-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3207-3209
doi:10.5923/j.ajmms.20241412.24
Received: Nov. 25, 2024; Accepted: Dec. 10, 2024; Published: Dec. 16, 2024

Some Indicators of Reproductive Health in Diferent Forms of Polycystic Ovary Syndrome
Gulammaxmudova Dilobar Valijonovna
Doctor of Philosophy in Medical Sciences, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Gulammaxmudova Dilobar Valijonovna, Doctor of Philosophy in Medical Sciences, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

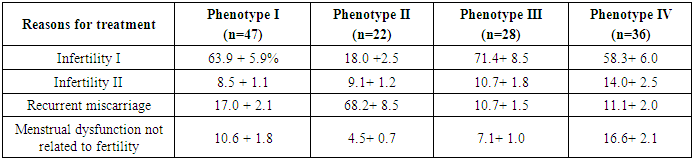
The article presents data on the study of reproductive disorders in women with PCOS, depending on the phenotype of the disease. Anamnesis was studied, clinical and hormonal studies were conducted in 133 patients with PCOS. The frequency of reproductive disorders and pregnancy outcomes were determined depending on the clinical form of the disease.
Keywords: Polycystic ovary syndrome, Reproductive function, Phenotype, Reproductive disorders, Hormonal studies, Pregnancy, Pregnancy outcomes
Cite this paper: Gulammaxmudova Dilobar Valijonovna, Some Indicators of Reproductive Health in Diferent Forms of Polycystic Ovary Syndrome, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3207-3209. doi: 10.5923/j.ajmms.20241412.24.
1. Introduction
- One of the most common causes of reproductive and health disorders in women of fertile age is polycystic ovary syndrome (PCOS). Clinical practice dictates the need to provide assistance to patients suffering from PCOS, and help them in solving problems, the main of which, obviously, is infertility. In addition, menstrual irregularities, metabolic disturbances, and cosmetic problems associated with excess androgen production are symptoms that are present in various combinations in all patients with PCOS and require treatment [1]. PCOS in the light of modern research refers to diseases of a polyetiological nature, the pathogenesis of the disease remains not fully understood. Accordingly, therapeutic approaches depend on the underlying problem with which the patient seeks a doctor. For obstetricians and gynecologists, the most frequent problems of this contingent of patients are primary or secondary infertility, fetal loss syndrome, and a number of pregnancy complications [2]. In the general population of women of reproductive age, depending on the diagnostic criteria used, the prevalence of PCOS ranges from 5 to 12%, while in the structure of infertile marriage, PCOS is 35-50%. Despite the high incidence of this disease and many years of clinical practice, the treatment of reproductive disorders in women with PCOS remains in the focus of attention of gynecologists and reproductologists. The variety of clinical manifestations of the disease requires differentiation from specialists in the choice of therapeutic tactics [3]. The objective of the research: To analyze reproductive disorders in women with PCOS depending on the phenotype of the disease.
2. Materials and Methods
- We examined 133 patients aged 19-35 years with PCOS. The diagnosis and phenotypes of the disease were verified on the basis of the recommendations of the Rotterdam Consensus (2003). We have developed special questionnaires that include reasons for going to a medical institution, anamnesis data, reflecting diseases of the reproductive system, features of the course of pregnancy and childbirth, the presence of gynecological diseases. To clarify the diagnosis and exclude conditions similar to PCOS, hormonal studies were carried out with standard kits by the ELISA method. The data obtained were subjected to statistical processing using standard computer programs with the calculation of the arithmetic mean (M), standard deviation (σ), mean error of the arithmetic mean (± m).
3. Results and Discussion
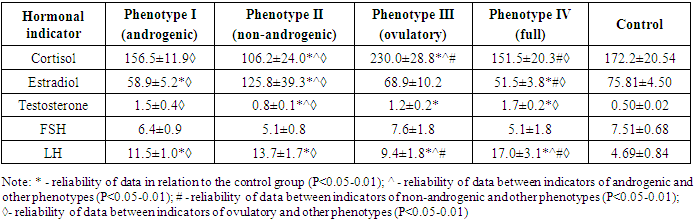
- Currently, most researchers have accepted the diagnostic criteria proposed by the 2003 Rotterdam Consensus, the European Society for Fertility and Embryology, and the American Society for Reproductive Medicine. According to the consensus, the diagnosis of PCOS is eligible after excluding other similar conditions, if any two of the following three criteria are present: anovulation or oligo-ovulation, clinical and / or laboratory signs of hyperandrogenism, polycystic ovary according to ultrasound. At the same time, depending on the combination of symptoms, 4 phenotypes of the disease are distinguished. These phenotypes combine a fairly wide range of clinical manifestations of the disease. There are differences in clinical and laboratory parameters, some hormonal characteristics of each phenotype are demonstrated in Table 1.
|
|
4. Conclusions
- Thus, polycystic ovary syndrome is a disease with a high incidence of reproductive disorders and complications of pregnancy. Detected disorders is different in phenotypes of PCOS, which should be taken into account in the treatment and preconception counseling.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML