5923/j.ajmms.20241412.67.
1. Introduction
- Choledocholithiasis remains one of the most significant challenges in contemporary abdominal surgery, not only as a common complication of cholelithiasis but also as a cause of severe, life-threatening complications such as mechanical jaundice, acute cholangitis, and biliary pancreatitis [1]. The prevalence of choledocholithiasis among patients with gallstones in the gallbladder is reported to be 10-15%, with the risk of its development increasing with age, particularly in older individuals [2]. As advancements in medical technology continue, this pathology is gaining increasing relevance in terms of selecting effective and minimally invasive treatment approaches. The primary objective in the treatment of choledocholithiasis is to restore adequate bile flow from the common bile duct, which can be achieved through various surgical and endoscopic methods. The classical approach, which involves laparotomic choledocholithotomy, remains effective but is highly invasive and associated with a high incidence of postoperative complications, particularly in the elderly population [3].The development of minimally invasive surgical techniques has led to the emergence of methods such as endoscopic papillary sphincterotomy with lithoextraction, laparoscopic cholecystectomy with simultaneous removal of stones from the common bile duct, and combined two-stage approaches. Endoscopic papillary sphincterotomy, either as a standalone procedure or in combination with laparoscopic cholecystectomy, has demonstrated high effectiveness and safety, particularly in patients with a high surgical risk [4].Simultaneous laparoscopic procedures, including cholecystectomy and stone extraction, allow for the resolution of the problem in a single stage, thereby reducing the need for repeated interventions. However, these procedures require a high level of surgical expertise and specialized equipment, which limits their applicability in certain medical institutions [5]. In a retrospective study of 1,076 patients, Totikov V.Z. et al. compared simultaneous laparoscopic treatment of choledocholithiasis with a two-stage approach, which included laparoscopic cholecystectomy and endoscopic papillary sphincterotomy. The study found no significant difference in the safety and effectiveness of the two methods, but highlighted that the outcomes of single-stage treatment were dependent on the experience and skill of the surgeon [6]. Approaches utilizing mini-access techniques represent a compromise between invasiveness and accessibility. This method provides a cost-effective alternative for the treatment of choledocholithiasis in patients with a surgical-anesthetic risk of P3-P4 and in cases where endoscopic or video-assisted surgical methods are not feasible [7]. Contemporary literature emphasizes the need for an individualized approach to treatment selection, based on the severity of the disease, the presence of comorbidities, the technical capabilities of the institution, and the qualifications of the medical staff. However, the question of which treatment method is most preferable in terms of minimizing invasiveness, accelerating rehabilitation, and reducing complication rates remains unresolved [6,8].The aim of this study is to conduct a comparative analysis of four different approaches to the treatment of choledocholithiasis, including two-stage treatment using endoscopy and laparoscopy, simultaneous laparoscopic interventions, mini-access surgeries, and traditional open procedures. This will help determine the most effective and safe treatment method.
2. Materials and Methods
- A retrospective study was conducted on 261 patients with choledocholithiasis who were treated in the surgical department of a multidisciplinary hospital between 2013 and 2023. 86% of patients were admitted on an emergency basis. Patient ages ranged from 26 to 93 years, with a mean age of 66,8±12,8 years. The female- to-male ratio 4:1. Patients were divided into four groups based on the surgical treatment method. The first group included 128 patients (49%) who underwent endoscopic papillary sphincterotomy (EPST) and laparoscopic cholecystectomy (LCE). The second group consisted of 22 patients (8.4%) who underwent mini-access (MA) surgery. The third group included 48 patients (18.4%) who underwent a one-stage method combining laparoscopic cholecystectomy and choledocholithotomy (LCE + CLT). The fourth group comprised 63 patients (24.1%) who underwent traditional open surgery through laparotomic access (LT).Mechanical jaundice was observed in 227 patients (87%). Upon admission to the hospital and during preoperative evaluation, all patients underwent routine laboratory tests, including clinical and biochemical blood analyses and a general urine test. Abdominal ultrasound (US) was performed in all cases. On ultrasound, concretions in the choledoch was visualized in 22.3% of patients. The mean diameter of the common bile duct was 12.2±3.6 mm. Fibrogastroduodenoscopy (FGDS) was performed on all patients to assess the presence of bile reflux into the duodenal lumen. Additionally, preoperative magnetic resonance cholangiopancreatography was conducted. Intraoperatively, cholangiography was performed, and postoperative fistulocholangiography was carriedout. The choice of treatment method for patients with choledocholithiasis was, in most cases, based on the preferences of the operating surgeon.To compare the different surgical treatment methods for choledocholithiasis, the following parameters were used across the four patient groups: invasiveness of the method and safety of the procedure.In determining the invasiveness of the method, the following criteria were considered: duration of the surgery, number of hospital bed-days, length of the postoperative period, need for narcotic analgesics, and the time required to mobilize patients after surgery. The concept of safety in the treatment methods included the frequency of somatic and surgical complications, as well as postoperative mortality.Statistical analysis of the clinical data was performed using Microsoft Excel 2021. This study conducted a retrospective analysis using the primary method of data extraction from patient medical records. Data comparison was performed at a significance level of p<0.05, meaning the probability of falsely rejecting the null hypothesis did not exceed 5% in each case.
3. Results and Discussion
|
|
4. Conclusions
- The use of minimally invasive surgical methods improves treatment outcomes, reduces the number of surgical complications, shortens the postoperative period, and prevents mortality.Endoscopic papillosphincterotomy combined with laparoscopic cholecystectomy is the method of choice for treating cholecystocholedocholithiasis, demonstrating the least invasiveness and postoperative complications. The two-stage treatment method should not be performed in cases of large bile duct stones, prolonged strictures, or S-shaped deformities of the distal common bile duct. The single-stage laparoscopic cholecystectomy and lithoextraction method requires advanced surgical skills, and with accumulated experience, treatment outcomes are expected to improve. In cases where laparoscopic techniques are not feasible, mini-laparotomy remains an alternative option. Laparotomy should be considered only when minimally invasive surgical methods are not applicable.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML