-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3322-3327
doi:10.5923/j.ajmms.20241412.52
Received: Nov. 8, 2024; Accepted: Nov. 27, 2024; Published: Dec. 28, 2024

Surgical Aspects of Ventral Hernia Treatment
Abduraxmanov Diyor Shukurullayevich
Samarkand State Medical University, Uzbekistan
Correspondence to: Abduraxmanov Diyor Shukurullayevich, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The results of treatment of 107 patients with postoperative ventral and recurrent hernias, which were performed plastic hernial defect With using onlay And sublay methods, A Also With using separation plastics With restoration normal topographic anatomy. The results of perioperative monitoring of intra-abdominal pressure at W 3- W 4 ≥ 11 justify the priority of posterior separation hernioplasty, at <11 it is possible to perform anterior separation plastic surgery. The algorithm for choosing the method of standard (onlay, sublay) or separation (anterior, posterior) plastic surgery for postoperative ventral hernias W 2, W 3, W 4 is based on the state of the muscular-aponeurotic structures of the anterior abdominal wall and the indicator of intraoperative monitoring of intra-abdominal pressure.
Keywords: Postoperative ventral hernia, Surgical treatment, Separation prosthetic plastic surgery
Cite this paper: Abduraxmanov Diyor Shukurullayevich, Surgical Aspects of Ventral Hernia Treatment, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3322-3327. doi: 10.5923/j.ajmms.20241412.52.
Article Outline
1. Relevance
- Despite the fact that in recent years All more often steel be used minimally invasive methods operational interventions in surgical diseases of the abdominal organs, The incidence of postoperative hernias remains high [10,16]. According to data rows authors, frequency development postoperative The incidence of ventral hernia (VH) after laparotomy reaches up to 20% of cases. After conducting emergency operations, the incidence of POVG development ranges from 18.1 to 58.7% of cases, with this celebrated prevalence median hernias [3,5,8,11,15].On today day questions use alloplasty at postoperative ventral hernias more and more attention is being paid to And conditioned by necessity conducting more deep research V in this direction. First of all, it is concerns questions relatively choice Togo or other method plastics And warnings development complications with sides postoperative wounds [1,4,6,12,17].It is worth noting that today there is no universal method surgical interventions. So at open methods hernioplasty results surgical treatments And frequency development postoperative complications vary And depend from places establishments synthetic material V fabrics abdominal walls, So called methods «sublay», «inlay», "onlay". Except Togo, frequency development postoperative complications depend Also And from size hernial gate, states local fabrics And working with them [2,7,9,13,14].Target research. To optimize the tactical and technical aspects of the use of anterior and posterior separation prosthetic hernioplasty in patients with postoperative ventral hernias.
2. Material and Methods of the Study
- The results of treatment of 107 patients operated on at the Department of Surgery of the Faculty of Postgraduate Education of the Samarkand State Medical University were studied. period With 2018 By 2022 years. In patients With postoperative ventral and recurrent hernias was produced plastic hernial defect With using onlay And sublay methods, A Also With using separation plastics.All patients were divided into 2 groups depending on the method used operations.IN the first group entered 51 sick, at which hernioplasty was carried out open ways With using separation plastic surgery and was divided into 2 subgroups: - 1.1 group of 29 patients who underwent anterior separation prosthetic plastic surgery and 1.2 group with the use of back separations muscles abdominal walls. The second one group (comparative) compiled 56 sick, at which were used standard methods hernioplasty By type onlay (n=38) And sublay (n=18).All patients were divided into separate subgroups according to classifications European societies herniologists (EHS, 2009) table 1).
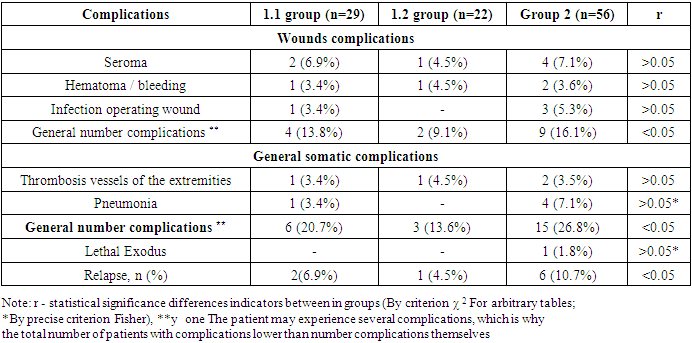
|
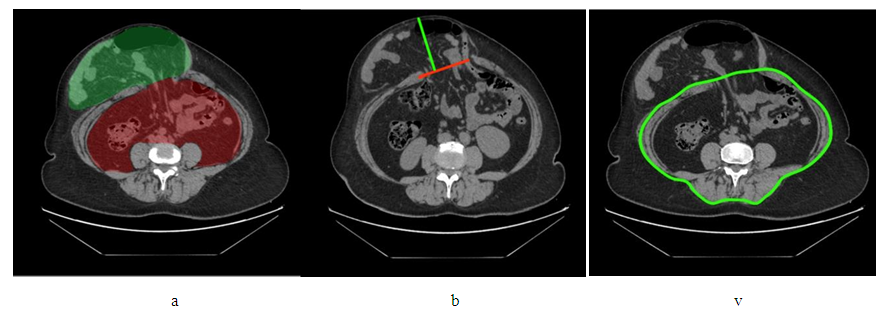 | Figure 1. Scheme for measuring CT dimensions: a – volumes of the hernial sac and abdominal cavity, b - the size of the hernial orifice and hernial bag, V - circles abdominal walls |
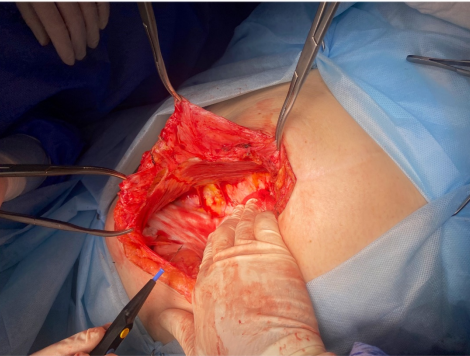 | Figure 2. Stage of separation of the rectus muscle |
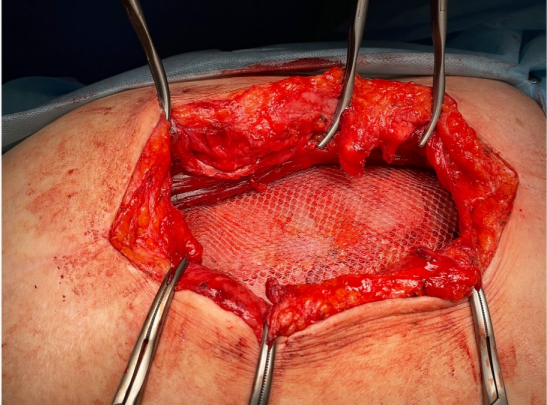 | Figure 3. Positioning of the mesh implant |
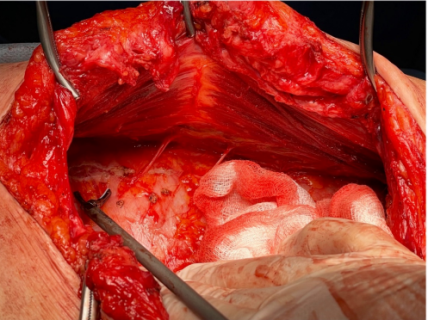 | Figure 4. Stage of separation of the rectus muscle |
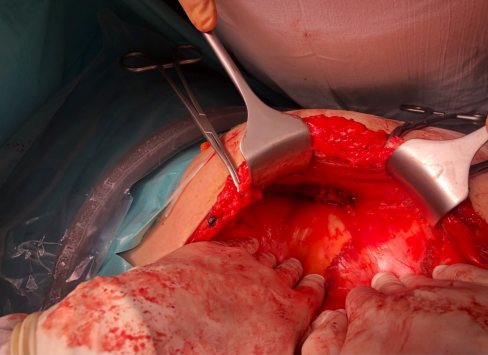 | Figure 5. Stage of intersection of the transverse muscle |
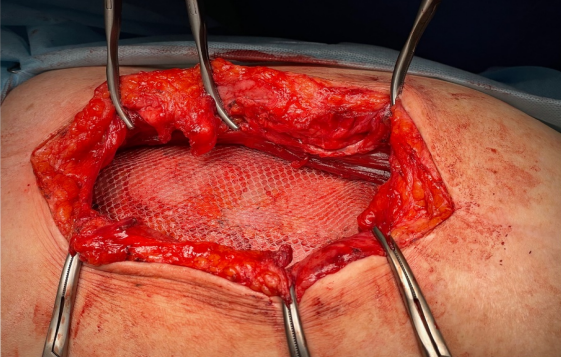 | Figure 6. Positioning of the mesh implant |
3. Results and Their Discussion
- The main point influencing the choice of the method of operation in patients all 3-x observed groups, were indicators intraoperative studies of the level of intra-abdominal pressure.At measurement original indicators intra-abdominal pressure at the patients we observed had a direct relationship between these indicators and the size of the hernial orifice (p<0.05). In this case, the achievement of these values of the threshold level of the first degree was not observed intra-abdominal hypertension (12-15 mm rt. Art.), average meanings VBD compiled 10.8±1.3 mm Hg At measurement VBD after intelligence edges hernial gate at patients With hernias W2 was observed some increase in IBP indicators relative to their initial values - up to 8.5±0.8 mm Hg, while the resulting difference in the indicators had no statistical significance significance (p>0.05). U patients With hernias dimensions W3 at information a reliable increase in IAP indicators was observed at the edges of the hernial orifice to a level corresponding to stage I intra-abdominal hypertension, which V average were composed 12.8±1.9 mmHg (p<0.05), A at patients With hernias dimensions W4 level intra-abdominal pressure after intelligence edges hernial gate turned out to be reliably higher, how at patients With hernias W3, And V average They were composed 14.7±1.7 mm Hg (p<0.05), What corresponded top border I degrees intra-abdominal pressure.Results control research level VBD, conducted V postoperative period, showed, What By measure termination actions muscle relaxants funds And departures sick from actions anesthesia was observed significant increase level VBD. So, at patients With hernias of size W3, the level of intra-abdominal pressure on the first day after surgery on average increased to 15.2±1.5 mm rt. Art., preserving To 3rd per day observations on level 14.8±1.8 mm rt. Art. (p<0.05), What corresponds I degrees intra-abdominal hypertension. U patients With hernias dimensions W4 V 1st day postoperative period noted increase level VBD to 16.7±4.2 mm rt. Art., What corresponded II degrees intra-abdominal hypertension, and by the 3rd day after the operation, some decrease was observed level VBD to 14.6±2.8, What corresponded I degrees intra-abdominal hypertension. Only in patients with hernias of W2 size, regardless of used method hernioplasty, Not were observed statistically significant differences in IAP parameters measured on the first day after surgery And after intelligence edges hernial gate (p>0.05), at this To 3rd per day postoperative period, a return of IAP indicators was noted closer To original values.Some other painting observed at monitoring level VBD V postoperative period at sick With big hernias, corresponding to W3 and W4, which used separation methods hernioplasty. At measurement intra-abdominal pressure after intelligence a reliable increase in IAP indicators was observed at the edges of the hernial orifice relatively its original values. In the 1st day of the postoperative period, some decrease in IAP indicators was observed, which by the 3rd day after operations already were approaching To original values (p<0.05).Like this in this way, according to results research level VBD V perioperative period, when choosing the standard method of hernioplasty in patients With hernias W3 And W4 it is forbidden rely on indicators VBD, measured after the edges of the hernial orifice are brought together. This is due to the fact that in in the postoperative period, the IBP indicators will be significantly higher, since sick in time conducting operations located under anesthesia And under action muscle relaxants funds. Results perioperative monitoring intra-abdominal pressure testify O tension character onlay And sublay methods hernioplasty, V connections With how their usage at hernias dimensions W3 And W4 not recommended. IN That same time confirmed non-tension character separation ways hernioplasty.Based on the results we obtained research we proposed our algorithm for choosing a method of hernioplasty in patients with median hernias dimensions W2-W4.IN case applications separation methods hernioplasty the condition of the tissues was assessed, primarily the rectus abdominis muscles, which had an effect influence on choice method plastics By degrees reconstruction normal anatomy front abdominal walls.There is a great danger when performing operations on patients with ventral hernias represents development syndrome intra-abdominal hypertension (SIAG), emerging By reason So called "non-accommodation". At this complication V the first queue arise disorders with sides respiratory And caridovascular systems.For prevention SIAG after execution plastics, establishments endoprosthesis, intra-abdominal pressure is measured. In case of increased IAP up to II-III degree to reduce it during surgical intervention produce total intubation thin intestines by way transnasal And transanal introductions probes. WITH with help such methods succeeded achieve reductions level VBD to lower borders norms. At this preference should give oneself up back separation hernioplasty.After the operation, the level of intra-abdominal pressure was examined, after which the patient was dressed bandage. IN 1.1 group sick indicators intra-abdominal pressure varied from 4 to 23 mm Hg, averaging 8.6±1.4 mm Hg. In patients of group 1.2, IAP indices ranged from 6.8 to 17 mm Hg, with average value of 8.2±0.7 mm Hg. In patients of group 2, the data The indicators ranged from 7.2 to 19 mm Hg, averaging 9.4±1.8 mm Hg. r t. Art. (p<0.05).Analysis results surgical treatments sick With POG V in the immediate postoperative period was carried out within 30 days after surgical interventions, distant results surgical treatments at data patients were studied V term from 12 to 36 months.U patients 1.1 groups V nearest postoperative period after surgery using anterior separation plastic surgery of wounds complications arose V 4 (13.8%) cases. IN 1.2 group sick, at which was used back separation plastic, similar wounded complications were noted in 2 (9.1%) patients over 60 years of age with epigastric hernia of large size and the presence of obesity. In patients 2 groups, at which were used standard tension methods hernioplasty, wound complications were observed in 9 (16.1%) cases. Thus, thus, wound complications less often were observed V 1.2 group of patients, where posterior separation plastic surgery was used – in 9.1% of cases (table 2).
|
4. Conclusions
- 1. The results of postoperative monitoring of intra-abdominal pressure at W 3- W 4 ≥ 11 justify the priority of posterior separation hernioplasty; at <11, anterior separation hernioplasty can be performed.2. The algorithm for choosing a method of standard (onlay, sublay) or separation (anterior, posterior) plastic surgery for postoperative ventral hernias W 2, W 3, W 4 is based on the state of the muscular-aponeurotic structures of the anterior abdominal wall and the intraoperative monitoring indicator of intra-abdominal pressure.3. Optimization of the tactical and technical aspects of surgical treatment of patients with postoperative ventral hernias made it possible to reduce the frequency of immediate postoperative complications from 16.1% to 9.1% and recurrence from 10.7% to 4.5% (p<0.05).Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML