-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3213-3219
doi:10.5923/j.ajmms.20241412.26
Received: Nov. 10, 2024; Accepted: Dec. 3, 2024; Published: Dec. 16, 2024

Results of Knee Joint Replacement with an Endoprosthesis of Our Own Design
Abdikarimov X. G.1, Gafur-Akhunov M. A.2, Davletov R. R.1, Nasirov S. K.3, Nurjabov A. I.4, Asamedinov N. K.4, Sadriddinov Sh. O.1, Sultonov B. B.1, Fayziev F. Sh.3
1Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology, Tashkent, Uzbekistan
2Center for Development of Professional Qualifications of Medical Workers, Tashkent, Uzbekistan
3Tashkent Medical Academy, Tashkent, Uzbekistan
4Tashkent State Dental Institute, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Malignant tumors predominantly affect the distal femur and proximal tibia, accounting for approximately 60% of primary skeletal tumors. This study evaluates the outcomes of knee joint reconstruction using a domestically designed endoprosthesis, addressing the limitations posed by high costs of foreign-made implants. The research encompasses 21 patients aged 16–38 with malignant bone tumors, treated at the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology. Preoperative diagnostics included CT, MRI, and biopsy to assess tumor extent and histological features. Post-resection, a custom-designed fixed-hinge titanium endoprosthesis was implanted, yielding excellent functional outcomes in most cases. Complications included aseptic loosening in two patients and one instance of local tumor recurrence. The study highlights the feasibility and efficacy of local endoprosthesis designs, reducing dependence on costly imports and advancing organ-preserving oncology practices.
Keywords: Malignant bone tumors, Endoprosthesis, Osteosarcoma, Organ-preserving surgery, Bone tumor reconstruction, Onco-orthopedic innovations
Cite this paper: Abdikarimov X. G., Gafur-Akhunov M. A., Davletov R. R., Nasirov S. K., Nurjabov A. I., Asamedinov N. K., Sadriddinov Sh. O., Sultonov B. B., Fayziev F. Sh., Results of Knee Joint Replacement with an Endoprosthesis of Our Own Design, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3213-3219. doi: 10.5923/j.ajmms.20241412.26.
Article Outline
1. Introduction
- The bones that form the knee joint are most frequently affected by malignant tumors - the distal metaphysis of the femur and the proximal metaphysis of the tibia. This area accounts for about 60% of primary tumors [5,6,13,17]. Until the end of the 70s of the last century, the method of treating tumors of this localization was considered to be surgical and mainly mutilating (amputation and disarticulation) operations were performed. The prognosis for patients with these tumors was unfavorable. The survival rate of patients with osteosarcomas and Ewing's sarcomas did not exceed 10%. With the introduction of chemotherapy, a combined approach to the treatment of malignant bone tumors appeared. The development of effective chemotherapy regimens, progress in bioengineering and surgical techniques made it possible to perform organ-preserving operations and endoprosthetics [7,8,10,14]. The risk of limb amputation has decreased more than 3 times: from 23% in 1980 to 7.4% at present [11,12]. Life expectancy and duration of the relapse-free period after The outcomes of organ-preserving operations, provided adequate resection is performed, are similar to those after amputation. Today, the standard for organ-preserving surgery for limb tumors is endoprosthetics. [2,16]. The first person in the world to develop and implement an all-metal total hip joint endoprosthesis and a linked knee joint endoprosthesis was Konstantin Mitrofanovich Sivash in 1956. Subsequently, together with S. T. Zatsepin, he developed oncological versions of these endoprostheses. [1]. This endoprosthesis was the starting point for a new direction in reconstructive surgery for tumor lesions of the bones that form the knee joint, saving the functioning limb of thousands of patients. served as a prototype for many designs that are still used today (3]. In the 1980s, the pioneer of Russian onco-orthopedics N.N. Trapeznikov advised performing organ-preserving surgeries only for strict indications, taking into account the biological characteristics of the tumor: the degree of anaplasia, growth rates, and tendency to metastasize [2]. One of the founders of foreign onco-orthopedics can be considered Henry Jaffe, who published his work “Tumors and Tumorous Conditions of Bone and Joints” in 1958. In the 1970s, the Benoit-Gerrard Company (Caen. France) developed prostheses with a fixed joint and adapted them to segmental reconstruction of resected bone. In the first half of the 1980s, rotational knee and hip prostheses appeared. In the last 30 years, modular endoprostheses have been widely used to reconstruct resected bone segments. Today, these are standard of organ-preserving treatment for patients with bone tumors [18]. The advantage of endoprosthetics after resection of the articular end with a tumor, in contrast to other reconstruction methods, is the one-stage compensation of massive bone defects by the implant while maintaining the support capacity and movements in the joint, which ensures optimal restoration of function and a higher level of quality of life for the patient, expanding the possibility of self-care and continuation of complex treatment [4]. Despite the significant successes achieved in the development of surgical intervention techniques using various designs of endoprostheses for oncological orthopedics, the search for an “ideal endoprosthesis” that meets all the requirements of modern oncoorthopedics continues, as evidenced by many publications [2,7,8,15]. In Uzbekistan, 320-350 patients with primary bone tumors are diagnosed per year. The incidence rate is 1.0 per 100 thousand people, which corresponds to global indicators [9]. Only 15-20 endoprosthetics of the knee joint and its constituent bones are performed annually. Considering that more than half of primary skeletal tumors occur in the bones that form the knee joint, the actual number of patients who need these surgeries is several times greater. In knee joint endoprosthetics, we use foreign-made devices, the cost of which, depending on the manufacturer, ranges from 30 to 60 million sum. Due to the high cost, not all patients have the opportunity to purchase an endoprosthesis. Therefore, organ-preserving operations with reconstruction and restoration of the knee joint are performed on a limited number of patients. The development and implementation of a new domestic endoprosthesis for replacing defects of the distal end of the femur, knee joint, proximal end of the tibia is certainly a solution to an important medical and social problem.The aim of the study. To analyze the results of reconstructive surgical interventions on the knee joint using a new endoprosthesis of our own design.
|
2. Materials and Methods of the Study
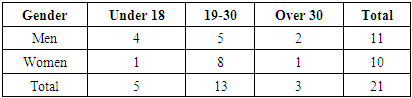
- The study included 21 patients with tumors of the distal femur and proximal tibia undergoing treatment in the surgical department of tumors of the musculoskeletal system of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology "RSSPMCOR". Of these, 11 were men and 10 were women aged 16 to 38 years (Table 1).Biopsy of the pathological lesion and pathomorphological examination were the final stage of the examination. In the preoperative period, the diagnosis was verified clinically, radiologically and morphologically in all patients.According to the examination, in 17 patients the tumor was localized in the distal femur and in 4 in the proximal tibia. According to the X-ray examination data: in 6 cases there was a lesion of the epiphyseal region spreading to the metaphysis, and in the remaining 15 cases - a lesion of the metadiaphyseal region of the bone; in 10 cases osteolytic, in 5 - osteoblastic and in 6 - mixed forms of the tumor were detected; on 15 radiographs, various types of periosteal reactions were determined. For the purpose of morphological verification, an open biopsy of the tumor was performed in all patients. Osteosarcoma was verified in 12 patients, giant cell tumor in 3, chondrosarcoma in 1, fibroma and xosarcoma in 1, adamantinoma in 1, Ewing's sarcoma in 1 and a malignant variant of GCT in 2 (Table 2). In 9 patients with malignant tumors, grade III malignancy was determined, in 5 - II.
 | Table 2. Distribution by localization and histological structure |
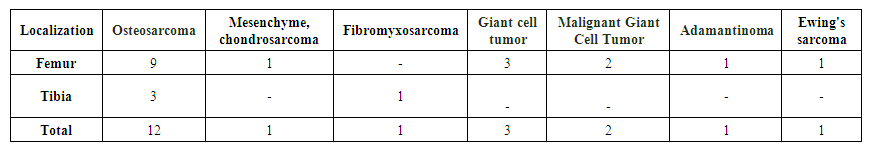
 | Figure 1. General view of the knee joint endoprosthesis of a new design |
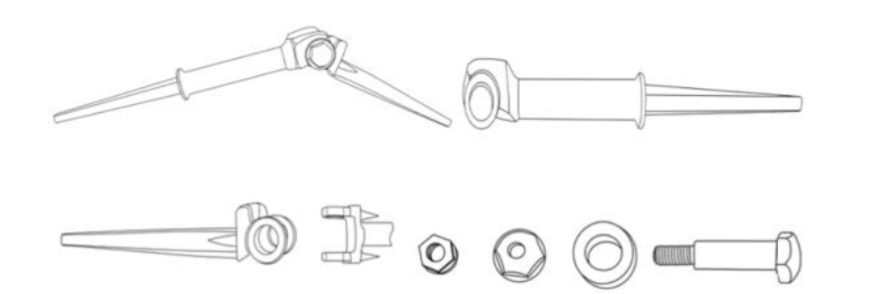 | Figure 2. Schematic drawing of the knee joint endoprosthesis of a new design |
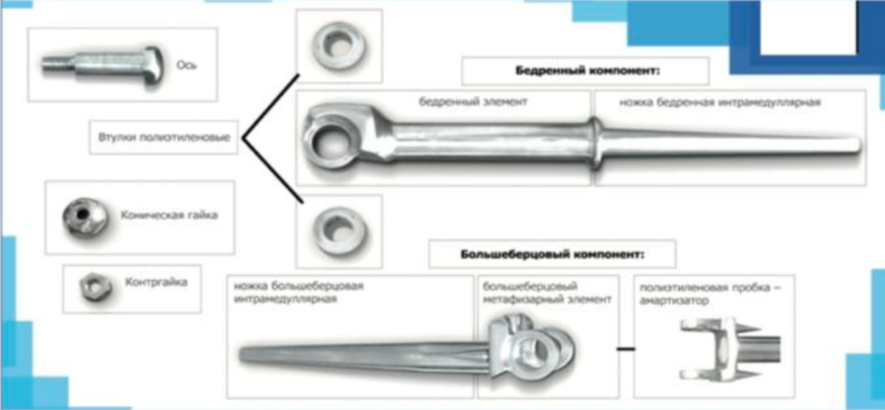 | Figure 3. Components of a new design knee joint endoprosthesis |
3. Results
- The duration of operations is 90-180 minutes. There were no intraoperative complications. Average blood loss was 500 ml. The endoprosthesis installation was performed without technical difficulties; all patients achieved adequate replacement of post-resection defects, which demonstrates the correctness of preoperative planning and the accuracy of the calculated sizes. Primary wound healing was achieved in all cases. The observation periods ranged from 13 months to 5 years. In the late period, aseptic instability of the endoprosthesis stem developed in two patients (9.5%). In the first case, 8 months after revision surgery for a previously installed metal-cement spacer in a patient diagnosed with osteosarcoma of the distal metadiaphyseal part of the right femur G3 T2N0M0, condition after combined treatment (4 courses of neoadjuvant chemotherapy + resection of the distal femur with installation of a spacer + 5 courses of adjuvant chemotherapy). When analyzing this case, we came to the conclusion that the predisposing factors for instability were the large length of the post-resection defect (24 cm) and, as a consequence, the short medullary canal of the femoral stump, into which the endoprosthesis stem was installed. In the second patient, after 52 months. Loosening was detected clinically and confirmed under fluoroscopic control. In both cases, surgery was performed - extraction of the proximal endoprosthesis stem from the canal, removal of bone cement residues, reinstallation of the stem with cement fixation. In the postoperative period, standard management with wound healing by primary intention. Observation periods are 11 and 23 months, knee joint function is restored by 80%. Tumor recurrence was detected in 1 patient (4.7%) with osteosarcoma in the soft tissues of the thigh 18 months after surgery. Excision of the recurrent tumor was performed, which did not affect the functional outcome. The functional results of treatment were assessed using the generally accepted international MSTS (Musculo Skeletal Tumor Society Score) system. After resection of the distal femur, all patients showed excellent and good functional results. knee joint function recovery according to the MSTS scale was 80-90%;. After resection of the proximal tibia, all patients showed good results, knee joint function recovery according to the MSTS scale was 75-80%.
4. Conclusions
- More than half of primary malignant tumors of the skeleton occur in the bones that form the knee joint. Therefore, the improvement of existing and the development of new methods for reconstructing this joint in tumors of the proximal tibia and distal femur are one of the main innovative areas in modern oncology. Implants of foreign manufacturers are not widely available due to their high cost. The development, introduction into production and use of endoprostheses of our own designs will solve both medical and economic problems in the treatment of patients. Thus, the widespread introduction into practice of a new endoprosthesis of our own design will improve the results of organ-preserving operations with the replacement of defects in the bones that form the knee joint.
5. Clinical Example
- Patient Sh., born in 1994. Diagnosis: Osteosarcoma of the distal metadiaphysis of the right femur G 2, T2N0M0, stage HB. The diagnosis was made in April 2015. After 5 courses of neoadjuvant chemotherapy according to the AR regimen, a good clinical effect was achieved (partial tumor regression). On 08.01.2016, an operation was performed - resection of the distal part of the right femur with replacement of the defect with a knee joint endoprosthesis of our own design. There were no intraoperative and postoperative complications. On the 2nd day, the patient began to move with crutches. Postoperative histological conclusion - osteosarcoma. Grade III therapeutic pathomorphosis. Taking into account the histological conclusion, the patient underwent 4 courses of adjuvant chemotherapy according to the same regimen. After 1 month, the knee joint function was restored by 40%, after 9 months by 90%.
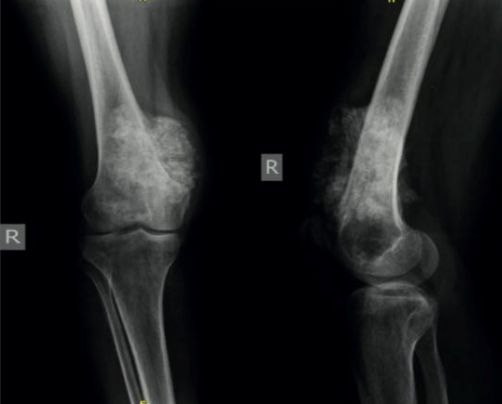 | Figure 4. Radiographs. Osteosarcoma of the distal metaphyseal part of the right femur |
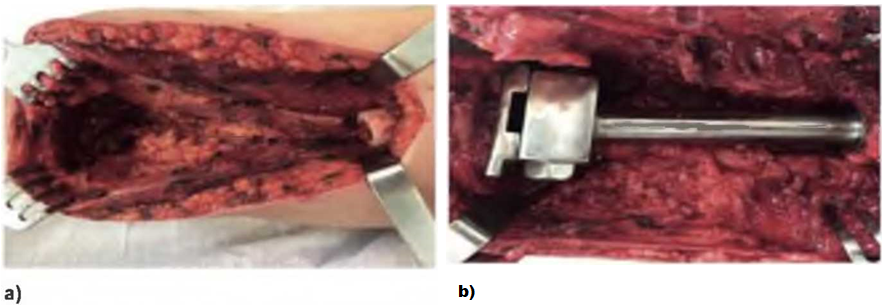 | Figure 5. Photo: a) the resulting defect after resection; 6) an endoprosthesis is installed |
 | Figure 6. Photo. Removed macropreparation |
 | Figure 7. Radiographs. Condition after resection of the distal femur and proximal articular surface of the tibia with knee arthroplasty: a) early postoperative period; b) 5 years later |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML