-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3224-3226
doi:10.5923/j.ajmms.20241412.28

Dynamics of the Wound Process After Hemorrhoidectomy
Xujabaev S. T.1, Rakhmatov B. H.2
1Doctor of Medical Sciences, Associate Professor of the Department of General Surgery, Samarkand State Medical University, Samarkand, Uzbekistan
2Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

224 patients with chronic internal and combined hemorrhoids were included in this study. The main group included 122 patients. The correction of chronic hemorrhoids in them was performed in a minimally invasive way using a hardware-controlled bipolar electrosurgical LigaSure unit. The control group consisted of 102 patients operated on by the traditional Milligan-Morgan surgical method. The use of bipolar vascular electrocoagulation LigaSure in the treatment of chronic hemorrhoids makes it possible to achieve rapid wound repair, compared with traditional hemorrhoidectomy, as a result of which the rehabilitation period is shortened.
Keywords: Chronic hemorrhoids, Surgical treatment, Wound repair
Cite this paper: Xujabaev S. T., Rakhmatov B. H., Dynamics of the Wound Process After Hemorrhoidectomy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3224-3226. doi: 10.5923/j.ajmms.20241412.28.
Article Outline
1. Introduction
- The treatment of patients with hemorrhoids remains one of the most urgent problems of coloproctology. For centuries, surgeons have been working on the problem of treating chronic hemorrhoids [1,6]. To date, the most common operation remains aimed at excision of three hemorrhoids, proposed by E. Milligan and G. Morgan back in 1937. In the world proctological practice, there are many surgical methods for the treatment of chronic hemorrhoids [3,7]. However, none of them can be considered fully optimal, devoid of the risk of developing both early and late postoperative complications. The interest of coloproctologists in new methods of hemorrhoidectomy is confirmed by the number of publications on this topic.New technologies in recent years have significantly improved the quality of surgical methods for the treatment of hemorrhoids [2,5]. Nevertheless, the question of the most optimal variant of surgical intervention remains unresolved to date, and data on the effectiveness of various techniques are often contradictory [4,8].In this regard, the need to develop new methods of surgical correction of chronic hemorrhoids served as the basis for this work.The purpose of the study. To study the features of the course and repair of wounds after traditional methods of hemorrhoidectomy and according to the proposed technique using bipolar electrocoagulation in chronic hemorrhoids.
2. Research Materials and Methods
- This study included 224 patients with chronic internal and combined hemorrhoids who were treated between 2018 and 2023.All patients (n=224) were divided into two groups. The first, main (prospective) group included 122 patients. The correction of chronic hemorrhoids in them was performed in a minimally invasive way using a hardware-controlled bipolar electrosurgical LigaSure unit. The second, control (retrospective) group consisted of 102 patients with the same diagnosis, but operated on by the traditional Milligan-Morgan surgical method in the II modification of the SSC Coloproctology of the Ministry of Health of the Russian Federation.In order to study the dynamics of the wound process, along with clinical ones, cytological and microbiological studies of the wound discharge were performed.
3. The Results and Their Discussion
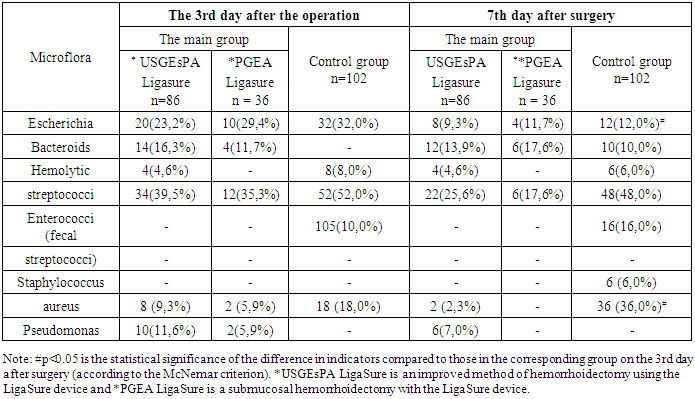
- In smears on the third day after surgery, when studying the dynamics of the wound process in 52 (60.4%) patients of the main group after performing an improved method of hemorrhoidectomy using the LigaSure device and in 12 (35.3%) patients who underwent submucosal hemorrhoidectomy with the LigaSure device, a moderately pronounced inflammatory reaction of neutrophilic character. Single nuclear histiocytes of monocytic cells (the first signs of the onset of repair) were also noticeable in 20 (23.2%) and 12 (29.4%) patients of this group, respectively. In addition, in 4 (11.7%) patients of the main group who underwent submucosal hemorrhoidectomy with the LigaSure device, large histiocytes with basophilic cytoplasm (cellular signs of active repair) are visible in the smears. At the same time, in the control group, 72 (72%) people had a pronounced inflammatory reaction (an increase in the number of eosinophils, mononuclear lymphocytes, monocytes).On the fifth day in 62 (72.0%) patients after performing an improved method of hemorrhoidectomy using an apparatus. LigaSure and in 24 (70.6%) submucosal hemorrhoidectomy with LigaSure apparatus of the main group, an increase in the number of eosinophils was revealed, neutrophilic leukocytes were visible, lymphocytes and monocytes were found in small numbers. At the same time, the vast majority of patients in the main groups showed a decrease in the number of neutrophils. They showed the first signs of reparation. On the seventh day after surgery, a large number of collagen fibers and an accumulation of immature epithelium were detected in smears in 44 (51.2%) and 16 (47.0%) people of the main group. Immature squamous epithelium and fibroblasts were detected in 4 patients (11.7%) after submucosal hemorrhoidectomy with LigaSure apparatus. In the control group, at the end of the first week, 78 (58%) patients showed a decrease in the number of neutrophils, only 12 (12%) showed the first signs of repair (single histiocytes are visible), and 8 (8%) patients showed signs of active repair (large histiocytes with basophilic cytoplasm). On the 10th day of the postoperative period, immature squamous epithelium and fibroblasts were detected in the field of vision in most patients of the main group, in 28 (32.5%) - mononuclear cellular elements of blood origin - lymphocytes and monocytes. In 24 (27.9%) patients after performing an improved method of hemorrhoidectomy using the LigaSure device and in 16 (47.0%) patients after submucosal hemorrhoidectomy with the LigaSure device of the main group, initial signs of granulation tissue formation appeared (single single-core histiocytes are noticeable). At the same time, 54 (54%) patients of the control group had a large number of neutrophils, phagocytic macrophages. In 12 (12%) patients, loose fibrous connective tissue (fibrous cords) was differentiated, in 14 (14%) - a decrease in the number of neutrophils and residual elements of inflammation.On the 14th day after surgery, elements of scar connective tissue (fibroblasts and fibrocytes) were detected in all cases in the main group. While in the control group, most patients (in 66% of cases) had a moderate amount of collagen fibers, an accumulation of immature squamous epithelium.On day 20, in 78 (90.7%) patients of the main group, after performing an improved method of hemorrhoidectomy using the LigaSure device and in all patients after submucosal hemorrhoidectomy with the LigaSure device, loose fibrous connective tissue was detected in smears. Whereas in the control group, only 34 (34%) patients had elements of loose fibrous connective tissue, 14 (14%) had residual elements of inflammation.The data of clinical and cytological studies were verified with the results of microbiological studies. As a result of the examination of the smear from the anal canal before the operation, various kinds of microorganisms were found. Fecal streptococci prevailed among them (in 35.7% and 22.2% of the main group and in 48% of the control group). All isolated organisms belonged to the group of episodically occurring or accidental, transient for the microflora of the surgical wound (Table 1).
|
4. Conclusions
- 1. Improved methods of hemorrhoidectomy using "LigaSure" at the stages of surgery for chronic hemorrhoids are highly effective, pathogenetically sound and radical methods that can improve both the immediate and long-term results of the operation.2. The use of bipolar vascular electrocoagulation "LigaSure" in the treatment of chronic hemorrhoids makes it possible to achieve rapid wound repair, compared with traditional hemorrhoidectomy, as a result of which the rehabilitation period is shortened.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML