-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2968-2971
doi:10.5923/j.ajmms.20241411.64
Received: Oct. 22, 2024; Accepted: Nov. 10, 2024; Published: Nov. 26, 2024

Aspects of Surgical Treatment of Acute Biliary Pancreatitis
Rizayev Ezozbek Alimdjanovich , Kurbaniyazov Zafar Babajanovich , Abdurahmanov Diyor Shukurullaevich
Samarkand State Medical University, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents an analysis of the treatment of patients with moderate to severe acute biliary pancreatitis – 79 (30.3%) patients. EPST effectively resolves obstruction of the bile and pancreatic ducts in acute biliary pancreatitis and eliminates ductal hypertension, which are the main cause of purulent cholangitis and pancreatic necrosis. Cholecystectomy, mainly laparoscopic, is advisable to perform after conservative resolution of mild biliary pancreatitis within 24 hours after the attack due to the risk of relapse of the disease. After EPST, cholecystectomy is also justified without discharge from the hospital if papillotomy is performed without complications. In acute biliary pancreatitis complicated by sterile or infected fluid accumulations, cholecystectomy should be postponed until their complete resolution and elimination of systemic inflammatory reactions.
Keywords: Acute biliary pancreatitis, Severe clinical course, Minimally invasive interventions
Cite this paper: Rizayev Ezozbek Alimdjanovich , Kurbaniyazov Zafar Babajanovich , Abdurahmanov Diyor Shukurullaevich , Aspects of Surgical Treatment of Acute Biliary Pancreatitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2968-2971. doi: 10.5923/j.ajmms.20241411.64.
Article Outline
1. Relevance
- Acute biliary pancreatitis (ABP) is a common disease, occurring in 25-30% of the total number of sick acute pancreatitis and in 15-25% it occurs in a severe form. Its main causes are the existence of gallstone disease, anatomical relationships of the general bile and main and pancreatic ducts and embryonic development between them of the “common channel”, microlithiasis, wedging and migration of stones through the major duodenal papilla [1,4].Currently active promotion is being promoted surgical tactics for the treatment of cholelithiasis, widespread introduction of laparoscopic cholecystectomy and endoscopic retrograde pancreato- and cholangiography with the possibility of performing papillotomy and stone extraction. However, the results of surgical treatment of patients with AP leave much to be desired, since in severe forms of this disease the mortality rate reaches 15-30%. Therefore, general and local complications of AP that arise during the long course of the disease dictate the need to develop reasoned recommendations for achieving the main goal – saving the patient’s life [3,6]. In particular, it is important to promptly recognize specific laboratory and special research data characteristic of acute pancreatitis. A well-founded choice species surgical benefits, minimal invasive or "open", depending on the predominance of certain changes in the gallbladder, bile ducts, pancreas, parapancreatic and retroperitoneal space. The question of the effectiveness and at the same time the danger of endoscopic papillotomy awaits a final decision in conditions of complicated course. No less important is the determination of the timing of cholecystectomy, as well as the possibility of its implementation during a single hospitalization after the relief of acute pancreatitis of varying severity [2,5].
2. Objective of the Study
- To determine the choice of the method of surgical correction of acute biliary pancreatitis in order to eliminate pancreatic and biliary hypertension.
3. Material and Methods of the Study
- The article presents an analysis of the treatment of patients with acute biliary pancreatitis with moderate and severe course – 79 (30.3%) patients.Biliary pancreatitis was more common in women, with a ratio of 1:1.5 in favor of women. The age of patients varied widely from 18 to 90 years, the average age of patients was 52.5 ± 2.0 years.To assess the severity of the infectious process, signs of a systemic inflammatory response (SIRR) were identified. To establish signs and manifestations of multiple organ failure, the main indicators of laboratory and instrumental studies were used. Computer versions of calculation algorithms in the APACHE II scale were also used.Ultrasound allowed us to detect not only free fluid in the abdominal cavity and swelling of the pancreas, but also the phenomena of acute calculous cholecystitis and choledocholithiasis (Fig. 1).The most informative was magnetic resonance cholangiopancreatography for identifying the state of extrahepatic bile ducts, cholangioectasia, microlithiasis and sludge. gall bladder and bile ducts (Fig. 2).
 | Figure 1. Ultrasound, multiple gallbladder stones up to 0.5 cm with acoustic shadow, thickening of the gallbladder wall up to 0.6-0.7 cm |
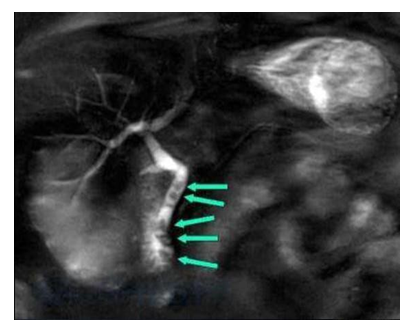 | Figure 2. MRI cholangiography. Choledocholithiasis |
 | Figure 3. Magnetic resonance cholangiopancreaticogram. Common bile duct and main pancreatic duct stones |
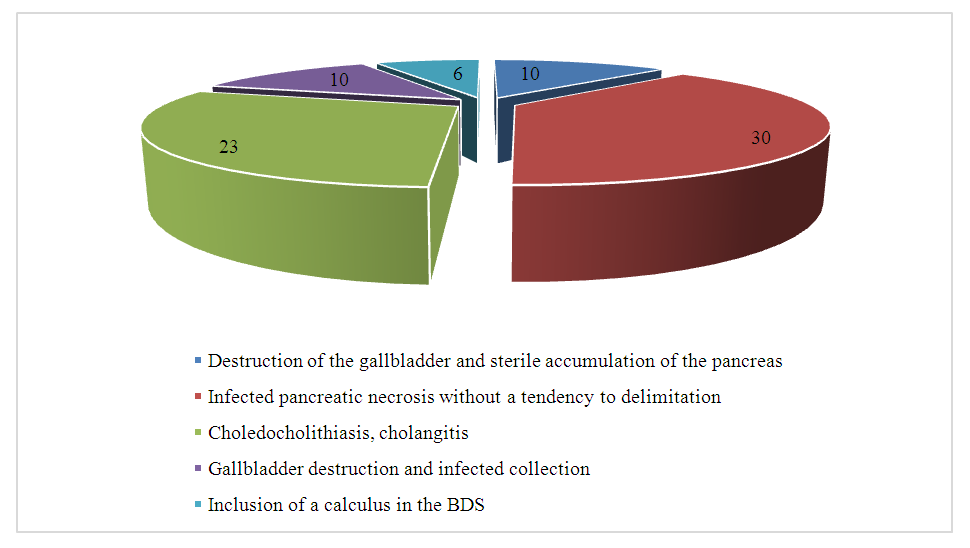 | Figure 4. Distribution of patients with moderate and severe acute biliary pancreatitis |
4. Results and Their Discussion
- Surgical treatment of acute biliary pancreatitis had its own characteristics associated with the need to correct cholelithiasis.6 patients with impaction of a stone in the major duodenal papilla, as our observations showed, required elimination of the pathological condition in the nearest time after detection. These patients underwent endoscopic papillotomy performed in the first hours after admission. It is the performance of endoscopic papillotomy in an emergency manner allowed to avoid the progression of acute pancreatitis, to stop it. And after the resolution of the edema of the pancreas, to perform laparoscopic cholecystectomy.23 patients with severe acute biliary pancreatitis, against the background of acute calculous cholecystitis, choledocholithiasis, mechanical jaundice and cholangitis, also underwent EPST. This manipulation was performed in the first 24 hours from the moment of admission.
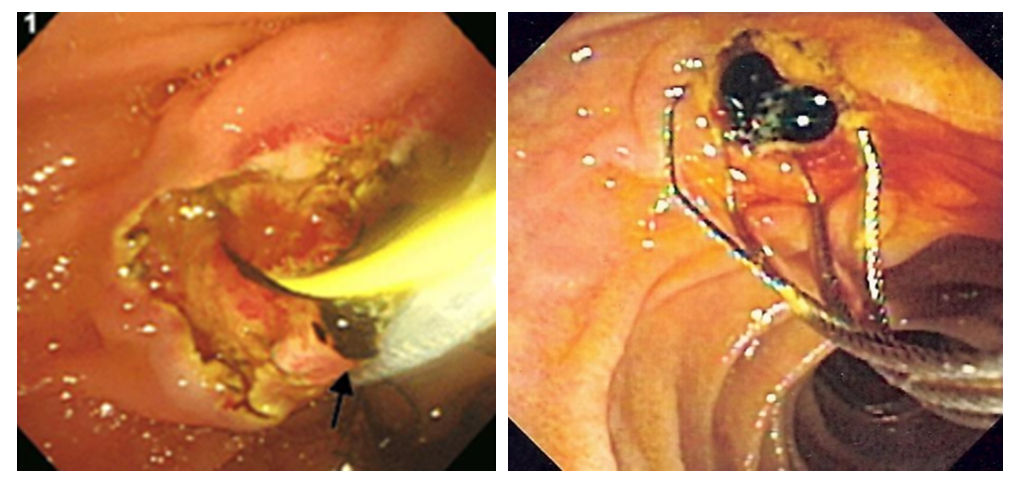 | Figure 5. Endoscopic papillotomy. Extraction of a common bile duct stone |
5. Conclusions
- 1. The leading criterion in choosing the optimal treatment tactics for acute biliary pancreatitis is the detection of stones in the biliary tract, the severity of the clinical course of the disease and the involvement of the retroperitoneal space in the inflammatory process. These criteria allow us to establish indications for EPST, lithoextraction, minimally invasive puncture methods for draining fluid accumulations or "open" operations.2. EPST effectively resolves obstruction of the bile and pancreatic ducts in acute biliary pancreatitis and eliminates ductal hypertension, which are the main cause of purulent cholangitis and pancreatic necrosis.3. Cholecystectomy, mainly laparoscopic, is advisable to perform after conservative resolution of mild biliary pancreatitis in the next 24 hours after the attack due to the risk of relapse of the disease. After performing EPST, cholecystectomy is also justified without discharge from the hospital if papillotomy is performed without complications. In acute biliary pancreatitis complicated by sterile or infected fluid accumulations, cholecystectomy should be postponed until their complete resolution and elimination of systemic inflammatory reactions.4. The proposed algorithm for examination and treatment of biliary pancreatitis, as well as substantiated indications for various types of surgical intervention, made it possible to individualize surgical tactics and avoid fatal outcomes in all cases except acute biliary pancreatitis complicated by unilateral or bilateral phlegmon of the retroperitoneal space.5. Long-term, over 4 weeks, course of acute biliary pancreatitis, late admission of the patient to a specialized department and ineffective surgical intervention lead to changes in the pancreas, parapancreatic and retroperitoneal spaces, similar to those in acute alcoholic pancreatitis, which was observed in 30 patients with a mortality rate of 23.3%. The most effective surgical intervention in these observations is the use of the "open" method. "belly".
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML