-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(12): 3107-3109
doi:10.5923/j.ajmms.20241412.05
Received: Nov. 10, 2024; Accepted: Nov. 28, 2024; Published: Dec. 3, 2024

Improving Treatment Strategies for Acute Cerebrovascular Disease
Asadullaev Makhsud Makhmudovich1, Sohibnazarov Nodirjon Ghanijonovich2, Ataniyazov Makhsudjan Kamaliddinovich3, Vakhabova Nargiza Makhsudovna4
1Professor, Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbekistan
2Physician, Department of Neurology, Multidisciplinary Clinic, Tashkent Medical Academy, Tashkent, Uzbekistan
3Associate Professor, Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbekistan
4Doctoral Student, Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Asadullaev Makhsud Makhmudovich, Professor, Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article analyzes the effectiveness of dehydration therapy in reducing local cerebral edema during the treatment of cerebrovascular disease, specifically ischemic stroke. The analysis uses the NIH Stroke Scale (NIHSS) and Scandinavian Stroke Scale scores, along with hemodynamic indicators, to assess the severity and dynamics of neurological deficits.
Keywords: Tashkent Medical Academy, Ischemic stroke, NIHSS and Scandinavian scales, Duplex scanning, MSKT
Cite this paper: Asadullaev Makhsud Makhmudovich, Sohibnazarov Nodirjon Ghanijonovich, Ataniyazov Makhsudjan Kamaliddinovich, Vakhabova Nargiza Makhsudovna, Improving Treatment Strategies for Acute Cerebrovascular Disease, American Journal of Medicine and Medical Sciences, Vol. 14 No. 12, 2024, pp. 3107-3109. doi: 10.5923/j.ajmms.20241412.05.
1. Introduction
- Cerebrovascular diseases rank among the leading causes of death and disability. Globally, the annual incidence of primary strokes exceeds 15 million. This figure is approximately 750,000 in the US, 500,000 in Russia, 100,000 in Ukraine, and 40,000 in Uzbekistan. In Uzbekistan, the incidence of cerebral stroke is 0.9-1.5 per 1000 population. Globally, ischemic heart disease ranks first among causes of death, followed by stroke. Ischemic strokes are 5-6 times more frequent than hemorrhagic strokes: ischemic strokes account for 80-85% of all strokes, while hemorrhagic strokes account for 15-20%. Stroke is a process that develops over several minutes (sometimes several hours or days), ranging from simple functional changes in the brain to irreversible changes – necrosis [16].Ischemic stroke is the most common type of acute cerebrovascular accident, based on local cerebral ischemia, with diverse underlying causes. The most frequent causes of ischemic stroke development are atherosclerotic lesions of extra- and intracranial cerebral vessels, arterial hypertension, and their combined occurrence, as well as diabetes mellitus and the relatively less common, but currently increasing, cerebral vasculitis [1,2,12,15]. Numerous studies show that stenotic or occlusive changes in cerebral vessels, especially extracranial ones, are crucial in the development of ischemic stroke in 84-90% of cases [1,2,4,14]. Stenotic and occlusive changes in extracranial vessels are 2-5 times more common than in intracranial vessels [14,17]. Atherosclerotic changes in cerebral blood vessels lead to reduced cerebral blood flow and, consequently, excitation of the circulatory center in the medulla oblongata, resulting in vasoconstriction and increased arterial blood pressure.
2. Materials and Methods
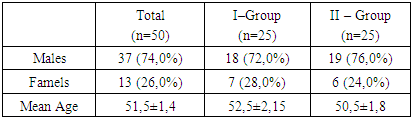
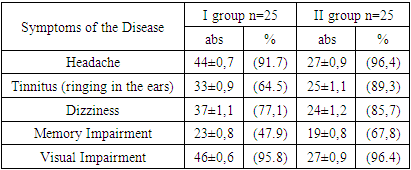
- Atherosclerosis contributes not only to the development of arterial hypertension but also to the exacerbation of existing hypertension [4,8,12,13,14]. The prevalence of arterial hypertension in patients with carotid artery stenosis is 72%. The combined occurrence of atherosclerotic lesions of the carotid artery and arterial hypertension further increases the risk of ischemic stroke [8,11,12].The widespread use of neuroimaging techniques has enabled accurate identification of ischemic stroke subtypes. Of all ischemic strokes, 34% are atherothrombotic, 22% cardioembolic, 15% hemodynamic, 20% lacunar, and 9% are of the hemorheological microocclusion type [1].In recent years, the significant role of cerebrovascular hemodynamic disturbances in the pathogenesis of cerebrovascular diseases has been emphasized. New pharmacological agents are being actively introduced into medical practice, their main effect aimed at treatment through normalization of brain tissue permeability, reducing the effects of ischemia and hypoxia, restoring microcirculation, and normalizing vascular tone. One such drug is Lidozinate. The drug quickly breaks down into lysine and aescin ions in the blood and readily crosses the blood-brain barrier. The main active substance determining the pharmacological properties of the drug is aescin. Lidozinate has endotheliotropic, venotonic, anti-inflammatory, and analgesic effects [3].Current research on ischemic stroke, despite the abundance of diagnostic methods assessing brain function and vascular status, often shows low treatment efficacy. This is due to the failure to consider the diversity of underlying processes, the etiology of this pathology, and the specific characteristics of vascular changes. Therefore, in cases of confirmed cerebral stroke, it is crucial to investigate the contributing factors, leading to a significant reduction in disability and mortality rates.Exclusion Criteria:• Patients with hyperdense lesions detected on CT scan.• Patients with severe somatic pathologies (myocardial infarction, pneumonia, cancer, decompensated diabetes), severe uncontrolled arterial hypertension (not controlled by antihypertensive drugs), and those receiving concomitant therapy with mannitol and/or saluretics were excluded from the study.Study Design:The study included 50 patients (n=50) who were randomly divided into two groups:• Group 1 (Control): 25 patients received standard baseline therapy and standard treatment for ischemic stroke.• Group 2 (Experimental): 25 patients received baseline therapy, standard treatment, and intravenous Lidozinate (10 ml in 100 ml of physiological saline) for 10 days to combat cerebral edema.Assessments:All patients (n=50) underwent clinical neurological (NIHSS and Scandinavian scales), angiographic (duplex scanning of neck vessels), and neuroimaging (brain CT scan on day 1) assessments on days 1, 2, and 10 of hospitalization.
3. Results and Discussions
- The mean age of patients in Group I (N=25) was 52.5 ± 1.4 years, with 72.0% (n=18) being male and 28.0% (n=7) female. The mean age of patients in Group II (n=25) was 50.4 ± 1.5 years, with 76.0% (n=19) being male and 24.0% (n=6) female (Table 1).
|
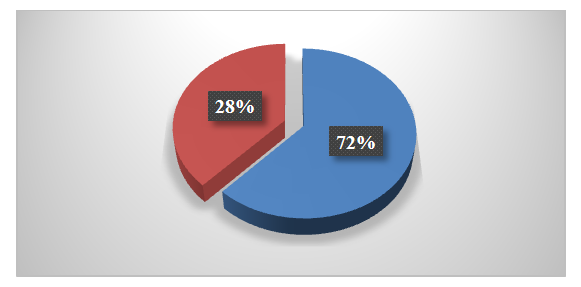 | Figure 1. Gender Distribution of Patients - Group 1 (n=25) |
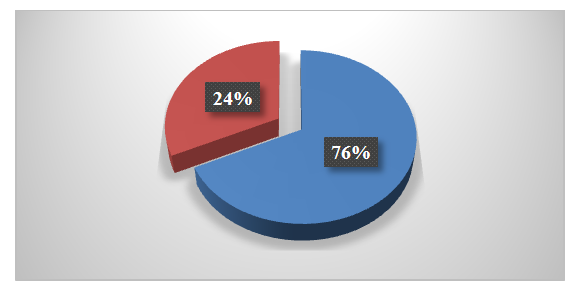 | Figure 2. Gender Distribution of Patients - Group 2 (n=25) |
|
4. Conclusions
- 1. Therefore, the study results demonstrate that the use of Lidozinate normalizes brain tissue permeability, reducing the impact of ischemia and hypoxia. This plays a crucial role in both early and late neuronal damage processes in acute ischemic stroke. Neurological scales showed a significant improvement in the clinical presentation of the disease, confirmed by a reduction in the severity of neurological deficit according to clinical indicators. The use of Lidozinate effectively improves intracranial blood flow due to improved venous circulation, which in turn leads to improved cerebral arterial perfusion.2. Atherosclerosis and pathological deformation of the carotid arteries are considered the main causes of ischemic stroke development. Over time, if reconstructive surgery of the carotid arteries is not performed in a timely manner, the degree of stenosis in the neck vessels increases, leading to an increased risk of ischemic stroke.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML