-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 3006-3009
doi:10.5923/j.ajmms.20241411.73
Received: Oct. 28, 2024; Accepted: Nov. 20, 2024; Published: Nov. 27, 2024

Regional and Modern Directions of Studying Specific Aspects of Comorbid Diseases in the Geront Population
Mamasoliev N. S.1, Sirojiddinov K. B.2, Botirov A. Q.3, Nishonova N. A.4, Mamasolieva Sh. A.5
1Head of the Department of Internal Medicine, Cardiology and Emergency Medicine, Andijan State Medical Institute, Andijan, Uzbekistan
2Doctor of Medical Sciences, Professor, Head of the Department of Surgical Diseases and Civil Defense, Andijan State Medical Institute, Andijan, Uzbekistan
3Head of City Administration, Independent Researcher of the Department of Doctor's Training and Training, Andijan State Medical Institute, Andijan, Uzbekistan
4PhD, Senior Lecturer, Department of Hospital Therapy and Endocrinology, Andijan State Medical Institute, Andijan, Uzbekistan
5Assistant, Department of Otorhinolaryngology, Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The authors of this literature review have analyzed the regional and modern directions of studying the characteristics of comorbid diseases in the geront population, showing the relevance and necessity of the topic. It can be concluded that the generally known scientific data shows that the study of the specific aspects of comorbid diseases in gerontological and geront age population groups in epidemiological studies is of great importance in revealing their modern trends, opening the horizons of primary and secondary prevention.
Keywords: Comorbid diseases, Geront population, Non-communicable diseases
Cite this paper: Mamasoliev N. S., Sirojiddinov K. B., Botirov A. Q., Nishonova N. A., Mamasolieva Sh. A., Regional and Modern Directions of Studying Specific Aspects of Comorbid Diseases in the Geront Population, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 3006-3009. doi: 10.5923/j.ajmms.20241411.73.
1. Introduction
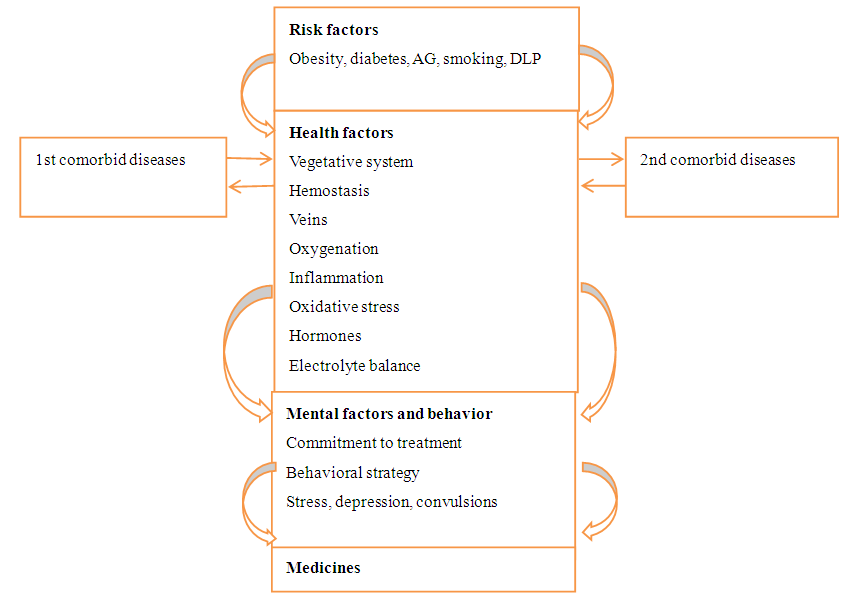
- In recent years, the problem of studying the characteristics of comorbidity and non-communicable diseases that are most "underlying" for it has been raised and discussed at different levels (state, society, science, practice, different population groups, including the geront population) [18,22].Major non-communicable diseases that cause comorbidity are the main cause of all deaths and disabilities worldwide. In this direction, obtaining scientific results and creating measures for practice to fundamentally improve the quality of medical services provided to the population is considered an important topic and an urgent, necessary issue for practice.In this regard, a special decision of the President of the Republic of Uzbekistan "On additional measures to deepen the reforms in the health sector" was adopted, aimed at deepening the reforms being implemented [5]. The issue of increasing the efficiency of prevention of non-communicable diseases is given priority in the "Uzbekistan-2030" strategy, and cardio comorbidity is given special priority.Gerontological comorbidity deserves special attention. Because no human organ, especially in geronts, can perform its activities alone. Separate diseases are almost absent in the geront population, they "appear", "pass" and "complicate" against the background of comorbidity.A.L. Vertkin (2012) summing up his researches of different years, described the following characteristics of comorbidity in different populations, especially in the geront age population: 1) the concept of "comorbidity" (more than 2 coexisting diseases) in 1979 Alvan Feinstein (American epidemiologist and the researcher) introduced to science, confirmed the increase of bad consequences in patients depending on it; 2) in recent years, comorbidity has been separated and developed as a separate research area; 3) comorbidity is a pathological condition associated with the pathogenesis of a single cause or a single mechanism, sometimes manifesting with similar clinical manifestations, and it is difficult to distinguish them; 4) transsyndrome (a combination of pathogenically related diseases or syndromes), transnosological (such a combination of nosologies) and chronological comorbidity (temporary combination) are classified by most researchers; 5) the terms "polymorbidity", "polypathy", "multimorbidity", "multifactorial diseases", "harmonious disease", "dual diagnosis" and "pluripathology" are proposed and used by researchers as synonyms of comorbidity; 6) in recent years, comorbidity is defined as a large number of diseases with a single pathogenetic mechanism, and multimorbidity is defined as a large number of diseases for which a single pathogenetic mechanism has not been proven; 7) in general, this term is clarified in the sense that the combination of several specific chronic diseases is called comorbidity (Kraeter N.S.); 8) inflammation, chronic infections, metabolic disturbances, iatrogenicity, social status, environmental factors and genetic predisposition are confirmed as comorbidity factors [2].According to the scientific data provided by this author based on the literature review, age-related comorbidity is determined among the population with varying frequency: 69% in 18-44-year-olds, and up to 98% in the gerontological and geront population over 65 years old. The number of chronic diseases is on average 2.8 in young people, and up to 6.1 in the elderly population.However, these data were obtained by the researchers mainly in the last years of the last century, and it is clear from the review of the literature that currently there are not enough epidemiological studies dedicated to comorbidity. In the geront population, under the conditions of Uzbekistan, there are no such scientific results, on special epidemiological-prophylactic research.However, the task of treating and preventing comorbidity was recommended by WHO as a priority project of the 21st century [2].One of the achievements of 21st century medicine is the reduction of death and disability of the population from cardiovascular system diseases (CVDs), especially CHDs, in a number of foreign countries. However, this process itself has led to an increase in life expectancy, an increase in morbidity and comorbid conditions, and an increase in the burden of comorbidity, especially in the geront population [14,15].In particular, the important issue of revascularization in the geront population remains open due to a certain degree of comorbidity.Ahrens I. et al. (2019) in the group of patients of gerontological age in emergency cardiology departments, revascularization is performed only in 7% of cases due to the reason mentioned. In this group, high-risk group, high frequency of left ventricular failure and high mortality are confirmed. This process, "treatment-risk paradox", is considered to be the same for the population of almost all countries [6].Hindricks G. et al. (2020) scientific observations prove that the most common reasons for not performing revascularization in the geront population are the high frequency of coronary artery disease (CHD) and multivessel damage of the coronary vessels (as a comorbidity). Judging from the latest clinical recommendations, it is clear that diagnostic and treatment algorithms in geront age are the same as in patients belonging to the younger category [13].Therefore, in the latest (2020) recommendations of the European Society of Cardiology, expansion of research in the directions indicated in the geront population and, first, in the preventive direction is highlighted as an actual problem [3].As a result of limitations in the use of modern treatment technologies in the geront population, mainly due to comorbidity, in the gerontological age population, in-hospital death from myocardial infarction is recorded as 7.8% in 65-74-year-olds and 17.7% in those over 75 years old. This indicator is 19 times higher than in people aged ≤65 years (1.2%), which confirms the existence of a cardiogerontological problem related to comorbidity, and it is an increasingly urgent scientific topic. Cardiogenic shock (80%), brain tumor (10%) and polyorgan deficiency (10%) are confirmed as the main causes of death from myocardial infarction against the background of geront comorbidity [4].There is increasing scientific evidence in the literature that comorbidity in SCI increases or exacerbates the resulting "hard end points" associated with it. Boytsow S.A. and everything. (2018) cites data on ICU, indicating that the current epidemiological situation of the disease has become more serious. In almost all countries, it is considered the main cause of death and disability of the population. In Russia, the death rate from coronary artery disease is 322 per 100,000, and the death from myocardial infarction is confirmed as 40 per 100,000 population per year [8].Barbarosh O.L. et al. According to (2019), coronary bypass graft (CABG) is the leading surgical technology used to restore coronary flow in ICU, and the need for it is increasing year by year. In different countries - from 50 operations (in Germany, Poland) to 24.5 operations (in Russia) per 100,000 population. In such conditions, the correct selection of the patient for ASh is of vital importance, in particular, comorbid pathologies reduce the level of its positive results and increase the risk of postoperative complications and death [7].Piksiin I.N. et al. According to the research results presented by (2007), the reason for this is the influence of operational stress as an "aggressive" factor. The use of artificial blood circulation (ABC) in surgery causes oxygen starvation (hypoperfusion) in tissues, and as a result, functional-metabolic disturbances occur, intermediate products of metabolism accumulate in cells. ASH has a negative effect on all components of the oxygen transport system - respiratory, circulatory, hemic and tissue [20].Any types of comorbid pathologies are considered an additional factor that worsens the state of hemocirculation and increases the risk of reperfusion disorders in patients with ICU. In CB, therefore, careful volumetric and hemodynamic monitoring is recommended, especially, for example, the use of transpulmonary thermodilution technology. The use of such technology in the CHHD passing on the background of comorbidity, Mareev V.V. and everything. According to (2018), it reduces the risk of surgery by making possible early diagnosis and elimination of pulmonary hemodynamic disorders and tissue oxygenation [16].Cardiovascular, respiratory, and metabolic comorbidity in ischemic heart diseases is mostly confirmed in the following forms: IHD+DPA (damage of peripheral arteries), IHD +CHOPD (chronic obstructive pulmonary disease), IHD +MS (metabolic syndrome). Rublev V.Yu and others. (2020) NYHA class II-III heart failure and/or AG II-III class are diagnosed in any comorbidity of HF. In the absence of appropriate therapy or preventive pharmacotherapy, the level of "aggression" of CB will increase [21].For example, in patients with "ChHD+MS", extravascular fluid accumulation increases and as a result, intra-abdominal pressure increases, functional activity of the diaphragm decreases, lung volumes are limited, microatelectation develops in the basal segments of the lungs, and vasoconstriction increases due to an imbalance in the synthesis of adipokines. or increases the risk of CB [19].Belyalov F.I. (2022) showed the characteristics of comorbid diseases in the gerontological age population and attributed their interaction mechanisms to 4 factors (risk factors, somatic factors, mental factors and behavioral drugs) as follows [1].
 | Figure |
2. Conclusions
- The generally known scientific data show that the study of the specific aspects of comorbid diseases in gerontological and geront age population groups in epidemiological studies is of great importance in revealing their modern directions, opening the horizons of primary and secondary prevention.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML