-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2977-2980
doi:10.5923/j.ajmms.20241411.66
Received: Nov. 2, 2024; Accepted: Nov. 23, 2024; Published: Nov. 26, 2024

Features of the Clinical Course of Chronic Sinusitis in Patients with Type 2 Diabetes Mellitus
Feruza Alimovna Khaydarova, Shavkat Ergashovich Amonov, Elmira Sagdullayevna Khodjaeva, Feruza Farrukhovna Khudoyberdiyeva
Republican Specialized Scientific and Practical Medical Center of Endocrinology named after Y. Kh. Turakulov, Tashkent Pediatric Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents the results of clinical and biochemical indicators of chronic sinusitis in patients with type 2 diabetes mellitus (T2DM). It details the demographic data, nosological forms of chronic sinusitis (CS), as well as the microflora indicators from nasal secretions in T2DM patients with chronic sinusitis. The aim of the study is to analyze the clinical and biochemical indicators of chronic sinusitis in patients with type 2 diabetes. Materials and Methods: The study involved the examination of 130 patients, including 80 patients with chronic sinusitis on the background of type 2 diabetes (Group 1, main group) and 50 patients with type 2 diabetes without chronic sinusitis (Group 2, control group), who received treatment at the Republican Specialized Medical Center of Endocrinology named after Y. Kh. Turakulov. Results: The analysis of clinical and laboratory studies of patients with chronic sinusitis on the background of type 2 diabetes (Group 1) reveals that the studied parameters reflect the activity and severity of the inflammatory process in the paranasal sinuses. Conclusions: The distinctive clinical features of chronic sinusitis in patients with diabetes mellitus include the rapid progression of the primary disease and the systemic inflammatory response syndrome. This can lead to complications and even unfavorable outcomes, particularly in patients with poor glycemic control. Patients with type 2 diabetes more frequently presented with productive (35%) and exudative forms (32.5%) of chronic sinusitis. An important principle of pathogenetic therapy is continuous blood glucose monitoring and etiological treatment targeting the causative agent of sinusitis. The main group of patients was characterized by a higher prevalence of overweight and obesity, a family history of type 2 diabetes, and lower physical activity compared to the control group.
Keywords: Type 2 diabetes mellitus, Chronic sinusitis, ENT organs, Paranasal sinuses
Cite this paper: Feruza Alimovna Khaydarova, Shavkat Ergashovich Amonov, Elmira Sagdullayevna Khodjaeva, Feruza Farrukhovna Khudoyberdiyeva, Features of the Clinical Course of Chronic Sinusitis in Patients with Type 2 Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2977-2980. doi: 10.5923/j.ajmms.20241411.66.
Article Outline
1. Introduction
- The presence of concomitant somatic pathology in patients and the combined course of focal infections, both from social and medical perspectives, is a pressing issue in modern medicine. Among the frequently encountered underlying conditions, diabetes mellitus (DM) stands out as one of the most severe in terms of progression and outcomes, being a significant problem not only medically but also socio-economically worldwide.Despite the availability of numerous conservative and surgical methods for treating ENT organ pathologies, inflammatory diseases of the nose and paranasal sinuses are fraught with various complications. These conditions often contribute to the development of systemic inflammatory syndrome and increase the frequency of orbital rhinogenic complications, ranging from 6.6% to 12.4% [1,3]. Patients with DM are more susceptible to various ENT diseases. In this pathology, depending on the pathogen and its pathogenic, virulent, and invasive properties, immune disorders, both systemic and local, play a significant role, as do disruptions in the interaction of various components of the immune system [1,2].Studies by Prentki M. and Nolan C. J. (2006) have shown that oxidative stress caused by hyperglycemia triggers mechanisms that damage pancreatic β-cells, thereby accelerating the progression of diabetes mellitus [5] and the development of local infections. Purulent infections worsen metabolic disorders, rapidly leading to decompensation of carbohydrate metabolism and ketoacidosis, which aggravates the course of infection and results in adverse complications in 13% of DM patients [6,7].The aim of the study is to examine some clinical and biochemical indicators of chronic sinusitis in patients with type 2 diabetes mellitus.
2. Materials and Methods
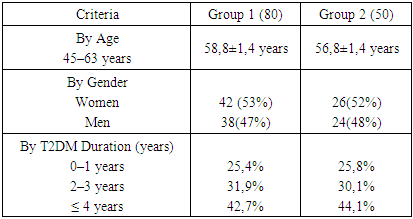
- A study was conducted on 130 patients, including 80 patients with chronic sinusitis (CS) on the background of type 2 diabetes mellitus (T2DM) and 50 patients with diabetes mellitus without chronic sinusitis. All patients received treatment at the Republican Specialized Scientific and Practical Medical Center of Endocrinology named after Y. Kh. Turakulov. The age of patients in the study groups ranged from 45 to 85 years (mean age 58.8 ± 1.4 years), with 84 (53%) women and 76 (47%) men. The duration of T2DM ranged from 1 to 27 years (mean 6.5 ± 3.6 years). The duration of chronic sinusitis ranged from 1 to 8 years (mean 3.5 ± 1.5 years).All patients underwent standard examinations, which included collecting complaints, disease history, quality of life assessment, measurement of height and weight, and ENT examinations using standard techniques: including endoscopy, rhinoscopy, pharyngoscopy, otoscopy, and laryngoscopy. Additional imaging studies such as MRI and 3D X-ray of the paranasal sinuses were performed, along with microbiological analysis of nasal sinus secretions. Biochemical blood tests were also conducted, including fasting blood glucose, glycated hemoglobin levels, cholesterol levels, high-density lipoprotein levels, and triglyceride measurements.
3. Results and Discussion
- The demographic analysis showed no significant differences between the two groups in terms of gender and age distribution, with 42 (53%) men and 38 (47%) women in one group, and 26 (52%) men and 24 (48%) women in the other group, respectively. The duration of type 2 diabetes mellitus ranged from 1 to 27 years, with an average duration of (6.5 ± 3.6) years (Table 1).
|
|
|
|
4. Discussion of the Results
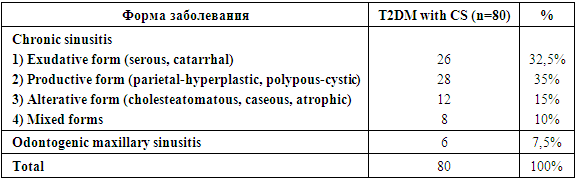
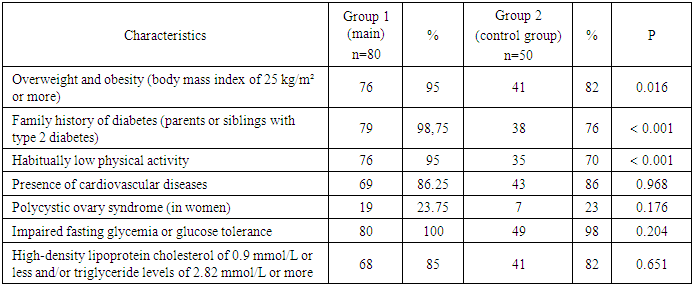
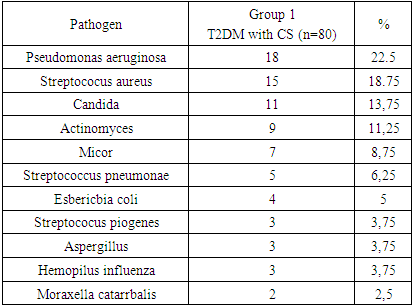
- Analyzing the data from patients with chronic sinusitis on the background of type 2 diabetes (main group), it can be concluded that these parameters primarily reflect the activity and severity of the infectious process. Patients with type 2 diabetes more frequently had the productive form (35%) and exudative form (32.5%) of chronic sinusitis. Individuals with a history of diabetes are more prone to various ENT diseases [1,2]. Depending on the pathogen and its pathogenic, virulent, and invasive properties, immune disturbances, both systemic and local, play a significant role, as do disruptions in the interaction of various components of the immune system [3,4]. According to Tappia P. S. et al. (2006), conditions for this form arise with increased oxidative substrates (glucose, lipids) and reduced activity of natural antioxidants [5].Research by Prentki M. and Nolan C. J. (2006) indicates that oxidative stress caused by hyperglycemia triggers a mechanism that damages pancreatic β-cells, accelerating the progression of diabetes [6]. A reduction in specific local resistance parameters in diabetic patients without inflammatory ENT pathology (2nd control group) is attributed to secondary immunodeficiency against the backdrop of chronic hyperglycemia [7,8]. Purulent infections exacerbate metabolic disorders, rapidly leading to decompensation of carbohydrate metabolism and ketoacidosis [9], which worsens the infection course and causes fatal complications in 13% of diabetes patients [10,11]. The increased susceptibility to infections and purulent-septic conditions in diabetic patients is largely due to reduced general and local immune resistance in the context of chronic hyperglycemia [12,13].This is evidenced by the growing number of consensus documents regularly appearing in European and U.S. countries, based on new evidence-based research and meta-analysis data. However, the criteria for disease reporting and the algorithms for diagnosing and treating rhinosinusitis vary significantly between countries, with these differences being more pronounced for chronic sinusitis (CS) [14,15]. In this category of patients, Pseudomonas aeruginosa 18 (22.5%), S. aureus 15 (18.75%), fungal pathogens Candida 11 (13.75%), Actinomyces 9 (11.25%), and Micor 7 (8.75%) were identified, which underscores the importance of selecting appropriate antibiotics in the treatment strategy for these patients.An important principle of pathogenetic therapy is the continuous monitoring of blood glucose levels, as in the main group of patients with type 2 diabetes and chronic sinusitis, fasting glycemia disorders were observed in 80 (100%) cases, elevated cholesterol in 68 (85%), and overweight and obesity (BMI of 25 kg/m² or more) in 76 (95%). The main group of patients was characterized by a significantly higher prevalence of overweight and obesity, a family history of type 2 diabetes, and lower physical activity compared to the control group. At the same time, indicators such as the presence of cardiovascular diseases, polycystic ovary syndrome, and metabolic markers did not show significant differences between the groups.
5. Conclusions
- In patients with type 2 diabetes, chronic sinusitis is more frequently associated with Pseudomonas aeruginosa, S. aureus, and fungal pathogens such as Candida, Actinomyces, and Micor, highlighting the need for careful antibiotic selection in the treatment strategy for these patients.Effective treatment of chronic sinusitis in the context of type 2 diabetes should be etiotropic, directly targeting the pathogen while also considering the systemic complications of antibiotic therapy.An important principle of pathogenetic therapy is the continuous monitoring of blood glucose levels. Additionally, patients in the main group more commonly presented with obesity, a family history of diabetes, and low physical activity, whereas other parameters did not differ between the groups.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML