-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2989-2992
doi:10.5923/j.ajmms.20241411.69
Received: Nov. 1, 2024; Accepted: Nov. 21, 2024; Published: Nov. 27, 2024

Improvement of Complex Treatment of Exudative-Hyperemic and Erosive-Ulcerative Forms of Red Flat Iron on the Mucous Membrane of the Oral Cavity
Sabirov Shukhrat Solijonovich
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Sabirov Shukhrat Solijonovich, Bukhara State Medical Institute, Bukhara, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study analyzes comprehensive treatment methods for the exudative-hyperemic and erosive-ulcerative forms of oral lichen planus (OLP) affecting the oral mucosa. OLP is a disease with a severe course, challenging treatment, and a high likelihood of malignant transformation. The study identifies the prevalence of various OLP forms among patients of different ages and its associations with systemic diseases and harmful habits. The results demonstrate that comprehensive treatment is effective in reducing OLP symptoms and improving quality of life.
Keywords: Mouth space mucus floor, Red flat iron, Exudative-hyperemic form, Erosive-ulcerative form, Complex treatment, Somatic diseases, Harmful habits
Cite this paper: Sabirov Shukhrat Solijonovich, Improvement of Complex Treatment of Exudative-Hyperemic and Erosive-Ulcerative Forms of Red Flat Iron on the Mucous Membrane of the Oral Cavity, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2989-2992. doi: 10.5923/j.ajmms.20241411.69.
1. Introduction
- Oral lichen planus (OLP) is one of the most prevalent diseases affecting the oral mucosa (SMF), distinguished by its unknown etiopathogenesis, the presence of severe forms, a wide range of symptoms, potential for malignant transformation, and frequent resistance to therapy. These characteristics underscore its significant medical and social importance. [1] Among the different forms of OLP is the erosive-ulcerative form o damage to the mucous membrane of the oral cavity and the red border of the lips, the disturbance of eating due to pain, which leads to a decrease in the quality of life of patients. [2] Factors provoking the development of OLP develop as a result of a violation of the microbiocenosis of the oral cavity, a decrease in local and general immunity, stress, an increase in related somatic diseases, and the reception of certain drugs. Solving the problem of effective treatment of SMF OLP remains an urgent problem in dental practice [3].Erythematous flatulence on the mucous membrane of the oral cavity (OLP) is one of the common, difficult to treat diseases, the etiology and pathogenesis of which have not been fully determined. According to scientific sources, OLP is important among inflammatory diseases of the oral mucosa, because it is characterized by pain, inconsistency and the possibility of transition to a poor quality form [4]. The severe course of OLP and its resistance to treatment prompt doctors and researchers to study this disease in depth [5].There are different forms of OLP, among which exudative-hyperemic and erosive-ulcerative forms are of particular importance. These forms present with obvious signs on the oral mucosa and are painful for patients, affecting eating, speaking and daily activities (Silverman, 2005). The fact that severe forms of the disease in rare cases have the risk of transition to low-quality tumors indicates the need to study OLP as one of the important medical problems [6].Recent studies confirm the role of various factors, including genetic, immunological, and psychogenic factors in the development of OLP. Stress conditions and related somatic diseases are among the factors that stimulate the development of OLP [7]. Therefore, it is important to use integrated approaches to increase the effectiveness of treatment of OLP.Various studies show that in the pathogenesis of OLP, the decrease of local and general immunity, the disturbance of the microbiocenosis in the oral cavity, and the effect of certain drugs are significant [8]. Accordingly, there is a need to improve therapeutic methods for effective treatment of various forms of the disease.The relevance of the research is determined by the fact that the complexity of the pathogenetic mechanisms associated with OLP in the mucous membrane of the oral cavity creates difficulties in the complete elimination of this disease. Therefore, the issue of increasing the effectiveness of complex treatment of exudative-hyperemic and erosive-ulcer forms of OLP in the mucous membrane of the oral cavity and improving the quality of life of patients remains an important problem in dental practice.The purpose of the study: improvement of complex therapy aimed at increasing the effectiveness of treatment of exudative-hyperemic and erosive-ulcer forms of erysipelas on the mucous membrane of the oral cavity.
2. Research Material and Method
- 122 people from 18 to 80 years old who were diagnosed with red squamous cell carcinoma of the oral mucosa (exudative-hyperemic and erosive-ulcer forms) were included in the study. the average age was 56.28±3.78 years. The average age of men (n=32) was 58.09±5.12 years, and the average age of women (n=90) was 54.47±2.44 years. The age of patients suffering from different forms of erysipelas was comparatively evaluated in SMF. The analysis showed that the average age of patients with the exudative-hyperemic form of SMF OLP was found to be significantly lower than that of patients with the erosive-ulcerative form of scarlet fever: 50.54±2.38 years in the exudative-hyperemic form, 50.54±2.38 years in the erosive-ulcerative form and 62.02±5.18 years old (p<0.05) indicators were analyzed. The WHO showed the indicators of the distribution of patients by gender. The exudative-hyperemic form was recorded in 13 (21.67%) men and 47 (78.33%) women, and the erosive-ulcerative form was recorded in 19 (30.65%) men and 43 (69.35%) women. (p>0.05).
3. Research Results
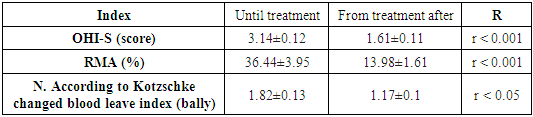
- During the study, in the exudative-hyperemic and erosive-ulcerative forms of SMF OLP, a case of somatic diseases meeting one by one at the same time was observed. Gastrointestinal tract (GIT) diseases (chronic gastritis, cholecystopancreatitis, liver diseases, colitis), cardiovascular system (CHD) pathology (ischemic heart disease, atherosclerosis), and nervous system diseases (encephalopathy, cerebral circulation disorders) the number of patients was found to be high. At the same time, it should be noted that the reliable superiority of the erosive-ulcerated form of the red flat iron in the oral cavity in patients with diseases of the cardiovascular system has gained great importance. (p<0.05). In addition, there are other groups and types of somatic diseases, endocrine system diseases (diabetes, hypothyroidism and obesity) and urogenital system (STT) diseases (nephrotic syndrome, kidney stone disease, pyelonephritis, endometriosis in women, chronic prostatitis and prostate gland in men) adenoma) in patients with oral cavity red flat iron erosive-ulcerative type was observed much more than exudative-hyperemic type (p<0.05).Local exogenous risk factors for the occurrence of OLP were identified during oral cavity examination: the presence of sharp edges of teeth and roots, the unsatisfactory condition of fillings in 57% of patients, the presence of metal prostheses made of dissimilar metals in 27%, the use of colored plastics for prosthetics were identified in 8% of patients. KPU index of tooth caries intensity was 18.85±0.9. In the analysis of the KPU index in patients, patients with OLP before treatment had an index of "K" equal to 3.77±0.6, 20% of which was equal to "P" equal to 5.63±0.6, corresponding to 30%, "U" equal to 9,37±1.04, corresponding to 50%. After treatment, the "K" indicator was 97±0.38, the "P" indicator was 8.0±0.71, the "U" indicator was 9.8±1.03, respectively 5% of the KPU index value, It was 43% and 52% (Fig. 1).
 | Figure 1. Indicators of KPU index before and after treatment in patients with OLP |
|
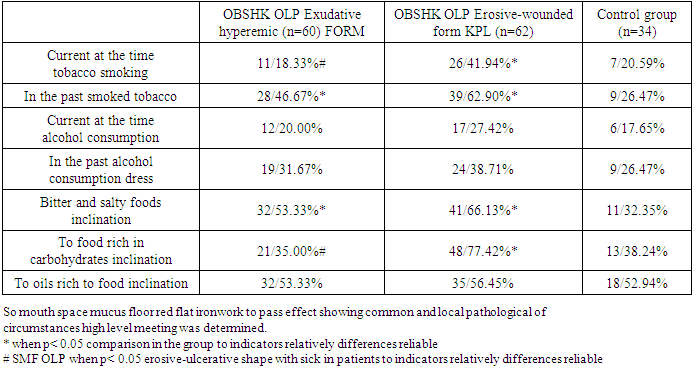
 | Figure 2. Dynamics of the OHI-S index in patients with OLP after complex etiopathogenetic treatment |
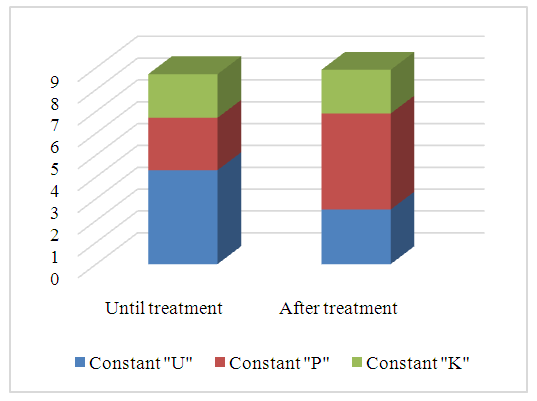
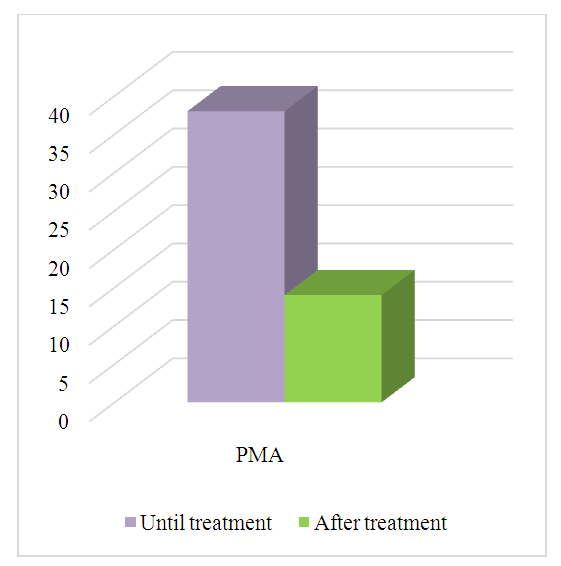 | Figure 3. Complex etiopathogenetic from treatment then with OLP hurt of the RMA index in patients dynamics |
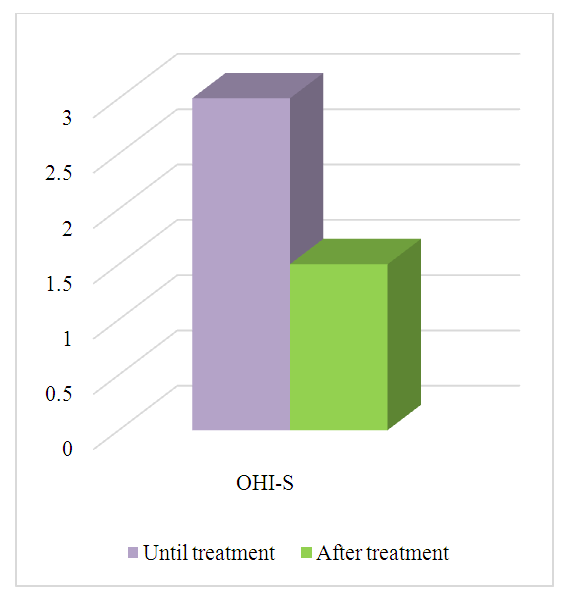
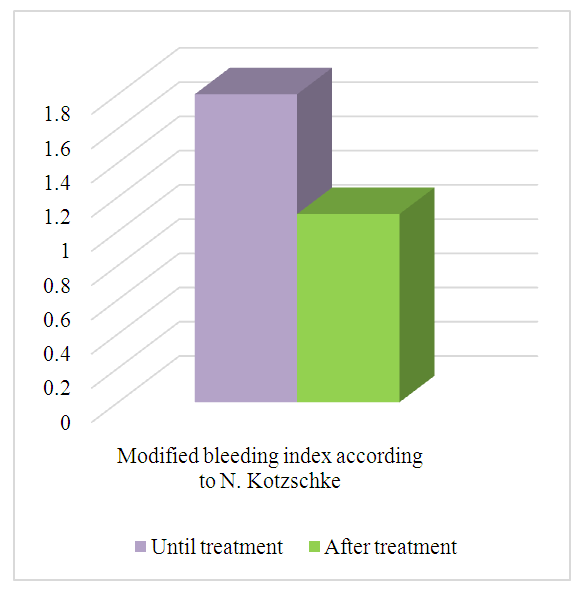 | Figure 4. Complex etiopathogenetic from treatment then with OLP hurt in patients N. Kotzschke according to modified blood leave |
|
4. Conclusions
- Mouth space mucus on the floor red flat of iron exudative-hyperemic and erosive-ulcerative forms efficient treatment methods improvement the necessity of the disease different of forms prevalence, gender and age differences, and of the disease different risk factors with dependence was determined. Research to the results according to complex treatment efficiency high being a mouth space mucus on the floor inflammation symptoms reduce and of patients life quality to improve help to give known it happened.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML