-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3376-3383
doi:10.5923/j.ajmms.20241412.63
Received: Dec. 6, 2024; Accepted: Dec. 26, 2024; Published: Dec. 31, 2024

Giant Meckel's Diverticulum of Thoracic Localization in Combination with Intestinal Malrotation and Cervical Spine Anomaly in an Infant: Diagnostic Challenges and Tactical Errors During the Stages of Surgical Treatment
Ergashev N. Sh., Markaev A. Y., Samatov O. S.
Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The paper presents literature data and the results of our own observations on the diagnosis and surgical treatment of 47 children with Meckel's diverticulum, who were observed in the clinics of the Department of Hospital Surgery of the Tashkent Medical Pediatric Institute in the period from 2010 to 2022. The frequency, nature of complications, and features of pathological conditions were studied. DM without pathological changes was detected during surgery in 7 (14.9%) observations as an accidental finding, in 40 (85.1%) cases it was accompanied by various complications. A case of thoracic localization of Meckel's diverticulum in combination with intestinal malrotation and anomaly of the cervical spine in an infant is presented; various difficulties and tactical errors were observed at the stages of diagnosis and treatment.
Keywords: Meckel's diverticulum, Combined anomalies, Complications, Diagnostics, Treatment
Cite this paper: Ergashev N. Sh., Markaev A. Y., Samatov O. S., Giant Meckel's Diverticulum of Thoracic Localization in Combination with Intestinal Malrotation and Cervical Spine Anomaly in an Infant: Diagnostic Challenges and Tactical Errors During the Stages of Surgical Treatment, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3376-3383. doi: 10.5923/j.ajmms.20241412.63.
Article Outline
1. Introduction
- Meckel's diverticulum (MD) is a developmental anomaly of the omphalomesenteric duct that occurs as a result of insufficient obliteration of the proximal portion of the vitelline duct. It is one of the most common congenital defects of the gastrointestinal tract and can be accompanied by various severe complications. The incidence of diverticulum is 2-3% in children of all age groups, with clinical manifestations and complications occurring in approximately 25% of cases [1,3,8,9]. This anomaly, both without visible changes and with various complications, is observed in children and adults, and is detected during laparotomy or laparoscopy, as well as during radioisotope studies and capsule video endoscopy of the gastrointestinal tract [14]. According to V.M. Timerbulatova et al. (2017), among 77 patients with complicated forms of DM, 47 patients were children aged 1 to 16 years, the remaining 30 were adult patients aged 21 to 80 years [22].Typically, DM is a protrusion of a segment of the ileum located in the abdominal cavity, having a variable length and shape, which resembles a vermiform appendix. Usually, it is localized in the abdominal cavity, within the ileum at a distance of 40-70 cm from Baugin's valve [4,10,12,18,19]. The length of the diverticulum can vary from 1-2 cm to 15-20 cm, and its diameter often reaches the width of the ileum and is considered a giant DM. The literature describes cases of giant Meckel's diverticula, up to 35 cm long and 15 cm in diameter [7,15]. Histologically, the diverticulum wall is similar to the wall of the small intestine, but the muscular layer is less pronounced. In the mucous membrane, areas of heterotopic gastric mucosa or pancreatic tissue may be found [17].In the clinical picture of DM, most researchers distinguish a triad of symptoms: abdominal pain, gastrointestinal bleeding (GIB) and intestinal obstruction. The prevalence and severity of each of them depends on the anatomical features of DM, the presence of ectopic tissues in the DM wall with different morphofunctional characteristics, the patient's age and physiological characteristics [2,10].Congenital anomalies of various organs and systems are characterized by a high degree of combination with other single or multiple developmental defects, which complicates diagnosis and the choice of optimal treatment tactics. This pathology can lead to various complications and / or serve as a cause for the formation of other pathological conditions. DM without complications is often detected during operations for pathologies of the abdominal organs. In DM, as in other developmental anomalies, there is a combination of various defects of the cardiovascular, genitourinary system, spine and spinal cord, or an association in the form of a triad of diaphragmatic hernia, intestinal malrotation, heterotopia of pancreatic tissue (HPT) in parts of the gastrointestinal tract or in Meckel's diverticulum itself [6-20,23-24]. Parkash Mandhan et al. 2014 described a case of a combination of diaphragmatic hernia DG with Meckel's diverticulum and HPT in the wall of the jejunum in a newborn, designating this pathology as a triad: congenital diaphragmatic hernia (DG), DM and HPT. In 2016, L. Basani et al. reported a combination of congenital DG with DM and intestinal malrotation in a three-month-old child, which was the first description of such an association. Migration of organs through the diaphragm is more often observed on the left side with non-closure of the Larrey fissure, less often on the right side with a Morgagni defect. Usually, the DM moves together with other abdominal organs, either in a small volume or significantly, which can lead to pronounced respiratory-hemodynamic or gastroenterological disorders [5,21,23].Purpose of the Study: was to determine the characteristic features of the clinical course of DM, the difficulties of diagnosis in case of atypical localization of Meckel's diverticulum in a child with intestinal malrotation and spinal anomaly in an infant.
2. Material and Methods of the Study
- From 2010 to 2022, 47 children with DM, which caused complications and diseases that required surgical intervention, were observed in the clinical bases of the Department of Hospital Pediatric Surgery of TashPMI. In 7 (14.9%) patients, DM without pathological changes was detected during operations performed on the abdominal organs for appendicitis: in 4 patients; with malformations of the anterior abdominal wall - 2; inguinoscrotal hernia - in 1. Among the patients, there were 32 (68.1%) boys and 15 (31, 9%) girls. Pathology was detected in 6 (12.8%) children under 3 months, from 3 months. up to 1 year - in 4 (8.5%), from 1 year to 3 years - in 8 (17%), from 3 to 7 years - in 8 (17%), from 7 to 12 years - in 12 (25.5%) and from 12 to 18 years - in 9 (19.1%). This report analyzes diagnostic and operational-tactical errors, complications that arose in a patient with atypical localization of the apical and middle part of the DM in the chest cavity through a diaphragmatic defect on the right, and its base originating from the ileum in the abdominal cavity. At the diagnostic stages, laboratory, instrumental, ultrasound, radiation, as well as endoscopic and histomorphological studies were used.
3. Results and Discussion
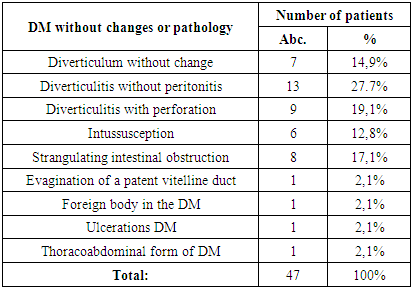
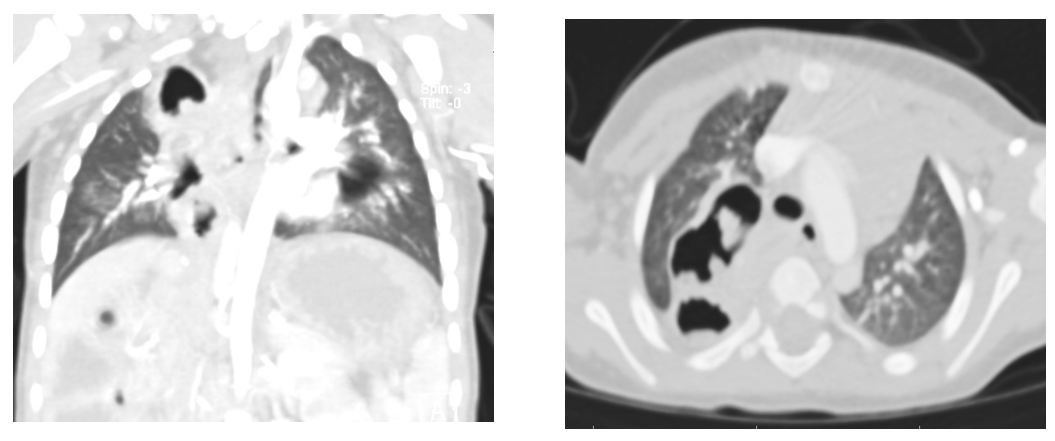
- No specific clinical manifestations were observed in uncomplicated DM. The remains of the rudimentary vitelline duct in the form of a fixed cord of Meckel's diverticulum with the umbilicus or mesentery caused intestinal volvulus and intestinal compression with the manifestation of symptoms of intestinal obstruction (Table 1).
|
|
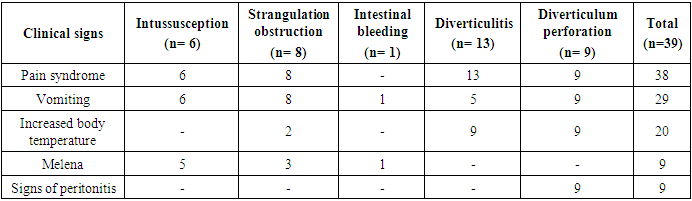
 | Figure 1. General chest radiography. Cystic formation in the projection of the right lung |
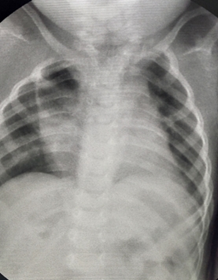
 | Figure 2. MSCT (description in text) |
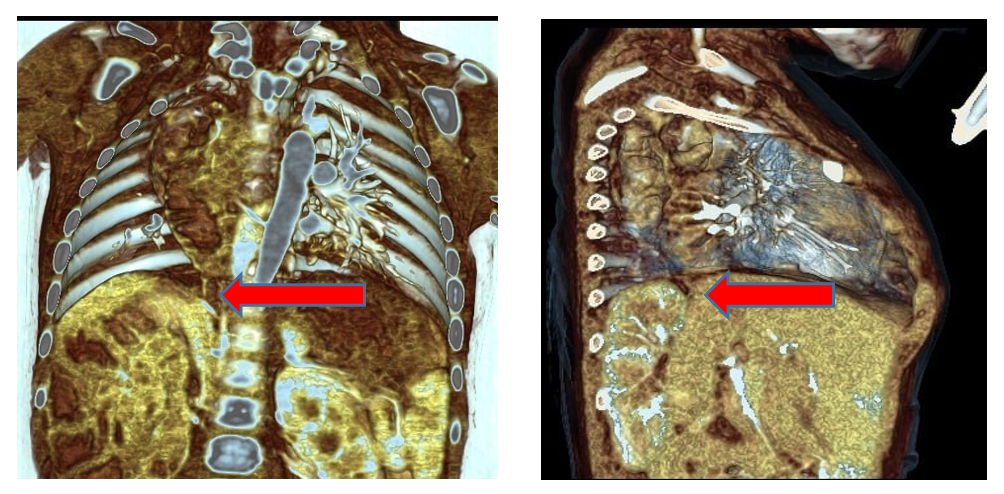 | Figure 3. MSCT angiography. A defect is determined in the projection of the posterior triangle of the right dome of the diaphragm and the displacement of intestinal loops into the chest cavity |
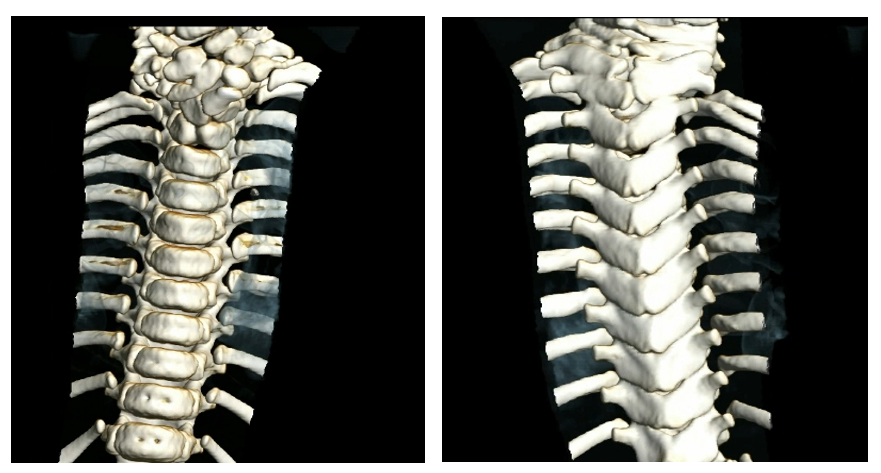 | Figure 4. MSCT of the cervicothoracic spine. Description in text |
 | Figure 5. Contrast irrigography, left-sided location of the colon |
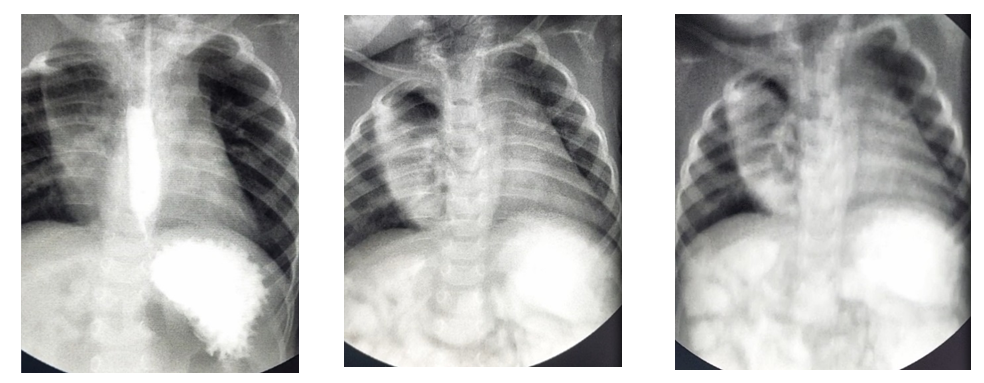 | Figure 6. Passage through the gastrointestinal tract. Description in the text |
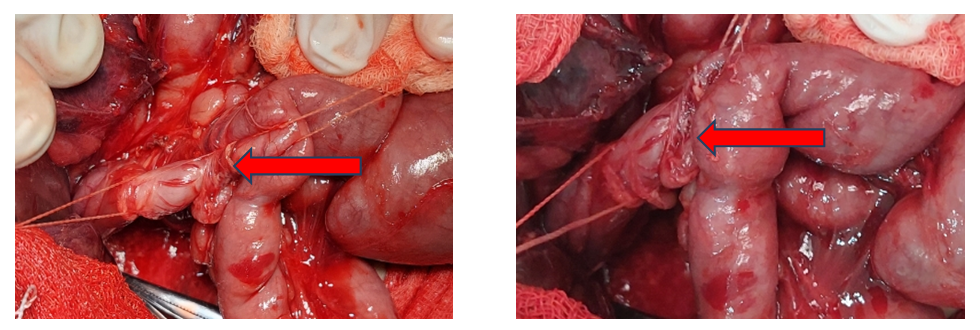 | Figure 7. Meckel's diverticulum originating from the wall of the ileum |
 | Figure 8. Resected section of small intestine carrying DM |
4. Conclusions
- In conclusion, it is important to note that Meckel's diverticulum (MD) as a congenital anomaly of the gastrointestinal tract is often detected during surgical interventions. Its frequency is 2-3%, while clinical manifestations and complications are observed in 25% of cases. In the clinical picture of the pathology, a triad of symptoms can be distinguished: abdominal pain, gastrointestinal bleeding (GIB) and intestinal obstruction of varying severity. The absence of pathognomonic signs of DM creates significant difficulties in diagnosis. DM is often combined with malformations of individual organs or is an association of various anomalies of other organs and systems, which aggravates their course. In recent publications, there is an increase in the descriptions of such combinations. Mandatory resection of both pathologically altered and intact DM is the main surgical tactic, since the risk of subsequent complications is incommensurate with simple diverticulectomy. The main method of treating DM is diverticulectomy. The options for its implementation and the types of simultaneous interventions depend on the severity and prevalence of the inflammatory process in the wall of the ileum and the diverticulum itself, as well as on the nature of the complications and secondary pathology from the peritoneum and abdominal organs."
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML