-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3191-3193
doi:10.5923/j.ajmms.20241412.21
Received: Nov. 27, 2024; Accepted: Dec. 10, 2024; Published: Dec. 16, 2024

Assessment of the Cognitive State of Patients with Autonomic Disorders in Chronic Cerebral Ischemia
Mirzaeva Dilfuza Botirjonovna1, Abdurasulova Nozima Abduvokhid Kizi2
1PhD., Tashkent Medical Academy, Tashkent, Uzbekistan
2PhD Student, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Mirzaeva Dilfuza Botirjonovna, PhD., Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

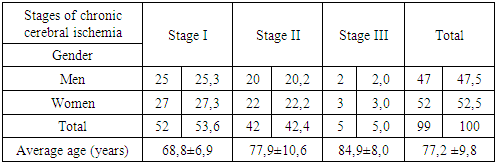
The syndrome of autonomic dysfunction is currently considered as a comorbid pathology of chronic cerebral ischemia (CCI), accompanying it as it develops. Changes occurring in the autonomic nervous system precede the subsequent neurological disorders and serve as a manifestation of maladaptive reactions. Background. The aim of our study was to conduct a neuropsychological study to identify cognitive impairment in patients with autonomic dysfunction at various stages of chronic cerebral ischemia. Methods. A study was conducted on 99 patients with autonomic dysfunction in CCI. There were examined cognitive violations at help special neuropsychological scales – MMSE, MoCA, HADS. The assessment of the vegetative status was performed using the Wayne questionnaire. Results. The results of our study revealed the absence of a direct proportional relationship between the patient's age and the stage of CCI, but there was a clear tendency towards an increase in the manifestations of CCI as the age of the patients increased. When studying the cognitive sphere with the MMSE scale, a direct correlation was noted between the worsening of cognitive impairment and the increase in the stage of chronic cerebral ischemia. The MoCA test showed memory impairment, difficulties in performing speed and attention tasks, as well as delayed recall in patients with stages II and III of chronic cerebral ischemia. Assessment of anxiety and depression using the HADS scale revealed an increase in anxiety-depressive manifestations with an increase in the severity of chronic cerebral ischemia (stage I – 8,0±1,5 points; stage II – 12,3±1,5 points and stage III – 14,2±1,7 points). Conclusions. In patients with autonomic dysfunction in chronic cerebral ischemia, cognitive impairment was observed. For definitions expressions cognitive dysfunctions follows apply special evaluation scales. Our studies revealed direct correlation changes in the severity of cognitive impairment with an increase in the stage of CCI.
Keywords: Chronic cerebral ischemia, Autonomic dysfunction syndrome, Cognitive impairment, Wein questionnaire, Special rating scales
Cite this paper: Mirzaeva Dilfuza Botirjonovna, Abdurasulova Nozima Abduvokhid Kizi, Assessment of the Cognitive State of Patients with Autonomic Disorders in Chronic Cerebral Ischemia, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3191-3193. doi: 10.5923/j.ajmms.20241412.21.
1. Introduction
- Chronic cerebral ischemia (CCI) is the most common cerebrovascular disease and is characterized by a negative impact on the quality of life of the population [2]. According to various studies, the epidemiological prevalence of CCI in the entire structure of cerebrovascular pathology is 60-75% [5].The syndrome of autonomic dysfunction in chronic cerebral ischemia manifests itself mainly by vegetative symptoms and emotional disorders [1,4]. The initial manifestations of CCI affect the emotional sphere to a greater extent, and are often manifested by astheno-depressive, asthenic and neurosis-like conditions [1].There is an increase in the number of patients with chronic cerebral circulatory insufficiency associated with cognitive impairment [2]. Cognitive impairment in CCI develops in more than 20% of cases [7]. At the same time, vascular cognitive impairment of both dementia and non-dementia forms of cognitive decline in the age category of patients over 65 years reaches a prevalence of 2,8% to 10% [3,7]. According to various authors, moderate and severe cognitive dysfunction occurs in 16,5% of cases in patients with CCI over 60 years of age[6]. Cognitive impairment in patients with CCI occurs as a result of brain damage caused by dysfunction of extra- and intracranial blood circulation during progressive ischemia. Mild cognitive impairment in cerebrovascular diseases is manifested by memory loss, impaired concentration and attention span, and the development of generalized asthenization. In addition, with CCI, sleep disorders are often observed, which manifest themselves already at an early stage of the disease and have a significant impact on the quality of life of patients [2,7].Currently, as a result of the high level of instability in the social sphere and the constant process of stress, there is an increase in the demands on the adaptive capabilities of a person. As a result of decompensation of adaptation mechanisms, the development of manifestations of various diseases occurs [1,2,4].Dysfunction of the autonomic nervous system in CCI develops as a result of pathological disturbances in the area of non-specific systems of the brain that regulate psycho-auto-somatic unity [2]. Most researchers associate selected neurophysiological characteristics with the peculiarities of psychological and constitutional-genetic status in patients with dysfunction of the autonomic nervous system [7].Clinical manifestations of autonomic dysfunction and their diagnostics are quite subjective, since they are based on the patient's own sensations. In this regard, the issues of diagnostics and objectification of autonomic dysfunctions in chronic cerebral ischemia are of particular relevance [4,5].To date, there are a number of studies devoted to the analysis of the vegetative status and cognitive sphere in CCI, but they are quite few in number, have different designs and often show divergent results. In addition, vegetative disorders in patients with CCI are usually studied without regard to age-related changes in the central nervous system. These circumstances served to determine the purpose and objectives of this study. The purpose of our study was to conduct a neuropsychological study to identify cognitive disorders in patients with autonomic dysfunctions at various stages of chronic cerebral ischemia.
2. Materials and Methods
- We conducted studies on 99 patients with chronic cerebral ischemia. All patients were hospitalized in the neurological department of the Tashkent Medical Academy. Our study included patients who signed a written informed consent to participate in the study. To analyze the state of the autonomic nervous system, the “Questionnaire for identifying signs of autonomic changes” by A.M. Vein (1998) was used. The Mini-Mental State Examination (MMSE) was used for screening assessment of the presence of cognitive impairment. The screening assessment was necessary because complaints of autonomic dysfunction and patients' responses to the "Questionnaire for the Identification of Signs of Autonomic Changes" by A.M. Vein, as well as to the scales for identifying emotional, anxiety and depressive disorders are purely subjective, and the results largely depend on the presence and severity of cognitive dysfunction. Therefore, patients with MMSE less than 20 points were not included in the study. The Montreal Cognitive Assessment Scale (MoCA test) was used for objectification and quantitative assessment of the identified disorders in the cognitive sphere. Emotional disorders in the form of irritability, tearfulness, emotional lability and sudden mood swings, as well as anxiety and depression always accompany autonomic dysfunction. The use of the Hospital Anxiety and Depression Scale (HADS) allows to identify the state of anxiety and depression in the patient. In statistical analysis, the data were evaluated using SPSS software for Windows (version 21.0).
3. Result and Discussion
- The analysis of the average age of patients treated in the neurological department of the TMA for chronic cerebral ischemia of stages I, II and III was carried out. Table 1 shows the distribution of patients depending on the stage of CCI.
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML