Kholzhigitova Mukhayyo Berdikulovna1, Ubaydullaeva Naima Nabixanovna2
1PhD., Associate Professor of the Department of Internal Medicine No. 4 Samarkand State Medical University, Samarkand, Uzbekistan
2DSc, Associate Professor, Department of Pulmonology with a Course in Clinical Allergology, Center for the Development of Professional Qualifications of Medical Workers, Samarkand, Uzbekistan
Correspondence to: Kholzhigitova Mukhayyo Berdikulovna, PhD., Associate Professor of the Department of Internal Medicine No. 4 Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
A new effective approach to early diagnosis and treatment of chronic obstructive pulmonary disease(COPD) has been developed based on the clinical, immunological and antioxidant characteristics of the disease. The study included 66 patients with chronic obstructive pulmonary disease who were treated in the allergology and pulmonology departments of the Samarkand City Medical Association in 2021-2023. Changes in the cellular immunity, humoral immunity profile in blood serum and bronchoalveolar lavage infections, the effects of immunomodulators on the disease clinic and the dynamics of immunological shifts after immunocorrection depending on gender in chronic obstructive pulmonary disease are described in detail.
Keywords:
Chronic obstructive pulmonary disease, Inflammatory markers, Cellular immunity, Humoral immunity, Immunotherapy, Antioxidant therapy
Cite this paper: Kholzhigitova Mukhayyo Berdikulovna, Ubaydullaeva Naima Nabixanovna, Relationship Between Immune and Infectious Markers of Inflammation in Patients with Chronic Obstructive Pulmonary Disease and Assessment of the Effectiveness of Immunocorregive and Antioxidant Therapy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3194-3199. doi: 10.5923/j.ajmms.20241412.22.
1. Introduction
Respiratory diseases occupy a leading place in the pathology of the respiratory system, characterized by a significant prevalence and a tendency to a recurrent course [1,3,10,17]. The problem of chronic obstructive pulmonary disease (COPD) is extremely relevant in modern medicine due to the widespread, impaired vital functions of the lungs and heart, leading to permanent disability and death [9,10]. In terms of the frequency of deaths, COPD ranks 4th in the world in the age group over 45 years and this figure is growing. According to GOLD forecasts [8,15], by 2020 COPD will take the third place as a cause of death. The economic and social damage from this disease is enormous and therefore COPD is currently considered as a “social burden” [9,13,19]. COPD is one of the most common human diseases, which is primarily due to the high prevalence of smoking, environmental pollution and recurrent respiratory infections [7,11,18]. This disease is one of the most important causes of morbidity and mortality worldwide [2,4,12,16]. COPD is a serious health problem due to the prevalence of the disease, reduced life expectancy, significant economic damage associated with temporary and permanent disability of the most active part of the population [3,8,14]. Establishing disorders in systemic immunity in COPD is the goal of many studies, since expanding understanding of the pathogenesis of the disease can contribute to the development of new educational and preventive measures in COPD [8,14,20].In Russia, According to scientific research, more than 25% of patient requests Respiratory diseases are treated by a doctor. In recent years, the incidence of Chronic lung pathology is growing all over the world, including in Uzbekistan, which is characterized by their increase in relation to common diseases by 21%. Currently, many risk factors are known that contribute to the development of COPD, but the most common among them are smoking and infectious factors, which accompany 50-60% of cases. Therefore, determining the etiology of COPD, predicting its course and finding new treatment methods is an important task of clinical pulmonology.A number of scientific studies are conducted worldwide to achieve high efficiency in improving early diagnostics, treatment and prevention of COPD. At the same time, one of the important tasks in COPD is to determine the role of atypical infection, infectious inflammatory factors, the mutual influence of immunoglobulin of the immune system, the influence of the antioxidant defense system on the development of inflammation and its exacerbation in the pathogenesis of the disease. On the other hand, an important factor is considered to be changes in the functional state of immunoglobulins and lymphocytes involved in the cytokine mechanisms of the immune system and the lack of analysis of the effectiveness of immunocorrective therapy, for which it is advisable to recommend immunocorrective drugs. In chronic obstructive pulmonary disease, a relative decrease in CD3, CD4, CD8 cells and lymphocytes and a two-fold increase in these indicators after immunocorrection were observed, as well as a change in the production of inflammatory and non-inflammatory cytokines that determine the course of the disease, showing the important role of immune mechanisms in the developing incompatibility of the immune system.
2. The Aim of the Study
to develop a new effective approach for early diagnosis and treatment of COPD based on the clinical, immunological and antioxidant characteristics of the disease.
3. Object and Result of the Study
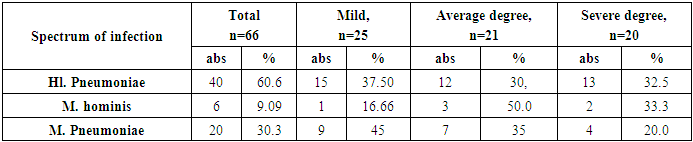
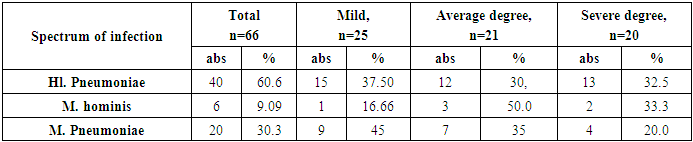
The study included 66 patients with COPD who were treated in the allergology and pulmonology departments of the Samarkand City Medical Association in 2021-2023.A special questionnaire for the detection of COPD was used (developed by the fundamental laboratory of the Institute of Immunology and Human Genomics of the Academy of Sciences of the Republic of Uzbekistan). The purpose of the survey was to monitor patients with COPD among patients with respiratory diseases, as well as to conduct in-depth diagnostics and treatment. Under observation were 66 patients with a diagnosis of COPD (ICD-10), aged 35-73 years (mean age 54.75±1.15 years), the average duration of the disease was 9.5±0.45 years. There were 41 men (59.85%) and 25 women (40.14%). The control group consisted of 21 conditionally healthy volunteers without signs of respiratory pathology with the corresponding anthropometric characteristics. Of these, 11 (52.38%) were men and 10 (47.61%) were women, whose average age was 47.5 ±1.5 years. To assess the course of clinical signs of COPD depending on age, the examined patients were divided into the following age groups: 16 (24.24%) aged 35-45 years, 29 (43.93%) aged 46-60 years and 21 (31, 81%) aged 61-73 years. The diagnosis of the examined patients was established on the basis of the ICD10 classification. The patients were divided into groups according to the severity of the disease: mild COPD-1, moderate COPD-2, severe COPD-3 - 25 (46.32%), - 21 (30.88%), - 20 (22.79%) respectively. For immunocorrection, the patients were divided into 2 small groups: a) a group of 20 patients who received quercetin + traditional therapy, b) a group of 23 patients who received bronchomunal + traditional therapy, the 2nd group received only traditional therapy formed the control group.General clinical examinations of all patients included: objective examinations, general blood, urine and sputum analysis; measurement of external respiratory function (ERF) by spirography on the SPIROSIFT-5000 device. Initial studies included an inhalation bronchodilator pharmacological test using b-agonists to study the frequency of broncho-obstruction recurrences; chest X-ray, fluoroscopy, bronchoscopy; determination of interleukins and the spectrum of atypical infection in the blood serum and bronchoalveolar fluid using enzyme immunoassay and polymerase chain reaction methods, as well as an assessment of the activity of the antioxidant system (catalase and peroxidase) by the photometric method. A sufficient volume of study materials allowed us to conduct a representative analysis from the point of view of different approaches.The following methods were used to assess the state of the immune system: 1. isolation of lymphocytes from peripheral blood using the Ficoll-verografin gradient (Boyum, 1968); 2. detection of the subpopulation composition of lymphocytes using monoclonal antibodies CD3, CD4, CD8, CD16, CD23 and CD25 (OOO Sorbent Product, Russian Federation, Moscow); 3. determination of the concentration of immunoglobulins A, M, G using the standard Mancini radical immunodiffusion method; 4. To carry out immune correction, patients were divided into 2 small groups: a) a group of 20 patients who received quercetin + traditional therapy, b) a group of 23 patients who received bronchomunal + traditional therapy, the 2nd group that received only traditional therapy constituted the control group. 20 patients were prescribed quercetin 1 packet 2 times a day for 10 days and on the 11th-13th day the immune system parameters were re-examined. 23 patients were prescribed bronchomunal 1 capsule (7 mg) for 10 days every 3 months. After 3 months a repeat examination was conducted and the function of external respiration was determined. The studies showed that 48.52% of patients had atypical infections in their bronchoalveolar lavage, namely Chlamidiya (Chl) pneumoniae in 60.0% (10 6 / ml), Mikoplazma (M) hominis in 7.57% (102 /ml), and Mikoplazma (M) pneumoniae in 31.81% (104 /ml). Patients infected with atypical infections were divided into groups based on the severity of the disease. In this case, 40 patients (60.0%) had Hl. Pneumoniae (26 (65%) men, 14 (35%) women), and 20 patients (31.8%) had M. Pneumoniae (14 (70%) men, 6 (30%) women). We believe that the incidence of atypical infections in men is higher than in women. In our opinion, this is due to lifestyle, working conditions, and stress. According to our data, both infections detected are more common in men.Patients with atypical infection were divided into groups depending on the severity of the disease. A high role of Chl. Pneumoniae (60.6%) was determined in the development of the disease, depending on the severity of the disease, the patients were distributed as follows: 15 (37.5%) patients with Chl. Pneumoniae had a mild degree, 12 (30.0%) had a moderate degree, and 13 (32.5%) had a severe degree of the disease. The total number of patients with M. Pneumoniae was 20 (30.3%), with a mild degree of 9 (45%), moderate severity of 7 (35%), and severe degree of only 4 (20.0%). M. hominis was observed in 6 (9.09%) patients, with a mild degree of the disease occurring in 1 (16.66%) patient, moderate severity in 3 (50.0%) and severe severity in 2 (33.3%) patients (see Table 1).Table 1. Distribution of patients with atypical infection depending on the severity of the disease
 |
| |
|
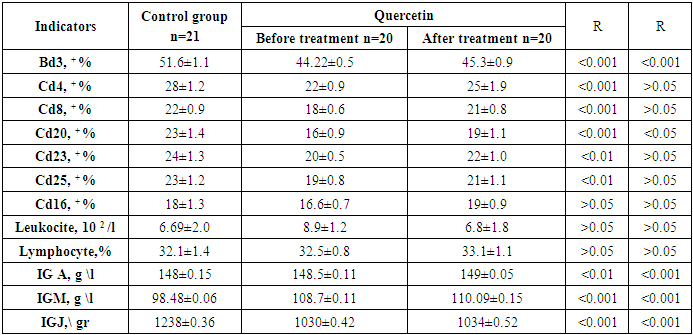
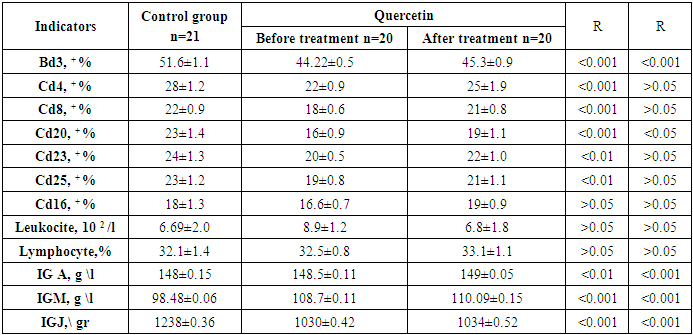
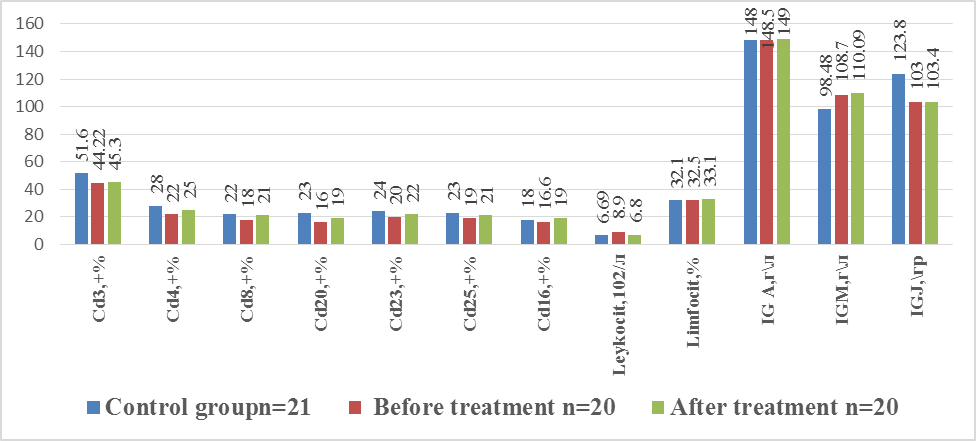
The effectiveness of immunocorrection was studied based on the dynamics of immunological parameters, severity of clinical and laboratory index and duration of remission. First, changes in immune system parameters were assessed depending on the spectrum of infection. In total, the types of the spectrum of atypical bronchoalveolar fluid infection were studied in 66 patients. Thus, Chl. Pneumonia gave a positive result in (n=40) patients. M. Pneumonia gave a positive result in (n=21) patients. M. hominus was positive in 6 patients and the immune system parameters in these patients were not studied due to the small number of patients.The following parameters were determined in the lymphocyte subpopulation: Cd3, + %- in the control (n=21), 51.6±1.1, Chl. Pneumonia, (n=40), 45.22±0.5, M Pneumonia (n=21)-47.3±0.9, p< 0.0 5, Cd4, + %- 28±1.2 in the control, Chl. Pneumonia24±0.9, M Pneumonia 26±1.9, p< 0.01, Cd8, + %- 22±0.9 in the control, Chl. Pneumonia 20±0.6, M Pneumonia-22±0.8, p< 0.05, Cd20, + %- 23±1.4 in the control, Chl. Pneumonia 17±0.9, M Pneumonia-19±1.1, p< 0.02, Cd16 + %- 18±1.3 in the control, Chl. Pneumonia 16.6±0.7, M Pneumonia -19±0.9, p< 0.0 2. Thus, low lymphocyte counts were observed in the main groups. A decrease in the relative number of lymphocytes was observed. Changes in the number of leukocytes were 6.69±2.0 in the control group, 12±1.8 in COPD caused by Chl. Pneumonia, 8.78±1.2 in COPD caused by M Pneumonia (p< 0.05), these indicators indicate a higher activity of the inflammatory process caused by Chl. Pneumonia. Humoral immunity indices showed changes for both pathogens: an increase in IgM was detected for Chl. Pneumonia up to 107.7±0.11 with an index of 98.48±0.06 in people of the control group, for M Pneumonia the indices were -109.09±0.15 (p< 0.05). These indices indicate higher indices of the inflammatory process in bronchitis caused by M Pneumonia.Despite the above, the IgA deficiency persists: in the control 148±0.15, Chl. Pneumonia 146.5±0.11, M Pneumonia - 148±0.05 (p <0.01) kuzatildi. The immune system parameters in patients with Chl. Pneumonia were significantly lower than in patients with M Pneumonia, indicating a more severe course of the inflammatory process.The clear distinction between cellular and immune changes with specific activity served to study the subpopulation composition of lymphoid cells before and after treatment.The immune system indices in patients with Chl. Pneumonia were significantly lower than in patients with M. Pneumonia. There was a relative decrease in the number of CD3 +, CD8 +, CD16 + lymphocytes (p < 0.05), and no significant changes in CD4 + indices were observed.Prescription of combination therapy of immunomodulators in combination with standard treatment for chronic obstructive bronchitis leads to improvement of immune status indices and increase in therapy effectiveness. In the first subgroup, quercetin + traditional therapy were used (n=20).In the first subgroup, the number of leukocytes in the blood before treatment was 8.9 ± 1.2, and after treatment there was a decrease to 6.8 ± 1.8 (p < 0.02). Analysis of the indicators of the T-lymphocyte marker CD3 + was lower in patients with COB, when compared with the control group (51.6 ± 1.1 μl ) and they were 44.22 ± 0.5 before treatment and 45.3 ± 0.9 after treatment (r< 0.05). Similar changes in the parameters were also noted in the case of CD4 + %, which was normally 28 ± 1.2, before treatment 22 ± 0.9 and after treatment 25 ± 1.9 (p< 0.05), CD8 + was normally 22 ± 0.9, before treatment 18 ± 0.6, after treatment 21 ± 0.8 (r< 0.05) and CD16 +% was normally 18 ± 1.3, before treatment 16.6 ± 0.7 and after treatment 19 ± 0.9 (r < 0.05). No significant changes were observed in the remaining subpopulations.During the immune response, B-lymphocytes differentiate into plasma cells and secretory antibodies. In our studies, humoral immunity indices were assessed by the values of IgA, IgM, Ig G in the blood. Based on the studies conducted in this regard, we found that the level of immunoglobulins before and after treatment in the first subgroup changed statistically insignificantly and amounted to IgA before treatment 148.5 ± 0.11, after treatment 149 ± 0.05 g/l, and in the control group 148 ± 0.15. IgM - 108.7 ± 0.11 and 110.09 ± 0.15 g / l, respectively, and in the control group 98.48 ± 0.06, IgJ - 1030.05 ± 0.42 and 1034.07 ± 0.52 g / l before and after treatment, respectively. IgM concentrations were almost the same as normal. During Ig A deficiency, IgM participates in the compensatory function as the formation of a defense line during inflammation (see table 2).Table 2. Immune system indicators after immunocorrection with quercetin
 |
| |
|
Thus, from a comprehensive assessment of the immune status during the formation of immunodeficiency in COPD, it became clear that chronic inflammation is characterized by a decrease in immunoregulation. This leads to a violation of the reproduction of immune component cells, inhibition of antigen production, and a decrease in its anti-inflammatory properties. An assessment of pharmacotherapy was carried out in subgroup 2, where Bronchomunal lyophilized bacterial lysate was prescribed according to the scheme in therapeutic doses, which increases the concentration of circulating T-lymphocytes in the blood, stimulates the function of macrophages, and increases the amount of immunoglobulins in the mucous membrane of the respiratory tract. The study of the state of cellular immunity in COPD was carried out by determining the number of CD3+, CD4+, CD8+ and CD16+%. It was revealed that the T-lymphocyte CD3+ indicators - 40.22 ± 0.5 μl in patients with COPD were 1.28 times lower than in the control group - 51.6 ± 1.1 μl, after the treatment this indicator increased by 1.17 times - 47.3 ± 0.9 μl (p< 0.05). An increase in the indices of other cell types in the T-lymphocyte population, in particular CD4+, CD8+ and CD16+, by an average of 1.33 times (r <0.05) was also noted. The level of leukocytes in the blood of patients in this group before treatment was 9.0±1.2, after pharmacotherapy it was 7±1.8, an effective reduction is evident (p<0.02) (see drawing 1).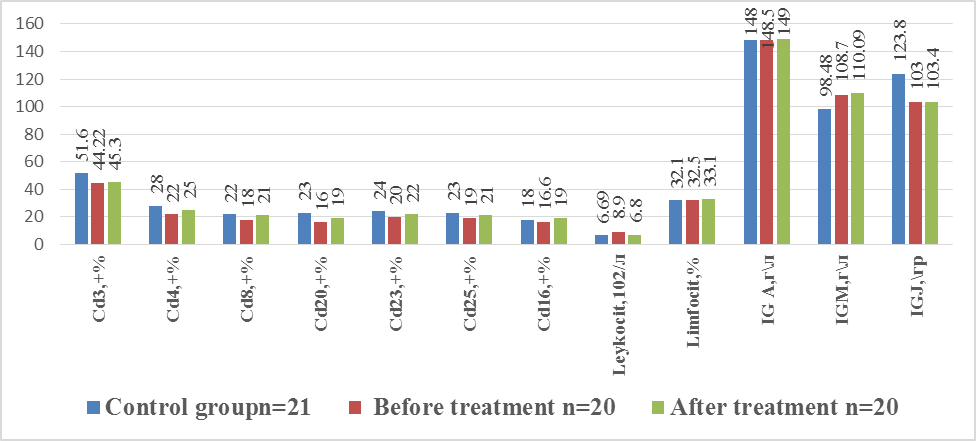 | Drawing 1. Immune system indicators after immunocorrection with bronchomunal |
Positive dynamics of changes in humoral immunity indices were noted in the second subgroup as follows: Ig A by 1.14 times, Ig M by 1.32 times, Ig G by 1.22 times (p<0.05). As noted above, this may be due to the fact that Ig M performs a compensatory function in case of Ig A deficiency and participates in the formation of a protective barrier during inflammation. In patients with a low Ig A index, deficiency of selective Ig A was detected in 13.3% of cases. The level of inflammatory activity did not change significantly after complex treatment without Bronchomunal. The results obtained after complex treatment with Bronchomunal showed that the drug has an effective immunomodulatory effect against inflammation. Also, in this group, elimination of broncho-obstructive syndrome was noted in 34.8% of cases. Normalization of these parameters, on the one hand, indicates a decrease in inflammatory activity during treatment, on the other hand, prevents complications and is a secondary prevention of the development of chronic obstructive pulmonary disease.A decrease in the secretion of sputum, cough and intoxication, a reduction in the symptoms of obstruction, as well as the normalization of humoral and cellular immunity are the criteria for the effectiveness of the therapy.Thus, a comprehensive assessment of the immune status in COPD revealed that chronic inflammation is characterized by a decrease in immunoregulation. This leads to a disruption in the reproduction of immune component cells, a decrease in antigen presentation, and a decrease in its anti-inflammatory properties.Normalization of these parameters, on the one hand, indicates a decrease in inflammatory activity during treatment, on the other hand, prevents complications and is a secondary prevention of the development of chronic obstructive pulmonary disease.As a result of the study “Relationship between immune and infectious markers of inflammation in patients with chronic obstructive pulmonary disease and assessment of the effectiveness of immunocorregive and antioxidant therapy”, the following conclusions were made:1. The diversity of clinical features of COPD depends on the immune reactivity of patients, the development of inflammation due to atypical infection, and the scope of inflammatory biomarkers of the immune system.2. In the bronchoalveolar fluid of patients with chronic bronchitis, atypical flora was detected in 48.52% of cases, including Chl. pneumoniae in 60.0% (microbial bodies 106 ml), M. hominis in 7.57% (microbial bodies 102 ml) and M. pneumoniae in 31.81% (microbial bodies 104 ml). These atypical microorganisms are the etiological factor that ensures the duration of inflammation and justifies the need for antibacterial therapy.3. The use of immunomodulatory and antioxidant therapy in patients with COPD contributed to the normalization of cellular and humoral immunity indicators, a decrease in neutrophilic inflammation, and significantly reduced the development of the fibrotic process, as a result of which an algorithm for the prevention of complications was developed.4. Restoration of the immune system was scientifically substantiated in patients with immunodeficiency 2.7-7±1.8 (p< 0.05), who, in addition to traditional therapy, were prescribed quercetin and bronchomunal for immunocorrection. It was found that the period of remission of the disease doubled.
References
| [1] | Albertson TE et al. Thelogical pharmacological management of asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS) // Expert Opinion on Pharmacotherapy. – 2020. – T. 21. – no. 2. – pp. 213-231. |
| [2] | Askarovna SO et al. Correlation of hormonal status indicators of physical and sexual development in children with chronic bronchitis //European science review. – 2017. – No. 1-2. |
| [3] | Dotan Y., So JY, Kim V. Chronic Bronchitis: Where Are We Now? // Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation. – 2019. – T. 6. – No. 2. – P. 178. |
| [4] | Mukhitdinovich SA, Atamuradovna ML Intrabronchial laser therapy in children with bronchoectatic disease and chronic bronchitis // Dostizheniya science i education. – 2017. – No. 9 (22). |
| [5] | Thimraj TA et al. Oxidative Signaling in Chronic Obstructive Airway Diseases // Immunity and inflammation in health and disease. – Academic Press, 2018. – P. 79 -98. |
| [6] | Vogelmeier CF et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary // American journal of respiratory and critical care medicine. – 2017. – T. 195. – No. 5. – pp. 557-582. |
| [7] | Dobritsa VP, Boterashvili NM, Dobritsa EV Modern immunomodulators for clinical use: A guide for doctors / VP Dobritsa. – St. Petersburg: Polytechnic, 2001. – 251 p. |
| [8] | Okboev TA Effects on the Course of Familial Bronchial Asthma Associated Allergic Diseases //Central Asian Journal of Medical and Natural Science. – 2023. – Vol. 4. – No. 5. – P. 721-725. |
| [9] | Sokolov DI, Kotov A.Yu., Simbirtsev AS, Freidlin IS Comparison of cytokines by their ability to influence the level of interleukin-8 secretion by endothelial cells. // Immunology. - 2000. – No. 1. – pp. 32-37. |
| [10] | Kholzhigitova M. B. et al. Characteristics of Clinical and Functional Indicators in Patients with Covid-19 Against the Background of Chronic Obstructive Pulmonary Disease // Journal of Science in Medicine and Life. - 2023. - V. 1. - No. 2. - P. 106-111. |
| [11] | Kholzhigitova M. B. et al. Clinical and bronchoscopic characteristics of the inflammatory process in patients with chronic obstructive bronchitis // Issues of Science and Education. - 2019. - No. 25 (74). - P. 55- 63. |
| [12] | Totolyan AA Freidlin IS Cells of the immune system / St. Petersburg: Nauka. - 2000. – 250 p. |
| [13] | Kholzhigitova MB, Aralov NR Studying the level of IL-8 production in bronchoalveolar lavage in patients with chronic obstructive bronchitis in adolescence. Academic Journal of Western Siberia 9 (1), 10-10. |
| [14] | Kholzhigitova MB, Aralov NR, Dusanov AD The level of local immunity factors in chronic obstructive bronchitis in adolescents. Tyumen Medical Journal 18 (1), 52-55. |
| [15] | Kholjigitova M. B., Ubaidullaeva N. N. General characteristics of patients with copd depending on the presence of metabolic syndrome in them // Oriental Journal of Medicine and Pharmacology. – 2022. – T. 2. – No. 06. – pp. 21-29. |
| [16] | Chuchalin AG Chronic obstructive bronchitis. //Ter. arch. – 2005. – No. 3. – pp. 5-9. |
| [17] | Chuchalin AG Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) Global strategy for diagnosis, treatment and prevention of chronic obstructive pulmonary disease. M.: "Atmosphere". 2007. 96 p. |
| [18] | Chuchalin AG The social burden of COPD. Materials of the symposium: epidemiology, diagnosis and treatment of chronic obstructive pulmonary disease – global trends and Russian features // Consilium medicum. (ec. issue). 2009. pp. 14-15. |
| [19] | Yashrolskaya Yu. A. 8th Congress of Pediatricians of Russia. - M., 2003. – P.436. (Khabarovsk Regional scientific and Practical Conference. “A teenager at the turn of the century.” Khabarovsk, 2011. – 200 p.) |
| [20] | Shmelev EI Pharmacotherapy of COPD: current data and new goals. // Materials of the symposium "Epidemiology, diagnosis and treatment of COPD – global trends and Russian features" // Consilium medicum (ec. issue). 2009. pp. 16-17. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML