-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2958-2961
doi:10.5923/j.ajmms.20241411.62
Received: Nov. 3, 2024; Accepted: Nov. 22, 2024; Published: Nov. 25, 2024

Pathomorphological Characteristics of Changes in the Lungs of Patients Who Died of Coronavirus Infection, Depending on the Time of Death
Sh. S. Burxanov1, A. I. Iskandarov1, A. X. Butaev2
1Republican Scientific and Practical Center of Judicial and Medical Expertise MZ RUz, Tashkent, Uzbekistan
2Republican Specialized Hospital "Zangiota - 1", Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In the study, researchers evaluated the pathomorphological changes in lung tissue in relation to the time of death of patients who died due to confirmed SARS-CoV-2 infection. The research subjects were divided into 3 groups, group 1 patients aged 0-14 days, group 2 patients aged 14-21 days and group 3 patients aged 21-40 days. The results of the study allowed us to draw the following conclusions: lung damage with the development of interstitial pneumonia is the main cause of severe disease and fatal outcomes. Inflammatory infiltration, generalized vascular damage with the development of thromboembolic complications, fibrosis of the lung parenchyma, and the addition of a secondary bacterial infection are predictors of an unfavorable prognosis. In the early stages, the main pathological changes in the lungs occur in the exudative phase, they reveal the appearance of thrombovasculitis, microangiopathy, and in the polyferative phase, the connective tissue cells around the walls of the bronchi and vessels grow. Based on this, it is possible to select specific treatment procedures for patients based on pathologoanatomical changes during the course of the disease and evaluate the quality of the treatment measures taken.
Keywords: Coronavirus infection, Interstitial pneumonia, Pneumosclerosis
Cite this paper: Sh. S. Burxanov, A. I. Iskandarov, A. X. Butaev, Pathomorphological Characteristics of Changes in the Lungs of Patients Who Died of Coronavirus Infection, Depending on the Time of Death, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2958-2961. doi: 10.5923/j.ajmms.20241411.62.
Article Outline
1. Introduction
- In 2019, it has been observed that SARS-CoV-2, a viral infection of the entire humanity, has risen to the level of a pandemic and caused lifelong disability as a result of high mortality rates and various complications. In the observations at the beginning of the pandemic, the course of the disease was manifested with different levels of clinical symptoms, depending on the age, gender, presence of secondary diseases and other factors. N.A. As a result of the analysis conducted by Belyakov, the high number of deaths caused by COVID-19 in the People's Republic of China was determined more in people over 60 years old and with co-morbidities. Also, in Italy and the Russian Federation, a high mortality rate was observed in the elderly, and it was found that the number of deaths in men was 1.5 more than in women [1]. Mild clinical symptoms of patients infected with coronavirus include dry cough, fever, weakness, flu, muscle pain, impaired sense of smell and sense of smell or the absence of the above symptoms at all, decreased appetite, and diarrhea in some categories of people. The course of COVID-19 in some patients has been observed to cause death due to severe clinical symptoms, including severe pneumonia with acute respiratory distress syndrome (ARDS), as well as damage to important parenchymatous organs and secondary infections with severe complications of MIKST infection [2]. In some patients, rapid transmission of coronavirus infection with the appearance of the first symptoms, the observation of interstitial pneumonia in the lungs, the area of damage in the lung tissue reached 85-90% in MSCT examinations, which is a syndrome of macrophage activation known by some authors as a result of local inflammatory reactions in patients (MAS) has been found to cause short-term death of patients with hypoxemia and other complications. In addition, among the causes of death of patients, changes in the rheological properties of blood in blood vessels and the formation of blood clots were at high levels [3,4]. When the pathogenesis of the disease was studied at the molecular level, it was found that the renin-angiotensin system actively participates in the acute phases of viral infection [5,6]. O.V. As a result of the observations made by Zayratyants and a number of authors, almost all patients who died from severe complications of COVID-19 had damage to the respiratory organs, including the lung tissue, and the harmful effects of the virus on other organs were found to be low [7]. Despite the conducted research, the pathogenesis and morphological features of the lung tissue of COVID-19 have not been sufficiently studied, which, in turn, can serve as an effective solution for the development of treatment and preventive measures of the disease.
2. Materials
- To evaluate pathomorphological changes in lung tissue depending on the time of death of patients who died as a result of SARS-CoV-2 infection confirmed on the basis of PTsR data and clinical instrumental examinations.
3. Research and methods
- Medical histories of 42 patients with positive PTsR results who died of coronavirus infection in the specialized multidisciplinary hospital "Zangi ota-2" located in Zangi ota district between 2020 and 2022 were randomly selected, and the period of illness and cause of death were analyzed. attention was paid to the data, macroscopic and microscopic analyzes of the results of pathologoanatomical examination were studied. Examination of the bodies of persons who died from COVID-19 was carried out using generally accepted methods in accordance with the guidelines of the World Health Organization (2020) in accordance with the requirements of sanitary and epidemiology, after the pieces of internal organs were fixed in a 12% formalin solution and processed by histological methods Preparations stained with hematoxylin-eosin, Mallory and Van Gieson dyes. digital photos of the lung tissue being studied using the ZEISS Axiocam 105 color camera under the AxioScope microscope. Up to 4-5 photos were taken by selecting the changed areas at x10 and x40 of the microscope lens. Clinical and pathomorphological results were applied using Microsoft Excel and Statistica 6.0 programs. When determining the difference by gender, the Wilcoxon-Manna-Whitney criterion, the correlation between the age of the patients and the studied parameters was determined by the Spearman's rank correlation coefficient. From the Kruskal-Wallis test for the determination of the difference between several samples, the distribution of main trends and quantitative characteristics was characterized by the mean M and standard error m, as well as the median and interquartile range depending on the type of distribution painted using methods.
4. Results and Discussion
- The medical history and histological conclusions of pathanatomical examination of patients (n-42) with positive PTsR analysis who died due to the diagnosis of bilateral polysegmental pneumonia were analyzed. In the analysis of deceased patients by gender, men made up 61.9% (n-26), women 38.09% (n-16), patients aged 30-40 made up 21.42% of all patients, aged 40-60 30.95%, 60 patients older than 47.61% of the total number of patients (represented in diagram No. 1).
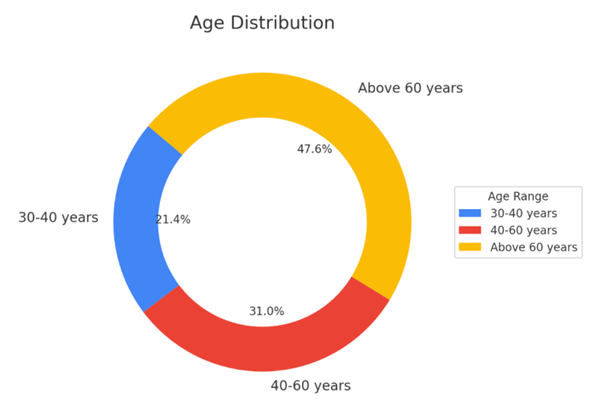 | Diagram 1. Indicators by age of patients with a positive PTsR analysis who died of a diagnosis of bilateral polysegmental pneumonia (n-42) |
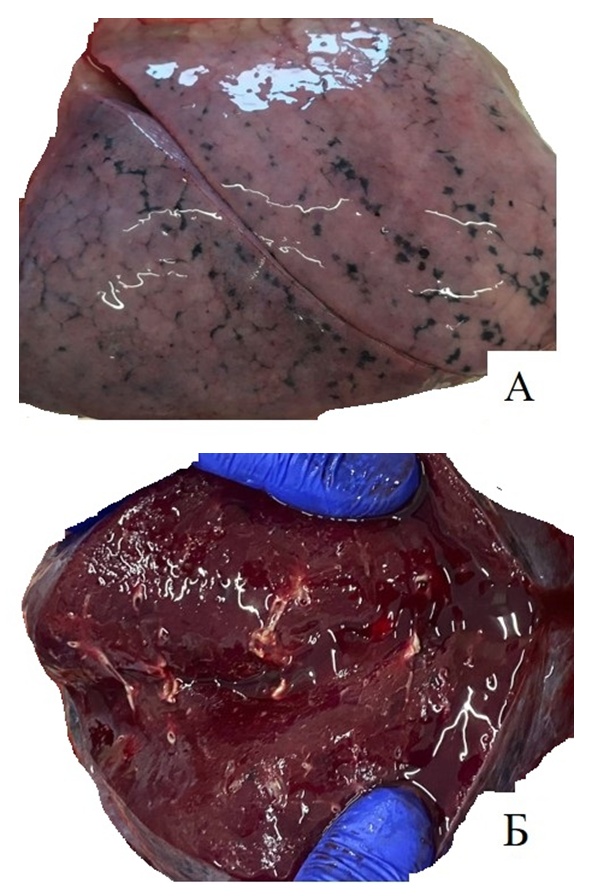 | Figures 1A and B. macroscopic view of lung tissue from patients who died between 0-14 days |
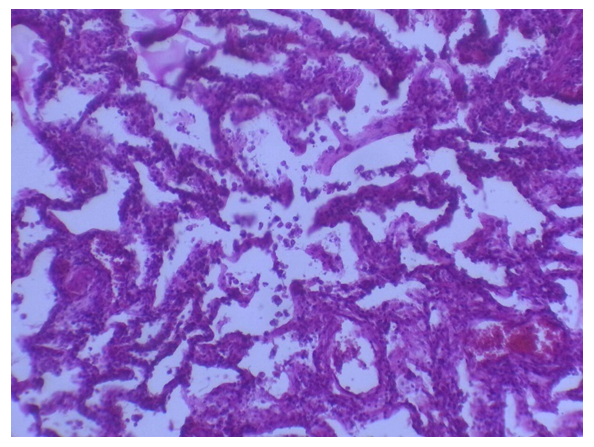 | Figures 2. Signs of fullness and acute exudative inflammation in the microcirculatory trunk and small branch arteries in the lung tissue. Illness 2 weeks apart. G-E. 10×0.25 |
 | Figures 3A. Dark red color, coarsening of pleural sheets, strong expression of venous congestion in blood vessels, and white and red infarct foci of various sizes. In 14-21 days, the patient's lungs |
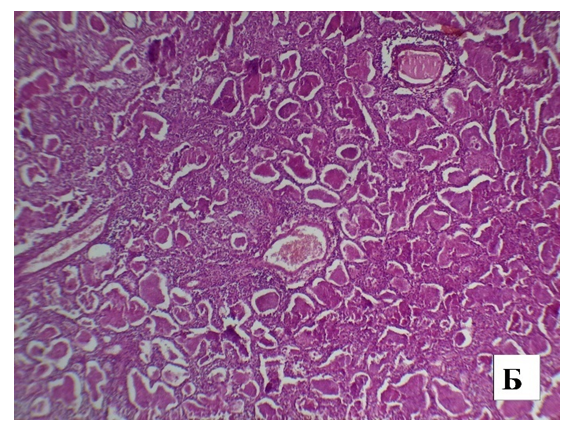 | Figures 3B. Formation of mixed-type thrombi, hyperplastic alveolocytes in the cavity of blood vessels in small and medium-sized hummingbirds. G-E. 10×0.25 |
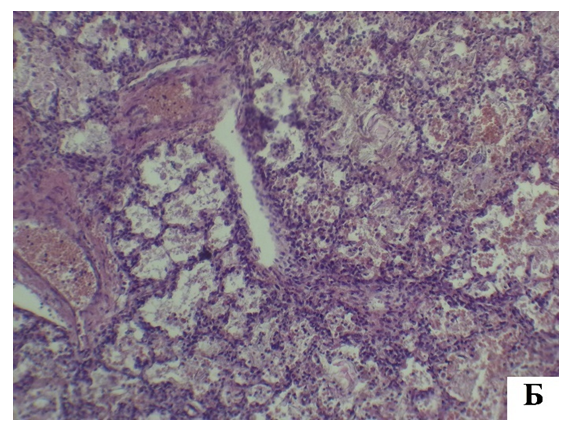 | Figures 4B. Alveolar edema and microangiopathies, venous congestion, thrombi in the vascular space, formation of fibrinoid masses in the cavity and wall of the alveoli. G-E. 10×0.25 |
5. Conclusions
- Acute respiratory distress syndrome in SOVID-19 interstitial pneumonia differs from the classic pattern of diffuse alveolar injury, modified in 2016 [8].Porazhenie legkix s razvitiem COVID-19-interstitsialnoy pneumonii — the main cause of tyajelogo techenia zabolevaniya i letalnykh iskhodov. Expressed inflammatory infiltration of the lung tissue by inflammatory macrophages, generalized defeat of the microcirculatory bed and larger large vessels with the development of thromboembolic complications, progressive parenchymal lung fibrosis, secondary bacterial infection is a predictor of unfavorable prognosis.With the development of COVID-19, lung damage - interstitial pneumonia - is the main cause of severe illness and death. Clear inflammatory infiltration of lung tissue by inflammatory macrophages, damage to the microcirculatory tract and larger common blood vessels with the development of thromboembolic complications, progressive fibrosis of the lung parenchyma, transition to secondary bacterial infection predicts unpleasant consequences [9].In the early stages, the main pathological changes in the lungs occur in the exudative phase, i.e., diffuse viral-toxic damage to the alveoli, thrombovasculitis of blood vessels, microangiopathy, and in the proliferative phase, connective tissue cells around the walls of the bronchi and vessels grow, which manifests proliferative inflammation. Based on this, it is possible to select specific treatment procedures for patients based on pathologoanatomical changes during the course of the disease and assess the quality of the treatment measures.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML