Rajabov V. B., Safoyev B. B., Yarikulov Sh. Sh.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Despite the fact that for more than 100 years, the problem of peritonitis has received the greatest attention from surgeons around the world, the mortality rate for diffuse purulent peritonitis remains virtually unchanged and ranges from 4.5% to 58% and higher. In severe forms of peritonitis, mortality may increase by more than 30-50%. The purpose of this study is to improve the results of treatment of patients with advanced peritonitis by using a multi-channel drainage tube. The scientific work is based on the analysis of the results of surgical treatment of 103 patients with diffuse peritonitis who were treated in the Bukhara department of the RNCEMP from 2018 to 2023.
Keywords:
Diffuse peritonitis, Laparotomy, Drainage, Postappendicular peritonitis, Gynecological peritonitis, Hemorrhagic peritonitis, Urinary peritonitis
Cite this paper: Rajabov V. B., Safoyev B. B., Yarikulov Sh. Sh., An Improved Method of Treating Patients with Diffuse Peritonitis by Using an Abdominal Sanitation Device, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3180-3184. doi: 10.5923/j.ajmms.20241412.19.
1. Introduction
According to V.S. Savelyev with co-authorship [1,3,6] about 15-20% of patients with acute surgical pathology of the abdominal cavity are admitted to surgical departments with signs of local or diffuse peritonitis. Most often, diffuse purulent peritonitis develops due to delayed treatment of patients with acute surgical diseases of the abdominal cavity. According to the available numerous data, among surgical pathology, perforation of the hollow organ most often leads to the development of peritonitis: stomach and duodenum about 30%, destructive appendicitis – more than 20%, lesions of the colon – 20-25%, small intestine – about 15% [3,4,6].In general, the available research results suggest that body-related factors affect the outcome of the disease more significantly than the type and source of infection [2,5,7]. Despite the fact that for more than 100 years the problem of peritonitis has received the greatest attention from surgeons around the world, the mortality rate for diffuse purulent peritonitis remains almost unchanged and ranges from 4.5% to 58% and above. In severe forms of peritonitis, mortality may increase by more than 30-50%. The parallel development of sepsis, septic shock, and multiple organ failure increases mortality to a level of 70% or more. Based on research, it was found that, regardless of the form of peritonitis, surgical intervention is the most effective method of its treatment.
2. Material and Methods
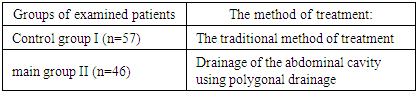
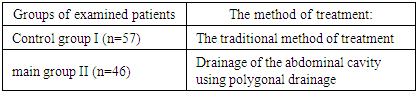
Analyzed data examination and treatment of 103 patients with diffuse peritonitis of various etiologies who were treated in the Department of emergency Surgery of the Bukhara City Medical Association and the Bukhara branch of the RNCEMP from 2018 to 2023.All patients, depending on the treatment method, were divided into 2 groups: the I – comparison group and the II – main group (Table 1). The I – control group consisted of 57 patients with diffuse peritonitis who received inpatient traditional treatment methods in the period 2018-2020.Table 1. Distribution of patients depending on the type of therapeutic measures
 |
| |
|
3. Results and Discussion
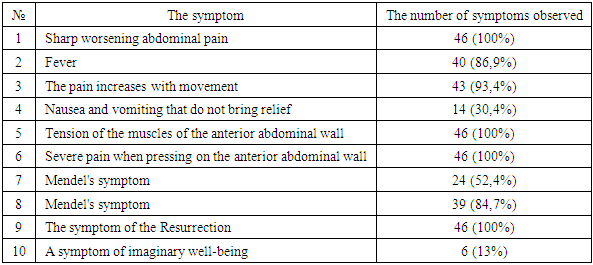
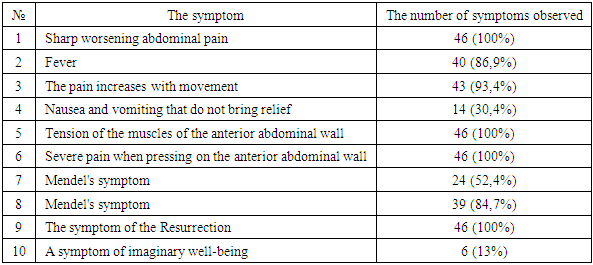
In patients of the comparison group I, after the elimination of the lesion and sanitation, the abdominal cavity was drained with a silicone drainage tube with a lumen size of 0.7-0.8 centimeters from three points with three drains. The first upper drainage tube, taking into account the area of localization of peritonitis, is installed in the right or left hypochondrium. The inner part of the drainage with 2-3 holes in the side walls was installed perpendicular between the internal organs and the anterior abdominal wall. The lower drainage from the left is installed at the entrance of the pelvis, on the right the end of the drainage tube is connected to the bottom of the pelvis.In the postoperative period, taking into account the antibiotic sensitivity of the identified microflora, 3-6 times a day were administered daily according to indications through the upper drainage tube. Before the detection of microflora sensitivity, Sulbactam 1.0 x 3 times a day, dissolved in 0.9% - 10 ml physical solution, was used as empirical antibiotic therapy. Since, according to our data, in our region, the pathogenic microflora in most cases shows sensitivity to this antibiotic (up to 70%).Unlike the control group, all patients of group II, when draining the abdominal cavity at the site of the upper single-light drainage, intraoperatively used a poly-channel silicone drainage tube with a channel lumen of 0.5 cm, with tank holes. The multi-channel drainage tube consists of 5 to 7 separate drainage passages with a clearance of 0.5 cm. The middle portion of the drains is combined, passing through the common passage of the silicone drainage is combined, the proximal end of the drainage passages is divided freely as a separate drainage tube.All patients with diffuse peritonitis of groups I and II compared the day of admission after short-term preoperative preparation within 1-2 hours, an emergency operation was performed that is aimed at clarifying and eliminating the source of peritonitis, sanitation, determining the prevalence of peritonitis in the abdominal cavity, a set of fluids for the affected areas for bacteriological studies, drainage of the abdominal cavity with three drains in group I patients with polycanal drainage in group II patients.The II group of the study included 46 patients with diffuse peritonitis, in which the complex treatment carried out in the control groups was characterized by the fact that a polychannel silicone drainage tube was used in the place of the upper single-light drainage, with a channel lumen of 0.5 centimeters, with tank holes. The multi-channel drainage tube consists of 5 to 7 separate drainage passages with a clearance of 0.5 centimeters. The middle portion of the drains is combined by passing through a common silicone drainage passage, the proximal end of the drainage passages is divided freely as a separate drainage tube. The number of drainage passages depends on the area of diffuse peritonitis. For example, if the process is common in three areas of the abdominal cavity, a five-channel drainage tube was used. Since, in this case, the first drainage tube is installed under the transverse colon, the second drainage tube is installed between the loops in the mesentery roots of the affected area, the remaining three drainage tubes are installed in three areas of the abdominal area which diffuse peritonitis is common, for example: right iliac, epitgastric and right lateral canal.In the postoperative period, to determine the exact localization of each drainage channel, the first drainage channel, which is installed under the transverse colon, the distal end was colored yellow, the second drainage channel, which is installed by the mesentery root, the affected part of the peritoneum, was marked in green. The remaining drainage channels, which are installed in the affected area of the abdominal cavity, were colored red. The amounts of red color simultaneously showed the cleavage of the abdominal cavity area involved in the process of peritonitis. The method of antibiotic therapy for the second group of patients was identical as the control group, but, unlike their antibiotics, the main group was administered through a different drainage channel separately from the above areas.If necessary, these patients also underwent ultrasound diagnostics of the abdominal cavity. Studies of the presence of symptoms of peritoneal irritation and other symptoms characteristic of peritonitis have revealed the following:Table 2. The frequency of detected symptoms of peritonitis in patients of group II (n=46)
 |
| |
|
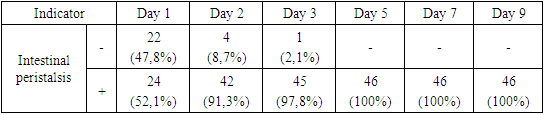
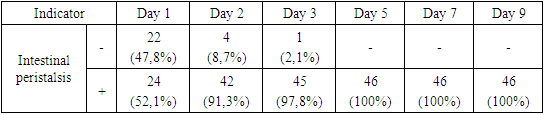
It should be noted, as mentioned above, in order to preserve the synchronicity of the various groups, patients with organ insufficiency were not included in the study.All patients of group II also underwent objective and laboratory examinations, if necessary, ultrasound and X-ray examinations, on the day of admission to establish a diagnosis similar to the previous group. Also, after diagnosis, short-term (1-2 hours) preoperative preparation was carried out, which included infusion, detoxification therapy using physiological solution, minerals and reosorbylact, taking into account indications up to 1 liter. According to the following, median laparotomy, revision of abdominal organs, clarification of the source of peritonitis, and identification of the prevalence of peritonitis in the abdominal cavity were performed under general anesthesia.Further surgical tactics aimed at eliminating the source of the lesion of diffuse peritonitis, sanitation and drainage of the abdominal cavity had their differences, which consisted in the method of drainage of the affected area of the abdominal cavity using a polygonal drainage tube. To determine the exact localization of each drainage in the postoperative period, the first drainage tube, which is installed under the transverse colon, the distal end was colored yellow, the second drainage tube, which is installed in the area of the mesentery root, the affected part of the peritoneum, was marked in green. The remaining drainage channels, which are installed in the affected area of the abdominal cavity, were colored red. The amounts of red color simultaneously showed the cleavage of the abdominal cavity area involved in the process of peritonitis. Drainage tubes are used mainly for two purposes: - to evacuate exudate from the abdominal cavity and to conduct local antibacterial therapy. Taking into account the nature and volume of discharge from various drainage tube channels, the dynamics of the inflammatory process in various affected areas of the abdominal cavity was indirectly assessed. With the study of qualitative and quantitative bacteriological studies from the isolation of the drainage tube, the tactics of antibiotic therapy were determined, taking into account the sensitivity of the microflora to antibiotics.We conducted empirical antibiotic therapy using Sulbactam or Cefaperazone. After sensitivity was detected, antibiotics were prescribed taking into account the sensitivity of the microflora. At the same time, the results of the individual intolerance test, which was carried out before the operating period, were taken into account. The upper-median access was used mainly for perforation of gastric and duodenal ulcers in 4 (66.6%) cases and for biliary peritonitis in 3 (75%) patients. Median laparatomic access in group II patients was used in 26 (56.5%) patients: - of these, appendicular peritonitis in 17 patients, gynecological peritonitis in 3 patients, fecal peritonitis in 3 cases, hemorrhagic peritonitis in 3 cases, median laparatomic access was used. In 6 (13.0%) patients of the control group, lower laparotomy access was used, of which 1 patient had appendicular etiology of peritonitis and 3 patients with Urinary peritonitis. Upper–middle –lower access was used in 7 (15.2%) patients who had sources of peritonitis: perforation of gastric and duodenal ulcers, fecal and hemorrhagic peritonitis in 2 cases and in one case with biliary peritonitis.The surgical stage of the operation was the elimination of the source of peritonitis in 46 patients of the control group, 18 (39.1%) patients were directed to eliminate the destructive appendicular process. In 9 (15.7%) patients, ectopic pregnancy was eliminated. In 5 (10.8%) patients with excision and suturing of perforation of ulcers of the stomach and duodenum (in 4 patients with suturing of a perforated gastric ulcer, in 2 patients with excision of a wound using Judd's pyloroplasty.In 5 (10.8%) cases, the damaged intestinal wall was pinched (in 3 patients, the walls of the large intestine, in 2 patients, the walls of the small intestine). Of the 5 patients with hemorrhagic peritonitis, 3 patients had intraperitoneal bleeding caused by damage to the parenchymal organ of the liver due to injury, in 2 cases ruptures of the mesentery, which was sutured during the operation with catgut sutures.We conducted empirical antibiotic therapy using Sulbactam or Cefaperazone. After sensitivity was detected, antibiotics were prescribed taking into account the sensitivity of the microflora. At the same time, the results of the individual intolerance test, which was carried out before the operating period, were taken into account. The upper-median access was used mainly for perforation of gastric and duodenal ulcers in 4 (66.6%) cases and for biliary peritonitis in 3 (75%) patients. Median laparatomic access in group II patients was used in 26 (56.5%) patients: - of these, appendicular peritonitis in 17 patients, gynecological peritonitis in 3 patients, fecal peritonitis in 3 cases, hemorrhagic peritonitis in 3 cases, median laparatomic access was used. In 6 (13.0%) patients of the control group, lower laparotomy access was used, of which 1 patient had appendicular etiology of peritonitis and 3 patients with Urinary peritonitis. Upper–middle –lower access was used in 7 (15.2%) patients who had sources of peritonitis: perforation of gastric and duodenal ulcers, fecal and hemorrhagic peritonitis in 2 cases and in one case with biliary peritonitis.The surgical stage of the operation was the elimination of the source of peritonitis in 46 patients of the control group, 18 (39.1%) patients were directed to eliminate the destructive appendicular process. In 9 (15.7%) patients, ectopic pregnancy was eliminated. In 5 (10.8%) patients with excision and suturing of perforation of ulcers of the stomach and duodenum (in 4 patients with suturing of a perforated gastric ulcer, in 2 patients with excision of a wound using Judd's pyloroplasty.In 5 (10.8%) cases, the damaged intestinal wall was pinched (in 3 patients, the walls of the large intestine, in 2 patients, the walls of the small intestine). Of the 5 patients with hemorrhagic peritonitis, 3 patients had intraperitoneal bleeding caused by damage to the parenchymal organ of the liver due to injury, in 2 cases ruptures of the mesentery, which was sutured during the operation with catgut sutures.In 3 (6.5%) patients with damaged bladder walls, suturing of damage to a part of the bladder was performed. In 4 patients with biliary peritonitis, the gallbladder was removed (in 3 cases, destructive cholecystitis, in 1 case, perforated destructive peritonitis).Analysis of the results of intoxication indicators in patients with diffuse peritonitis on the first day of treatment, the body temperature of patients averaged 39,5±0,42°C. The content of leukocytes in the blood was on average 9,9±0,17 х 109/l. The volume of the average molecules averaged 0,198±0,03 units. Similarly, an increase in LII and ESR was noted.On the third day of treatment, there was a slight decrease in body temperature from 39,5±0,42 to36,8±0,17, the number of white blood cells decreased to an average of 7,0±0,22×109//l. The volume of the average molecules averaged 0,116±0,007 units. There was a decrease in the indicators of LII and ESR to 1,1±0,04 and 24,5±1,13, respectively.By the fifth day of treatment in patients of group II with diffuse peritonitis, the body temperature index was 36,7±0,27°C. At the same time, according to all indicators of intoxication of the body: L, MSANTIMETER, LII and ESR of the blood, their further decrease was also noted, that is, there was a tendency to normalization – 6,5±0,1; 0,102±0,006; 1,0±0,03; 14,2±1,04 accordingly.Studies of the presence of paresis and the recovery time of intestinal peristalsis determined the following (Table 3).Table 3. The timing of the appearance of intestinal peristalsis in patients of the main group
 |
| |
|
As Table 3 shows, out of 46 examined patients with diffuse peritonitis of group II, 47.8% of patients were diagnosed with intestinal paresis clinic with complete absence of peristalsis on the day of admission. 52.1% of patients had mild or increased intestinal motility. In the postoperative period, against the background of complex treatment, stimulation of intestinal peristalsis was performed using proserin subcutaneously - 1-2 mg 1-2 times / day starting from the second day after surgery.Of the 22 patients who had paralytic intestinal obstruction, 18 (81.8%) patients showed signs of recovery of intestinal peristalsis on the second day of treatment, which manifested itself by listening to intestinal noise during auscultation, gas and stool discharge. There were improvements in the general condition of patients and well-being, appetite appeared. Against the background of complex treatment with the use of polycanal drainage with the introduction of antibiotics in the area under the transverse colon, the mesentery root of the small intestine and the affected areas of the abdominal cavity. Complications in the form of sluggish diffuse peritonitis were not observed in the main group of patients. That in the control group was observed in 7.0% of patients (Table 4).Table 4. Comparative analysis of postoperative complications and duration of inpatient treatment in patients of groups I and II
 |
| |
|
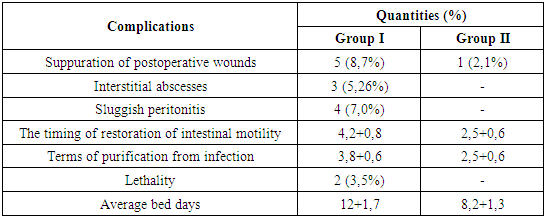
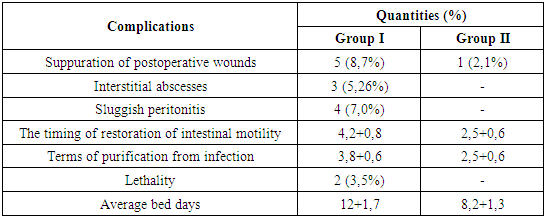
In the postoperative period, the 1st (2.1%) patient of group II had suppuration of the postoperative wound by 3 days after surgery, which, after appropriate local treatment with 25% dimexide solution and levamicol ointment, by 5-6 days passed to the 2nd and then to the 3rd phase of the wound process as in Table 4, shows identical complications in patients of the control group were observed in 8.7% of patients. When using the developed method of treatment of patients with diffuse peritonitis of the main group, inter-loop abscesses were not observed in the postoperative period. The time of purification from abdominal infection in the control group was 3.8 +0.6 days, and in patients of group II this indicator was on average 1 day ahead of the control group.Mortality was not observed in patients of group II. The average duration of inpatient treatment was 8.2+1.3 days.
4. Conclusions
1. The traditional method of treatment of diffuse peritonitis has a number of unsatisfactory results in the form of complications, suppuration of postoperative wounds 8.7%, inter-loop abscesses 5.26%, development of sluggish peritonitis 7.0%, mortality reaches up to 3.5%.2. When using a polycanal drainage tube, suppuration of postoperative wounds decreases to 2.1%, while inter-loop abscesses and sluggish peritonitis, mortality decreases by 5.26%, 7.0% and 3.5%, respectively, while the average inpatient treatment is 8.2+1.3 days.3. The use of a multi-channel drainage tube in the treatment of diffuse peritonitis with separate drainage under the transverse colon, the area of the mesentery root of the small intestine and each affected area of the abdominal cavity contributes to a reduction in postoperative complications and mortality than with traditional treatment methods. 4. In the treatment of diffuse peritonitis using a multi-channel drainage tube with separate drains, the affected areas of the abdominal cavity, the mesentery root of the small intestine and under the transverse colon with the introduction of antibiotics through tube microirrigators, taking into account the location of the drainage site, is a more optimal, improved treatment method.
References
| [1] | Jakobsson J. Perioperative regional anaesthesia and postoperative longer–term outcomes - Text: visual // F1000 Research. – 2016. – Vol. 5. – P. 1–7. |
| [2] | Ruiz–Patino A., Rey S., Molinа G. Cost–effectiveness of laparoscopic versus open appendectomy in developing nations: a Colombian analysis - Text: visual // J. Surg. Res. – 2018. – Vol. 224. – P. 33–37. |
| [3] | Dever J.B., Sheikh M.Y. Spontaneous bacterial peritonitis – bacteriology, diagnosis, treatment, risk factors and prevention - Text: visual // Alimentary Pharmacology & Therapeutics. – 2015. – Vol. 41, № 11. – P. 1116– 1131. |
| [4] | Sh.Sh. Yarikulov, A.I. Radjabov – Modern view on the diagnosis and treatment of acute cholecystitis in persons over 60 years of age // New Day in Medicine 2023 6(56): 64-72. https://newdaymedicine.com/index.php/2023/06/09/l-95/. |
| [5] | Vafoyeva, S. Yarikulov, Sh. (2023). Results of treatment of patients with liver cavities. International Bulletin of Medical Sciences and Clinical Research, 3(6), 204–209. https://researchcitations.com/index.php/ibmscr/article/view/2141. |
| [6] | Sh S. Yarikulov, AI Radjabov–Modern view on the diagnosis and treatment of acute cholecystitis in persons over 60 years of age. New Day in Medicine. 2023; 6(56) p. 64-72. |
| [7] | Biesen W.V., Brown E.A. Diagnostic and therapeutic approach to peritonitis - Text: visual // Nephrology Dialysis Transplantation. – 2017. – Vol. 32, № 8. – P. 1283–1284. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML