-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3163-3167
doi:10.5923/j.ajmms.20241412.16
Received: Nov. 26, 2024; Accepted: Dec. 13, 2024; Published: Dec. 16, 2024

Surgical Treatments for Esophageal Bleeding: Literature Review and Improved Approaches
Khakimov M. Sh.1, Kodirova G. R.2
1Head of the Faculty and Hospital Surgery Department No.1, Tashkent Medical Academy, Tashkent, Uzbekistan
2Assistant of the Department of General Surgery, Fergana Medical Institute of Public Health, Fergana, Uzbekistan
Correspondence to: Khakimov M. Sh., Head of the Faculty and Hospital Surgery Department No.1, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article provides a literature review of open surgical interventions performed for esophageal bleeding due to portal hypertension, where the main shortcomings of existing methods are indicated. Underwent open surgeries due to the ineffectiveness of minimally invasive interventions. 15 patients underwent the traditional Pacior operation. The analysis of the high frequency of recurrent bleeding showed that during open operations, the veins feeding the EGV are not always sutured, in particular the branches of the left gastric vein, which often have crossflows or can pass outside the walls of the stomach, which is sutured during the Pacior operation. The author proposed a technique for performing disconnection of the gastroesophageal collector, which made it possible to reduce the frequency of recurrent bleeding from 33% to 0%.
Keywords: Bleeding, Portal hypertension, Disconnection, Gastroesophageal collector
Cite this paper: Khakimov M. Sh., Kodirova G. R., Surgical Treatments for Esophageal Bleeding: Literature Review and Improved Approaches, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3163-3167. doi: 10.5923/j.ajmms.20241412.16.
1. Introduction
- One of the serious complications of portal hypertension (PH), developing against the background of liver cirrhosis (LC), is bleeding from varicose veins of the esophagus and stomach (VVEGS), leading to high mortality [1-7]. Many different methods of treatment of this complication have been proposed, indicating low efficiency of the proposed approaches and dissatisfaction with the results of their use. Despite the progressive development of medical technologies, the issues of choosing treatment tactics still remain controversial. Mortality after the first episode of bleeding reaches up to 50%, in 30% of patients, recurrent bleeding is observed during the first 6 months, in 70% of patients during observation periods of up to 1 year.The arsenal of treatment methods includes minimally invasive endovascular and endoscopic interventions, which are quite effective. However, despite their high effectiveness, open surgical interventions remain the operation of choice when minimally invasive methods are ineffective.The first attempts at surgical correction of PG were undertaken in the second half of the 19th century by N.V. Eck, who was the first to create an anastomosis between the vena Portae and veins cava inferior [3].The literature contains many different variations and methods of surgical treatment of PG, most of which have no clinical value and are part of the historical chronicle of the development of PG surgery.Depending on the timing of the surgical intervention, there are urgent ones, performed for emergency indications directly during bleeding from the esophageal varices, emergency-delayed ones, performed after the bleeding has stopped, and planned ones, performed for the purpose of preventing bleeding without any episodes of the latter in the anamnesis [4,5]. It is logical that planned surgical interventions are the most preferable, while emergency ones are an operation of “desperation” and are associated with high mortality rates and complications.Currently, surgical treatment methods for PG can be divided into the following types:1– “indirect”, in which bypass venous anastomoses are formed, which allow to reduce the pressure in the portal vein system;2– surgical techniques that involve ligation of the varicose veins;3– liver transplant.The most frequently used methods at present are the application of selective veno-venous anastomoses, in particular distal splenorenal anastomosis and mesenteric-caval H-shaped anastomosis using an autovenous patch or alloprosthesis. The positive aspects of these methods are the relatively low incidence of deaths and recurrent bleeding, and the reliability of hemostasis [6,7].The most frequent complication of these techniques is the development of thrombosis in the area of the imposed anastomosis, the frequency of which remains high. Recurrence of bleeding from varices of the esophagus after these operations ranges from 24% to 45% of cases, and the frequency of fatal outcomes after planned interventions reaches 8%, while after urgent ones it reaches 50% [4,6,8-11].In general, operations to form vascular anastomoses are recommended for patients of Child - Pugh class A with stable hemodynamics and no cognitive impairment [3,6,12].The most widely used operations in practice are those aimed at disconnecting the gastroesophageal collector. The most common complications of these operations are suture failure (frequency reaches up to 12%) and recurrent bleeding (incidence ranges from 8 to 20%). The fatality rate varies from 8 to 30% [13].The pioneers of surgical interventions for ligation of esophageal varices were J. Boerema (1949) and G. Crile (1950), who proposed to perform longitudinal esophagotomy through a thoracotomy approach followed by ligation of the esophageal varices with separate (Boerema) or continuous (Crile) sutures. The frequency of recurrent bleeding after these interventions reached 50%, and fatal outcomes – 75% [3,6,14].N. Tanner suggests performing subcardial gastrotomy 5 centimeters below the cardiac part of the stomach and suturing of varicose veins of the stomach. The disadvantage of this operation, in addition to its trauma, is the leaving of collateral extramural veins above the level of gastrotomy, which creates conditions for recurrent bleeding from the varicose veins, the frequency of which reaches 45% of cases. A number of authors have modified the Tanner operation, replacing the gastrotomy by clipping the stomach wall or applying ligatures to it [15].One of the most common operations in the CIS countries, including the Republic of Uzbekistan, is the operation of M.D. Patsior, proposed in 1959. The course of the operation consists of performing an upper-midline laparotomy, gastrotomy along the anterior wall from the bottom to the lesser curvature, suturing and ligation of the veins of the cardia, the proximal part of the stomach and the distal part of the esophagus for 5 cm above the cardiac transition, sutures are applied at intervals of 8-10 mm. Veins are suturing and ligating in a checkerboard pattern [4,7,14,16].The frequency of recurrent bleeding after the M.D. Pacior operation is 3-18.1% of cases, while their occurrence in the early postoperative period is associated with the cutting of sutures due to peristalsis, and in the late postoperative period - with ulcerative changes in the mucosa against the background of impaired blood supply. The frequency of fatal outcomes after the M.D. Pacior operation at the peak of bleeding reaches up to 31% [17,18].Domestic authors, headed by academician Nazyrov F.G., improved the Patsior operation. The authors performed a gastrotomy up to 3 cm long closer to the lesser curvature of the stomach, not reaching about 3 cm to the Mayo vein. A corrugated tube with a diameter of 2.5 cm is inserted into the lumen of the stomach through the gastrotomy opening, on which the stomach is sutured as on a frame, and the corrugation compresses the varicose vessels from the inside. Serous-serous sutures are applied, and the stomach is skeletonized and all venous collaterals are ligated. Mortality rates are about 25%, and recurrent bleeding is 5% [6,19,20].In a number of foreign clinics, the operation of M. Sugiura and S. Futagawa, developed in 1973, is performed. The essence of the operation consists of extensive devascularization, transsection of the esophagus, splenectomy, vagotomy and pyloroplasty. The results of this operation in the context of recurrent bleeding from esophageal varices are the best among surviving patients, but the frequency of fatal outcomes is extremely high in the late postoperative period [21].Sugiura operations was conducted, which showed that the fatality rate after urgent interventions reaches 55%, and after planned ones - 20%; recurrent bleeding was noted in 18%; 5-year survival varies from 52 to 78%, which depended on the initial condition of the patient [22,23].Some authors have tried to practice splenectomy in isolation, but its implementation does not reduce the volume of varicose veins in any way, but only reduces PG. Splenectomy is indicated only for segmental extrahepatic PG, leading to bleeding from the varicose veins of the stomach due to occlusion of the vena lienalis; in the presence of pathological communication between the arteria and vena lienales [18,24].Some authors included the following as indications for splenectomy: hypersplenism, however, according to statistics, there is no data confirming an improvement in the condition of patients and a decrease in mortality [3,6,18,25].Many authors believe that splenectomy during portal system disconnection is justified only in those situations when an enlarged spleen does not provide full access to the varicose veins, severe hypersplenism. Such narrow indications are due to the fact that performing splenectomy during disconnection operations increases mortality by 30% [19,26,27].A number of modern clinics are introducing methods of laparoscopic isolating operations. The essence of the operation is similar to open ones, but the trauma of the intervention is significantly reduced, despite its duration, which leads to a decrease in the frequency of fatal outcomes and recurrent bleeding [10,18,20]. Despite this, the complexity of performing these operations does not allow them to be introduced into routine practice.Considering the variety of approaches to surgical treatment of esophageal bleeding and their unsatisfactory results, we defined the aim of the study, which was to improve the surgical method of disconnecting the gastroesophageal collector and conduct its clinical evaluation.
2. Clinical Material
- The results of surgical treatment of 20 patients who were hospitalized in the emergency surgery department of the multidisciplinary clinic of the Tashkent Medical Academy for the period from 2010 to 2023 were analyzed. Depending on the treatment tactics, all patients were divided into two clinical groups: control and main. The control group included 15 patients who underwent the traditional Pacior operation. In the main group, 5 patients underwent the proposed method of disconnecting the gastroesophageal collector.
3. Results Obtained
- In the control group, 15 patients were subjected to open surgical treatment (after suturing of bleeding veins and Pacior's operation).Indications for surgical treatment were: 4 patients had profuse bleeding upon admission, attempts to install a Blackmore tube or perform endoscopic hemostasis were unsuccessful; in 5 cases after installation of a Blackmore tube, hemostasis was not achieved, despite reinstallation of the Blackmore tube and attempts to perform endoscopic hemostasis; in 3 cases after ligation recurrent bleeding was noted in varicose veins, which was the reason for open surgery; in 3 cases, repeated hemorrhage was noted after sclerotherapy sessions. Of the operated patients, recurrent bleeding was noted in 5 cases. All patients were re-operated. Intraoperatively, the source of bleeding was noted to be blood from the middle part of the esophagus. The operation was completed with intraoperative installation of a Blackmore tube. In the early postoperative period, a fatal outcome was noted in 3 cases. Percutaneous transhepatic portography with embolization of the left gastric vein, which made it possible to achieve hemostasis and save the patients' lives.When analyzing the results of selective phlebography, a sharply dilated left gastric vein was revealed, feeding the EGV (Fig. 1).
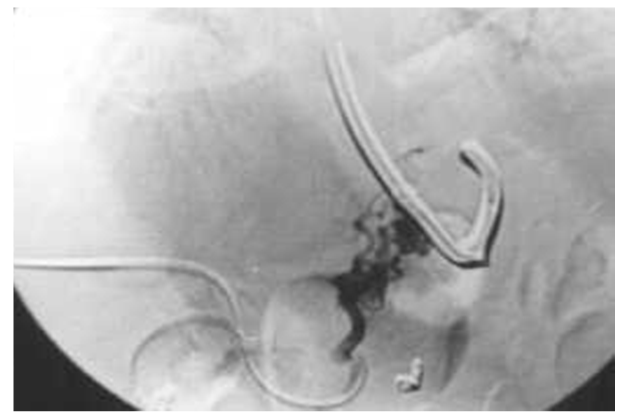 | Figure 1. Selective phlebography revealed a sharply dilated left gastric vein feeding the RV |
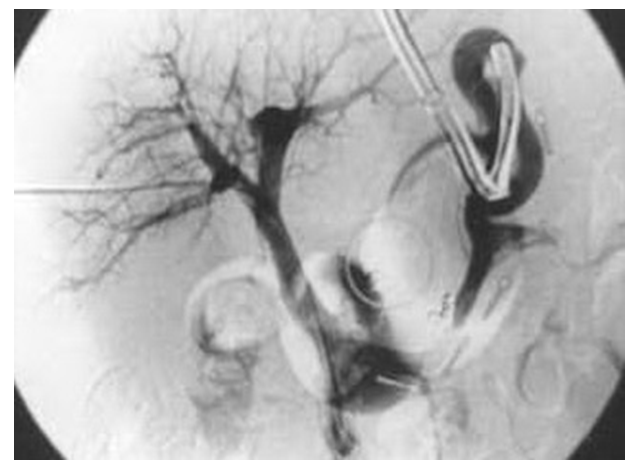 | Figure 2. Control portography of the VRV of the pancreas is not filled after interruption of the gastroesophageal collector |
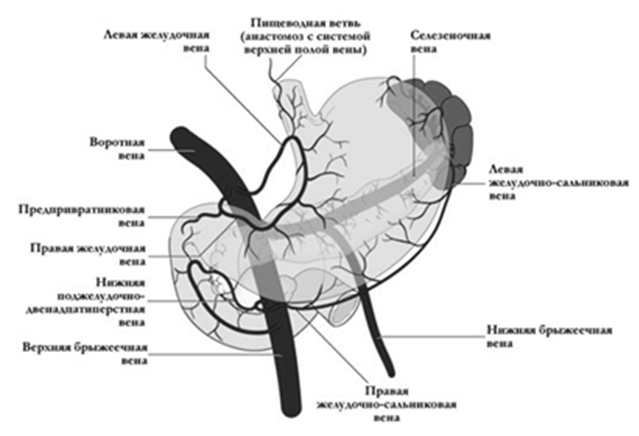 | Figure 3. Veins feeding the left gastric vein |
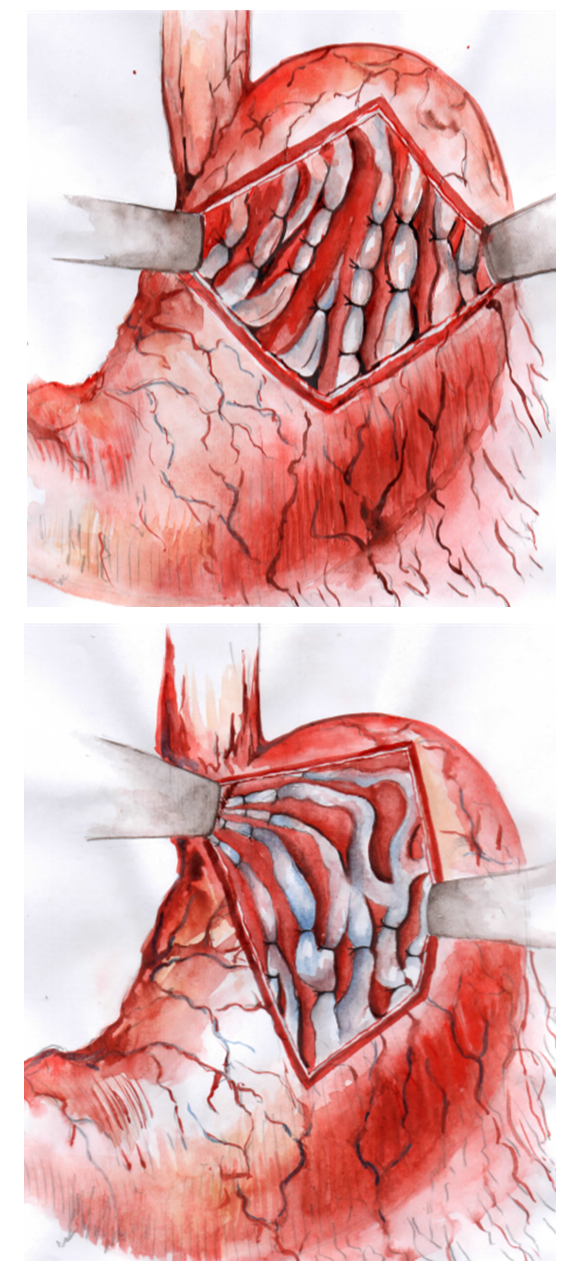 | Figure 4. Scheme of the operation of M.D. Patsior modified by us |
4. Conclusions
- 1. With a wide range of minimally invasive technologies in the treatment of bleeding from varicose veins against the background of portal hypertension, if the latter are ineffective, the method of choice is open surgical interventions aimed at disconnecting the gastroesophageal collector.2. The endovascular interventions performed have shown that during open surgeries, the veins feeding the EGV are not always sutured, in particular the branches of the left gastric vein, which often have cross-flows or can pass outside the walls of the stomach, which is sutured during the Pacior operation.3. The proposed method of disconnecting the gastroesophageal collector, which consists of suturing the dilated tributaries of the gastric vein in the area of transition of the lesser curvature of the stomach into the esophagus, allows to reduce the frequency of recurrent bleeding from 33% to 0%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML