-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3210-3212
doi:10.5923/j.ajmms.20241412.25
Received: Nov. 16, 2024; Accepted: Dec. 6, 2024; Published: Dec. 16, 2024

Surgical Treatment Efficacy Juvenile Glaucoma with Myopia
Nabiev Abduvali Mirzaievich1, Sodikov Sherzod Adbugofurovich2, Boltaeva Sanobar Atamuradovna3, Faizieva Sevara Batirovna4
1Doctor of Medical Sciences, Chief Physician, Tashkent Regional Branch of Republican Specialized Scientific and Practical Medical Center of Eye Microsurgery of Uzbekistan, Tashkent, Uzbekistan
2Resident Physician, Republican Clinical Ophthalmological Hospital, Tashkent, Uzbekistan
3Head of Eye Microsurgery Department, Tashkent Regional Branch of Republican Specialized Scientific and Practical Medical Center of Eye Microsurgery of Uzbekistan, Tashkent, Uzbekistan
4Resident Physician of Tashkent Regional Branch of Republican Specialized Scientific and Practical Medical Center of Eye Microsurgery of Uzbekistan, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A comparative analysis of the results of surgical treatment of 41 patients (76 eyes) with open-angle juvenile glaucoma against the background of myopia of various degrees - the main group - was carried out. The control group consisted of data from 16 patients (21 eyes) who received conservative treatment. 14 surgeries were performed on 76 eyes, 20 trabeculotomy, 16 trabeculotomy with drainage, and 13 trabeculotomy with iridectomy. In 42 eyes (revision surgeries), 5-fluorouracil was used. In the long-term period, IOP was compensated in 89% of cases. It has been established that the advantage of fistulizing surgical treatment of this group of patients over non-penetrating ones, especially in the advanced and advanced stages with the use of 5-fluorouracil, as well as the use of drainage surgery, is promising.
Keywords: Juvenile glaucoma, Myopia, Surgical treatment
Cite this paper: Nabiev Abduvali Mirzaievich, Sodikov Sherzod Adbugofurovich, Boltaeva Sanobar Atamuradovna, Faizieva Sevara Batirovna, Surgical Treatment Efficacy Juvenile Glaucoma with Myopia, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3210-3212. doi: 10.5923/j.ajmms.20241412.25.
1. Introduction
- One of the unsolved problems is early diagnosis of juvenile glaucoma against the background of progressive myopia regardless of its degree and in case of establishing combined pathology in search of new ways to preserve visual functions in patients [6]. Among glaucoma patients of young age (up to 40 years old), myopic refraction occurs from 51.4% to 57.3% of cases. At the same time, in elderly glaucoma patients, myopic refraction is observed in only 7.4% [5]. As a cause of disability due to ophthalmopathology, glaucoma accounts for 28%, myopia - 19% [2,4].It has been established that visual function decline in patients with progressive myopia is more often caused not by myopia, but by unrecognised glaucomatous process; that patients are more often blinded not because of myopia, but because of glaucoma [1,7].Currently available literature data indicate that there is no unified view on the indications for surgical neuroprotective treatment of juvenile glaucoma in myopia. Meanwhile, the contradictions on the key issues concerning the diagnosis and treatment of juvenile glaucoma with progressive myopia indicate that the problem is insufficiently studied and require further research [3,8]. Objective: to analyse the clinical and functional features and results of surgical treatment of juvenile open-angle glaucoma (JOGOAG) against the background of various degrees of myopia.
2. Material and Methods
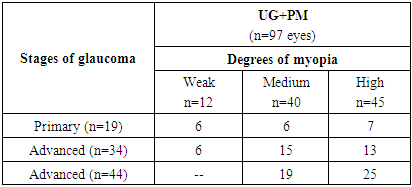
- A comparative analysis of the results of surgical treatment of 41 patients (76 eyes) with open-angle form of juvenile glaucoma on the background of myopia of different degrees - the main group - was carried out. The control group consisted of data of 16 patients (21 eyes) receiving conservative treatment. The age of patients was from 15 to 37 years, mean age 28,2±5,4. Among them, there were 27 males and 31 females. The follow-up period ranged from 6 months to 3 years. The initial stage of UG was established in 19 eyes (19,6%), developed stage - in 34 eyes (35,1%), far advanced stage - in 44 eyes (45,3%), there were no patients with absolute stage. Combination of the initial stage of UG with myopia of weak degree in 6 eyes, with medium degree in 6 eyes and with far advanced stage in 7 eyes. At the advanced stage of UG, myopia of a weak degree was established in 6 eyes, with a medium degree in 15 eyes, and with a high degree in 13 eyes. On the background of far advanced UG, myopia of weak degree was not established, 19 eyes had myopia of medium degree, 25 eyes had myopia of high degree. The distribution of patients by myopia degree and stage of juvenile glaucoma is shown in Table 1.
|
3. Results
- In the initial stage of SE (19 eyes) visual acuity was 0.72±0.11 with correction with spherical lenses, horizontal corneal diameter was 11.1±0.3 mm, anterior chamber depth along the optical line was 3.0±0.3 mm. The mean IOP was 20.8±1.4 mm Hg. On the ocular fundus in all patients the ratio of the excavation diameter to the optic disc - E/D ratio was equal to 0.4. The borders of the visual fields along all meridians were at the level of norm and totalled 489.8±10.3°. At ultrasound examination on the optical axis, the anteroposterior size of the eyeball averaged 22.41±0.54 mm. In connection with stable indices of IOP level with compensation, local hypotensive conservative treatment was continued in 8 eyes. This group of patients underwent neuroprotective treatment. In 11 eyes IOP was over 27.0 mm Hg, they underwent surgery - non-penetrating deep sclerectomy. IOP in 10 days was at the level of 16.0 mm Hg, in the remote period normal IOP was observed in 8 eyes (72.7% of cases), 2 eyes were stabilised by nidling, one more eye underwent trabeculotomy with drainage.In the advanced stage of SE, 17 patients (42.5%) had complaints of lacrimation during near visual work and rapid fatigue. Visual acuity was 0.48±0.16 with correction with spherical and astigmatic lenses, horizontal corneal diameter was 12.1±0.2 mm, anterior chamber depth along the optical line was 3.2±0.5 mm. The average IOP was 24.7±0.5 mm Hg. On the ocular fundus in all patients the ratio of the excavation diameter to the optic disc - E/D ratio was 0.5-0.6. The borders of the visual fields along all meridians were at the level of norm and totalled 351.7±16.8°. At ultrasound examination the anteroposterior axis size of the eyeball averaged 24.6±0.5 mm. Local hypotensive conservative treatment was continued in 7 eyes due to stable IOP level with compensation. Neuroprotector mexidol 300 mg w/v, emoxipin parabulbarly for 2 weeks was administered to this group of patients against the background of standard trophic treatment. On 23 eyes goniodysgenesis of 2 degree was established and IOP was from 26,0 mm Hg to 34,0 mm Hg (average 27,3±3,1 mm Hg), they were operated - non-penetrating deep sclerectomy on 3 eyes, penetrating - on 20 eyes, 11 of them - repeatedly. Moreover, trabeculotomy in 10 eyes with 5-fluorouracil and sinus trabeculotomy with iridotomy with hydrogel drainage in 13 eyes. IOP after 10 days was at the level of 16.0-17.0 mmHg, in the remote period normal IOP was observed in 24 eyes (88.9% of cases), nidling was performed in 2 eyes, and penetrating reoperation was performed in two more eyes after NSCE.In the far advanced stage of UG, 17 patients (42.5%) had complaints of lacrimation at near vision and rapid fatigue. Visual acuity was 0.22±0.16 with correction with spherical and astigmatic lenses, horizontal corneal diameter was 13.9±0.2 mm, anterior chamber depth along the optical line was 3.7±1.1 mm. The average IOP was 29.3±4.5 mm Hg. In 9 eyes, due to the presence of keratoconus and corneal opacity in the optical zone, it was not possible to reliably determine the parameters of excavation of the RPE. In 38 eyes the ratio of the excavation diameter to the optic disc - E/D ratio was equal to 0.8-1.0. The borders of the visual fields along all meridians were at the level of norm and totalled 161.7±35.8°. At ultrasound examination the anteroposterior axis size of the eyeball averaged 28.6±2.3 mm.Local hypotensive conservative treatment was continued in 6 eyes due to stable IOP level with compensation. This group of patients was prescribed neuroprotectors - mexidol, cerebrolysin by injection, emoxipin locally parabulbarically for 2 weeks, after completion of injection therapy patients received mexidol 150 mg 3 times a day for 2 months. Goniodysgenesis of the 2nd degree was found in 25 eyes and goniodysgenesis of the 3rd degree in 19 eyes. IOP was at the level from 26.0 mm Hg to 34.0 mm Hg (average 27.3±3.1 mm Hg). This group of patients (38 eyes) underwent the following surgeries: - trabeculectomy 10 operations, trabeculectomy and iridectomy with 5-fluorouracil - 13 operations, trabeculectomy with hydrogel drainage - 16 operations. The surgeries were without complications in 37 eyes. One operation was accompanied with hyphema formation, which resolved on its own on the 3rd day after surgery. IOP in 10 days was at the level of 16.0-18.0 mm Hg, in the remote period normal IOP was observed in 29 eyes (87.9% of cases), nidling was performed in 5 eyes, reoperation with drainage was performed in one eye after trabeculotomy.
4. Discussion
- Thus, clinical manifestations of juvenile glaucoma on the background of myopia of various degrees are accompanied by an increase in biometric parameters of the eyes, caused by an increase in intraocular pressure and stretching of the fibrous capsule of the eye. Our observations have shown that in the overwhelming majority the timely diagnostics of juvenile glaucoma on the background of myopia of various degrees suffers. This is especially true for patients with medium and high degree myopia. When patients of this category apply to doctors, visual acuity is most often checked and the doctor is limited only to the selection of spectacle correction. As a result, among the operated patients (the main group) the initial stage of juvenile glaucoma was 15.5%, developed - 40%, far advanced - 44.6% of cases. Our data agree with the literature data [3,4,8]. Besides, in 56.5% (42 eyes) of cases the repeated surgical interventions show insufficient hypotensive efficiency of the previously performed surgeries in UG on the background of myopia of various degrees. In connection with the above-mentioned, we used fistulising surgeries in advanced and far advanced stages of UG on the background of myopia. Our views on the use of drainage surgery and its perspectives in the treatment of juvenile glaucoma on the background of myopia coincide with the opinion of other authors [2,6].
5. Conclusions
- 1. Conservative treatment of juvenile glaucoma with different degrees of myopia requires a more careful selection of hypotensive drugs and dynamic observation of visual functions.2. Non-penetrating surgeries are the method of choice in the initial stage of juvenile glaucoma due to insufficient efficiency (72.7%). The advantage of fistulising surgical treatment with hypotensive efficiency up to 88,9% of cases in this group of patients in advanced and far advanced stages of the disease is established. 3. The use of drainage surgery in repeated surgical interventions of juvenile glaucoma on the background of myopia of various degrees is promising and requires further research.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML