Rizayev Ezozbek Alimdjanovich , Kurbaniyazov Zafar Babajanovich , Abdurahmanov Diyor Shukurullaevich
Samarkand State Medical University, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The results of the survey are presented. 182 patients with moderate acute pancreatitis and severe clinical course of alimentary genesis. The main method of surgical treatment for aseptic necrosis of the pancreas is videolaparoscopic sanitation, percutaneous drainage under ultrasound guidance is effective for the treatment of pancreatic abscess or infected fluid accumulation. Minimally invasive surgeries were performed in 51.4% of patients with severe acute pancreatitis. Minimally invasive interventions are a priority in the treatment of patients with aseptic severe pancreatitis compared to open surgeries, which is justified by a significant decrease in the incidence of deaths (6.2% and 17.2%, respectively). In infected pancreatic necrosis, this figure was 19.1% and 27.3%, i.e. statistical differences are significant (p<0.05).
Keywords:
Acute pancreatitis, Severe clinical course, Minimally invasive interventions
Cite this paper: Rizayev Ezozbek Alimdjanovich , Kurbaniyazov Zafar Babajanovich , Abdurahmanov Diyor Shukurullaevich , Differentiated Approach to Minimally Invasive Treatment of Acute Pancreatitis of Alimentary Genesis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2962-2967. doi: 10.5923/j.ajmms.20241411.63.
1. Relevance
The solution to the problems of treating severe acute pancreatitis (SAP) is hampered by conflicting data on the use of various species operational interventions V different phases development of the disease. There are still disagreements regarding the choice of a specific method of surgical intervention; open and minimally invasive methods during aseptic enzymatic damage to the pancreas glands And development TOP [1,4].The late phase of the disease is complicated by the development of purulent-septic complications With frequency 30 - 50%, What along With high The mortality rate, which reaches 80%, also determines the relevance of the problem of developing rational tactics for surgical treatment of TOP [2,6].There is no decision on which surgical intervention methods are preferable for use in patients with purulent-septic complications of POP. One of the most important issues is the choice between open and minimally invasive methods. Each of these methods has its own advantages and limitations. Minimally invasive interventions are less traumatic compared to open surgeries, but the latter provide better sanitation of the site of purulent-septic inflammation [3,5].Thus, at present, urgent issues of rational choice of treatment methods in various phases of development of TOP remain unresolved, which necessitates this study.
2. Objective of the Study
To study the possibilities and develop indications for minimally invasive interventions depending on the stage of pancreatic necrosis in acute pancreatitis.
3. Material and Methods of the Study
The results of the survey are presented. 182 patients with moderate acute pancreatitis and severe clinical course of alimentary genesis, aged 31-81 years, were treated in the multidisciplinary clinic of the Samara State Medical University and the Samarkand branch of the Russian Scientific Center for Emergency Medicine in the period 2018-2023. The average age of patients was 51.6±13.7 years. The study included 78 women (42.9%) and 104 men (57.1%).The diagnosis of "severe acute pancreatitis" in 182 patients was made based on a combination of clinical and laboratory data, ultrasound examination (US), computed tomography (CT) of the abdominal organs (Fig. 1), and the results of diagnostic laparoscopy. To stratify patients, the TOP criteria were used in accordance with the revision of the Atlanta classification and the definition based on the international consensus (2012). To assess the volume of primary pancreatic necrosis using CT, the Balthazar-Ranso pancreatitis severity index was used. The SOFA scale was used to assess the severity of organ dysfunctions, and the APACHE II scale was used to assess the severity of the condition. | Figure 1. CT scan in axillary and frontal projections Pancreatic necrosis and fluid accumulations |
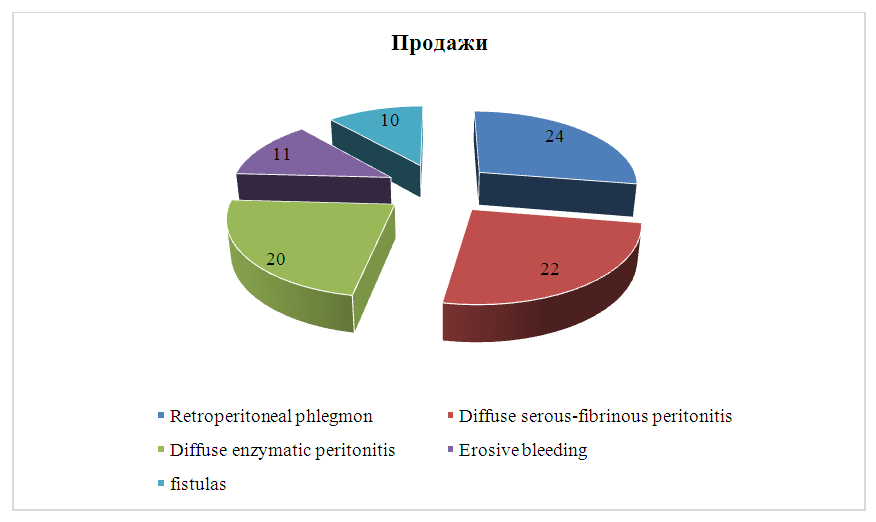
The majority of patients (65.9%) had small focal pancreatic necrosis. More expressed volumes defeats PJ V view Large focal and subtotal necrosis were observed in slightly more than a third of all cases (34.1%). In 89 (48.9%) patients, there was damage to one anatomical region. Damage to two or three anatomical regions of the retroperitoneal tissue was noted in 93 (51.1%) patients.Most patients had aseptic necrosis of the pancreas – 107 patients (58.8%).Infected severe acute pancreatitis occurred in 75 (41.2%) patients. The criteria for infection were a combination of clinical, instrumental, and laboratory signs: persistent hyperthermia, leukocytosis, the presence of gas bubbles during ultrasound examination and computed tomography, positive culture of discharge from abdominal drainage or aspirate obtained by percutaneous puncture.Patients with pancreatitis were divided into group A and group B according to the presence of aseptic or infected pancreatic necrosis according to the data of bacteriological studies of biomaterial to determine the type of microorganisms and their sensitivity to antibiotics. Group A - 107 (58.8%) patients with aseptic pancreatic necrosis was divided into subgroups: A1 - 40 (37.4%) patients who underwent only conservative treatment; A2 - 35 (32.7%) patients who underwent open surgical interventions as a surgical aid; A3 - 32 (29.9%) patients for whose treatment minimally invasive interventions were used. Group B - 75 (41.2%) patients with infected pancreatic necrosis was divided into subgroups: B1 - 42 (56%) patients who underwent minimally invasive interventions; B2 - 33 (44%) patients for whose surgical treatment open operations were used.Acute pancreatitis developed in 87 (47.8%) patients, in group A – 28 (26.1%) patients, in group B – 59 (78.6%) patients. Among the complications TOP in patients with aseptic necrosis of the pancreas (Group A) in 19 (17.7%) sick enzymatic peritonitis was detected in 9 (8.4%) patients serous-fibrous peritonitis. In patients with infected pancreatic necrosis (Group B), erosive bleeding was detected in 10 (13.3%) cases, and in 11 (14.6%) sick Education noted intestinal fistulas, at 24(32%) sick was phlegmon retroperitoneal space, 13 (17.3%) patients had serous-fibrous peritonitis. The structure of complications of TOP is shown in the figure 2.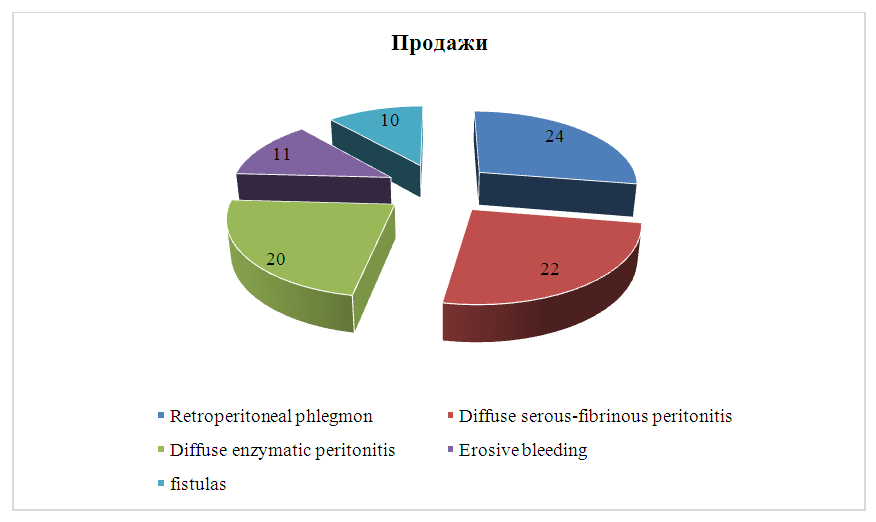 | Figure 2. Complications of TOP in patients with aseptic and infected pancreatic necrosis, n=87 |
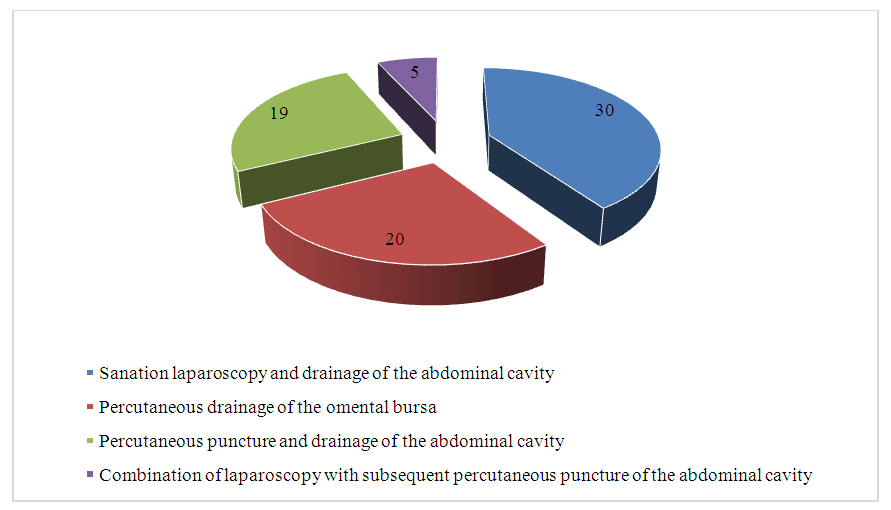
During the treatment of patients with TOP of alimentary genesis, various tactical methods were used. approaches that determine patient management: minimally invasive interventions and open surgeries.Among the surgical interventions used to treat 142 patients with TOP, 74 (40.1%) were minimally invasive interventions (Fig. 3) and 68 (37.4%) were open surgeries.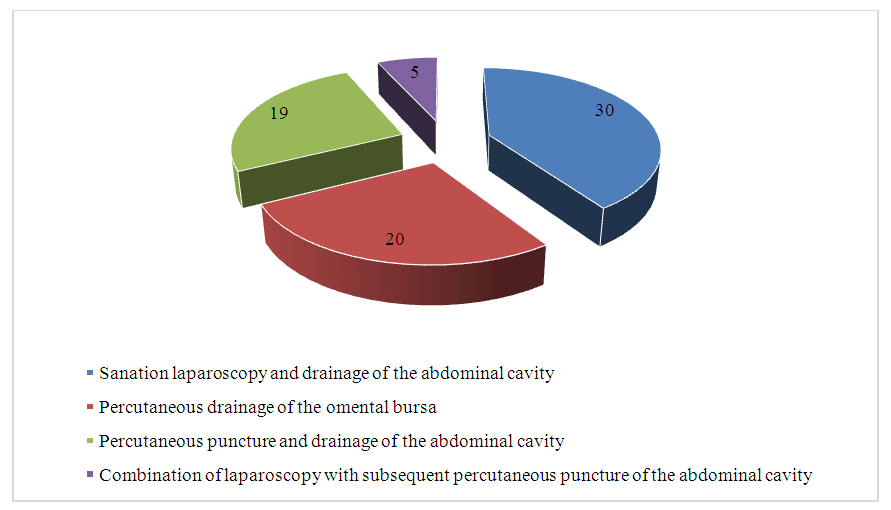 | Figure 3. Structure of minimally invasive interventions in patients with severe acute pancreatitis of alimentary genesis, n = 74 |
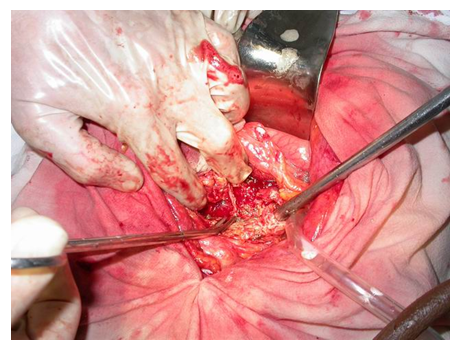
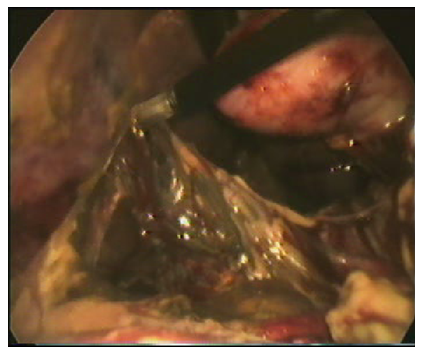
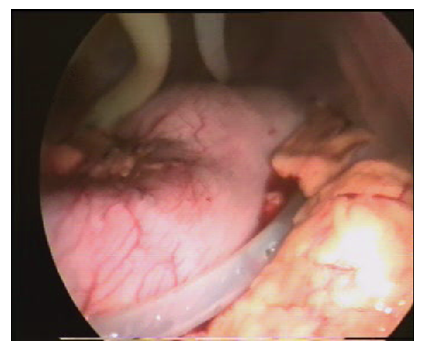
One of the main methods of surgical treatment of 30 (16.4%) patients with aseptic POP (group A) was videolaparoscopic sanitation and drainage of the abdominal cavity. In case of detection of extensive aseptic necrosis of the pancreas, as well as in the presence of large fluid accumulations located in the retroperitoneal space, with signs of bulging of the parietal peritoneum, it was opened through one or both lateral channels. In the presence of fluid accumulations in the omental bursa, it was drained through the gastrocolic bundle.In 3 cases, when fluid accumulations were detected in retroperitoneal fiber or stuffing box bag performed transcutaneous punctures with application ultrasonic navigation. 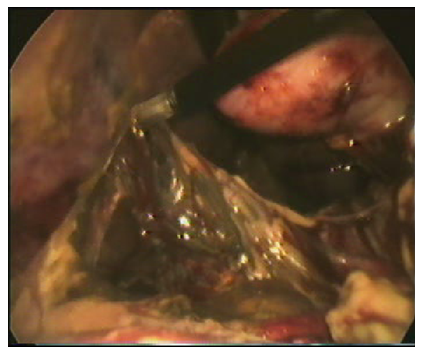 | Figure 4. Videolaparoscopy. Intersection of the gastroscopic ligament after clipping |
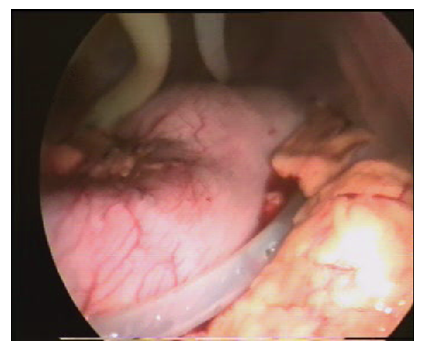 | Figure 5. Drainage of the omental bursa and retroduodenal space |
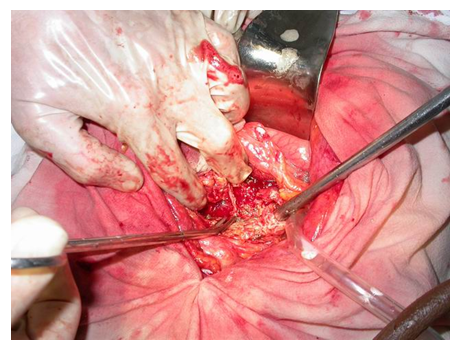
For the purpose of surgical treatment of 35 (19.2%) patients with aseptic necrosis of the pancreas, the following types of open surgical interventions were used:wide midline laparotomy and drainage of the abdominal cavity in 19 (10.4%) patients - in cases of parapancreatic infiltrate with signs of decompensated duodenal obstruction, as well as in case of rupture of a pseudocyst;minilaparotomy, sanitation and drainage of the abdominal cavity together with drainage of the omental bursa in 11 (11.5%) patients with enzymatic peritonitis (Fig. 6);abdominization of the pancreas after opening the omental bursa with subsequent drainage of the abdominal cavity and omental bursa in 12 (6.6%) patients - with rupture of a developing pseudocyst of the pancreas glands. In all cases applications open surgical interventions on against the background of the course of aseptic necrosis of the pancreas, suturing of the operating room was performed wounds (Fig. 7). | Figure 6. Minilaparotomy. Sanitation and drainage of the abdominal cavity |
 | Figure 7. Abdominization of the pancreas |
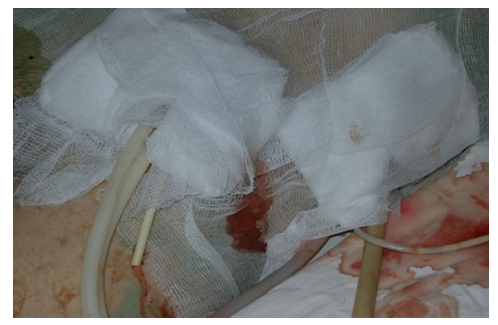
In infected pancreatic necrosis of the pancreas (group B), 42 (22.5%) patients underwent minimally invasive interventions - percutaneous drainage stuffing box bags under ultrasonic guidance for the treatment of pancreatic abscess or acute infected fluid collection. In order to control the effectiveness of percutaneous drainage of the omental bursa and abdominal cavity, as well as to identify residual cavities, ultrasound, CT and fistulography.For surgical treatment of purulent-septic forms of POP in 33 (18.7%) patients, open surgeries were used as the main surgical interventions (Fig. 8). In this case, the main surgical approaches were minilaparotomy, as well as lumbotomy and wide midline laparotomy.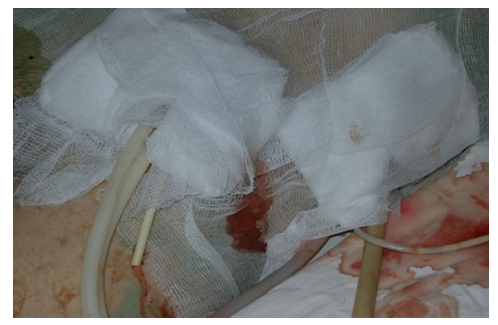 | Figure 8. Open drainage of the abdominal cavity with incomplete suturing of the wound with gauze tampons and double-lumen drainages |
When using wide midline laparotomy or lumbotomy two types of drainage were used: “open” (the operation ends with partial suturing of the wound, while gauze tampons are used for drainage, together with double-lumen drains with a diameter of 11 mm) – 20 (10.9%) patients or “closed” (complete wound suturing after installation of double-lumen drains in the area of the sanitized lesion, drainage of the retroperitoneal tissue and abdominal cavity under conditions of anatomical integrity of the omental bursa cavity and abdominal cavity) – 14 (7.7%) patients (Fig. 9). | Figure 9. Closed drainage with complete wound suturing after installation of double-lumen drains in the retroperitoneal tissue and abdominal cavity |
During repeated sanitization operations, tampons were changed, cavities were washed, necrosequestrectomy was performed, drainage position was monitored and adjusted, and drainage efficiency was assessed. In the presence of focal infection necrosis PJ on one sick had to 2 - 4 sanitation operations. In cases of development of widespread necrosis of the pancreas, the number of operations reached 4 - 7. Complete suturing wounds, That There is transition for the “closed” type of drainage, performed after the final achievement of necrosequestrectomy and the appearance of granulation in the wound.
4. Results and Their Discussion
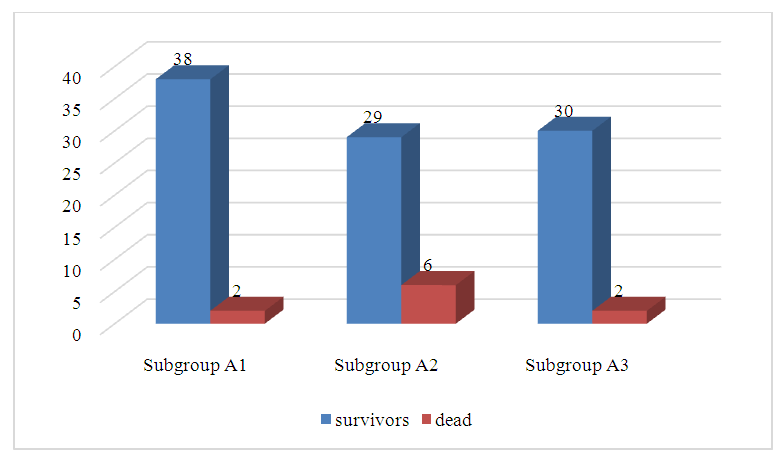
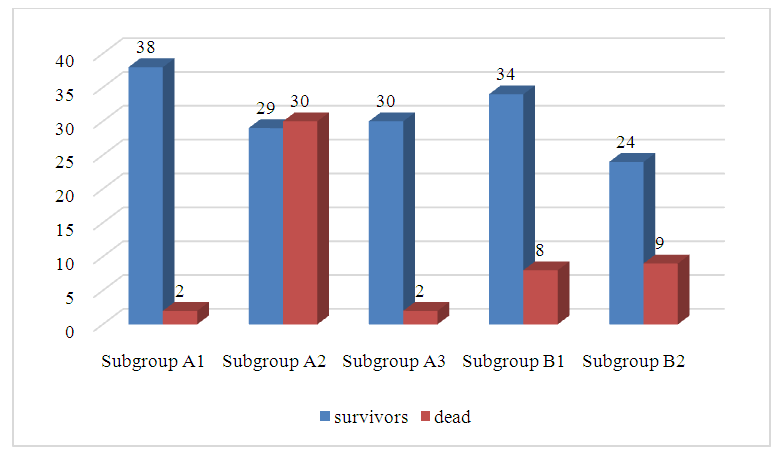
IN in the course conducting comparative analysis, directed on Comparison of mortality rates among patients in the studied subgroups revealed statistically significant differences. The mortality rate among patients in group A was 10 (9.3%). Figure 10 shows the ratio of surviving and deceased patients in subgroups.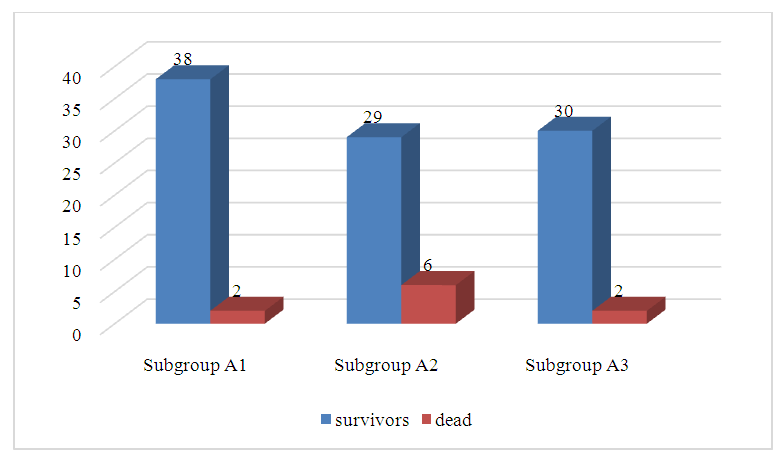 | Figure 10. Ratio of surviving and deceased patients in the studied subgroups |
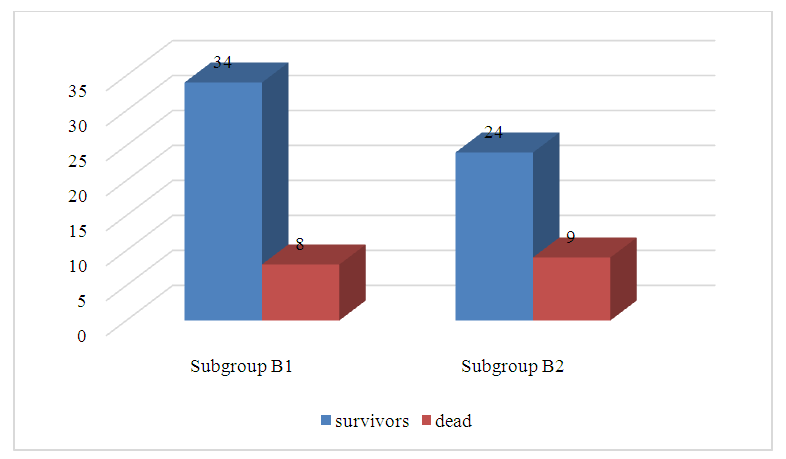
The highest proportion of deaths was observed in subgroup A2 (open interventions) due to the development of enzymatic peritonitis. At this indicator lethality V given subgroup 6 (17.2%) was statistically significantly higher than those in other studied subgroups. When comparing mortality in subgroups A1 (only conservative therapy) And A3 (minimally invasive interventions) Not was statistically revealed significant differences.When conducting a comparative analysis aimed at comparing mortality rates among patients in the studied subgroups, reliable differences were revealed. The mortality rate among patients in group B was 17 (22.7%). Figure 11 shows the ratio of surviving and deceased patients in subgroups B1 and B2.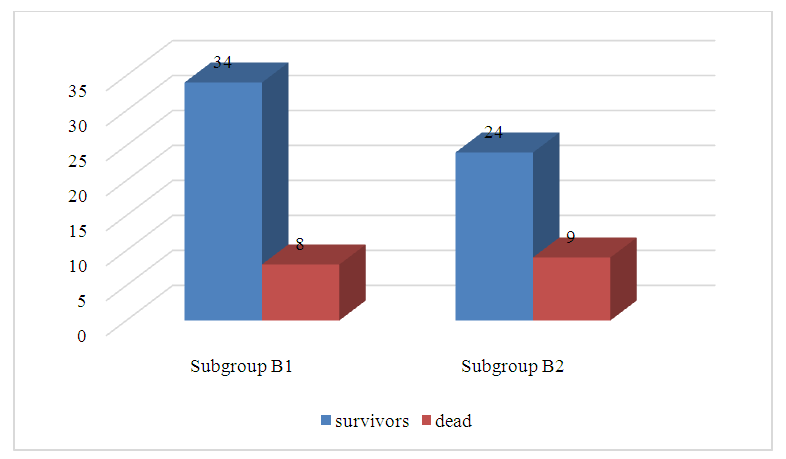 | Figure 11. Ratio of surviving and deceased patients in the studied subgroups |
The highest proportion of deaths was observed in subgroup B2 (open interventions) due to the development of complications of TOP such as erosive bleeding and retroperitoneal phlegmon. The mortality rate in this subgroup was 9 (27.3%). was statistically insignificantly higher than in subgroup B1-8 (19.1%) (minimally invasive interventions).A comparative analysis was conducted, aimed at comparing mortality rates among patients in groups A and B, and reliable differences were identified. Diagram 40 shows the ratio of surviving and deceased patients in groups A and B (Figure 12).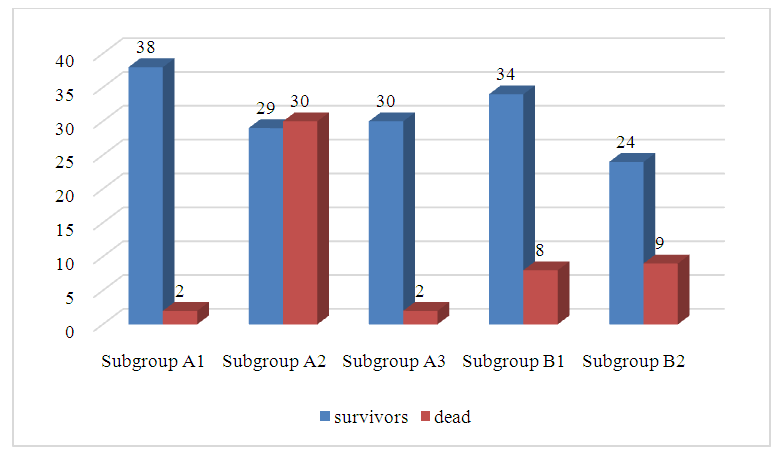 | Figure 12. Ratio of surviving and deceased patients in the studied subgroups |
When conducting a comparative analysis of mortality in subgroup A2 (open interventions) with aseptic necrosis of the pancreas 6 (17.2%) and in subgroup B2 (open interventions) with infected necrosis of the pancreas, statistically significant differences were revealed (p<0.05), in subgroup B2 - 9 (27.3%) statistically significantly higher than in subgroup A2 - 6 (17.2%). When conducting a comparative analysis in subgroup A3 (minimally invasive interventions) with aseptic necrosis of the pancreas and in subgroup B1 (minimally invasive interventions) statistically significant differences (p<0.05) were revealed in infected pancreatic necrosis, V subgroup B1 – 8 (19.1%) statistically significant higher how V subgroup A3 – 2 (6.2%).Thus, minimally invasive interventions are a priority in the treatment of patients with aseptic severe pancreatitis compared to open surgeries, which is justified by a significant reduction in the incidence of fatal outcomes (6.2% and 17.2%, respectively). In infected pancreatic necrosis, this figure was 19.1% and 27.3%.
5. Conclusions
1. The main method of surgical treatment for aseptic necrosis of the pancreas is videolaparoscopic sanitation, percutaneous drainage under ultrasound guidance is effective for the treatment of pancreatic abscess or infected fluid collection. Minimally invasive operations were performed in 51.4% of patients with severe acute pancreatitis.2. Minimally invasive interventions are a priority in the treatment of patients with aseptic severe pancreatitis compared to open surgeries, which is justified by a significant reduction in the frequency of fatal outcomes (6.2% and 17.2%, respectively). In infected pancreatic necrosis, this indicator was 19.1% and 27.3%, i.e. statistical differences are significant (p<0.05).
References
| [1] | Khadjibaev A.M., Rizaev K.S., Hashimov M.A., Baymuradov Sh.E. Acute biliary pancreatitis kak oslojnenie endobilarnyx vmeshatelstv. XXII Congress Assotsiatsii hepatopancreatobiliarnyx khirurgov. Tashkent 2015; 193-194. |
| [2] | Johnson L., Roberts C. "Minimally invasive techniques for managing biliary pancreatitis." Surgery Today. 2022; 52(4): 450-460. DOI: 10.1007/s00595-022-0240-4. |
| [3] | Lee D., Kim Y. "Role of endoscopic retrograde cholangiopancreatography in acute biliary pancreatitis." Endoscopy Journal. 2021; 33(3): 234-240. DOI: 10.1055/s-0041-1726042. |
| [4] | Miller R., Evans T. "Use of biomarkers in diagnosing acute biliary pancreatitis." Medical Journal of Research. 2020; 118(2): 190-198. DOI: 10.1097/MJR.0000000000000030. |
| [5] | Nguyen H., Watanabe Y. "Comprehensive treatment strategies for acute biliary pancreatitis." Clinical Gastroenterology. 2015; 49(3): 286-292. DOI: 10.1016/j.cgh.2015.01.015. |
| [6] | Smith J., Brown A. "Innovative surgical approaches in the treatment of acute biliary pancreatitis." Journal of Clinical Surgery. 2023; 45(1): 101-110. DOI: 10.1016/j.jocs.2023.01.001. |





 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML