-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2948-2950
doi:10.5923/j.ajmms.20241411.59
Received: Nov. 3, 2024; Accepted: Nov. 22, 2024; Published: Nov. 25, 2024

Immunological Effectiveness of Intrauterine Intravascular Hemotransfusion to the Fetus During Rh Immunization of Pregnant Women
Kh. M. Khatamov, U. U. Jabborov, N. A. Urinbaeva
Republican Perinatal Center of the Ministry of Health of the Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

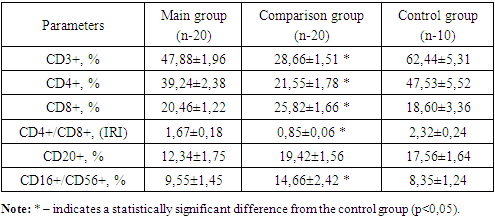
Purpose of the study: to study the indicators of cellular immunity in newborns with hemolytic disease who underwent high-tech fetal operations during pregnancy. Materials and methods: studies were carried out in the Republican Perinatal Center for 2024. A total of 50 newborns participated in the studies and were divided into 3 groups. 1st main group of 20 newborns with hemolytic disease and who underwent an operation “intrauterine, intravascular blood transfusion to the fetus” in the antenatal period. The 2nd comparison group consisted of 20 newborns with hemolytic disease and who did not undergo fetal surgery in the antenatal period and the 3rd control group of 10 healthy newborns. All immunological studies were carried out at the Institute of Immunology of the Academy of Sciences of the Republic of Uzbekistan. Results: the number of CD3+ T-lymphocytes and CD4+ T-helper cells in newborns in the comparison group were significantly reduced by 2.2 times compared to the control group, and the number of CD8+ cytotoxic lymphocytes and CD16+ killer lymphocytes was significantly increased by 1.4 times and 1 .8 times in relation to newborns of the control group. The indicators of CD20+ B-lymphocytes in both groups of newborns did not differ significantly from those in the healthy group. Conclusion: intrauterine, intravascular blood transfusion to the fetus not only improves hematological blood parameters, but also improves indicators of cellular immunity, in particular an increase in the number of T-lymphocytes, which has a beneficial effect on T-cell immunity and prevents the formation of an immunodeficiency state at birth.
Keywords: Rh-immunization, Hemolytic disease of the newborn (HDN), T-lymphocytes CD3+, CD4+, CD8+, CD16+, CD20+ immunoregulatory index (IRI), B-lymphocytes, Intrauterine intravascular blood transfusion
Cite this paper: Kh. M. Khatamov, U. U. Jabborov, N. A. Urinbaeva, Immunological Effectiveness of Intrauterine Intravascular Hemotransfusion to the Fetus During Rh Immunization of Pregnant Women, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2948-2950. doi: 10.5923/j.ajmms.20241411.59.
Article Outline
1. Introduction
- Maternal alloimmunization, also known as hemolytic disease of the newborn (HDN) occurs when a mother is exposed to fetal antigens and subsequently produces immunoglobulin G antibodies targeting fetal red blood cell antigens that cross the placenta [1]. In cases of diagnosed fetal anemia, intrauterine transfusion may be necessary to restore fetal red blood cell levels [2]. Treatment for hemolytic disease of the newborn includes phototherapy, blood transfusion, and when indicated, exchange transfusion [3]. According to data from local authors in Uzbekistan from 2016-1018, there was a trend toward an increased incidence of hemolytic disease (HD) in newborns, both in percentage and absolute number [4]. Phototherapy is the primary treatment for unconjugated hyperbilirubinemia in infants [5]. A Cochrane review (2012) found that early phototherapy in preterm infants can prevent bilirubin from reaching levels requiring exchange transfusion and reduce the risk of neurological damage [6]. High bilirubin levels are toxic to the basal ganglia and brainstem, potentially causing bilirubin encephalopathy with various clinical consequences [7]. The effectiveness of phototherapy depends on the light wavelength, source intensity, total radiation dose (based on phototherapy duration and exposed skin area), and the initial bilirubin level, all with minimal serious side effects [8]. Currently, LED lamps are preferred over fluorescent lamps due to reduced risk of overheating in newborns [9]. Some studies by Russian authors have examined adaptive cellular immunity in newborns with hemolytic disease who received antenatal intrauterine transfusions [10]. Based on our findings, we have decided to conduct a more detailed study of the key indicators of innate cellular immunity in newborns with hemolytic disease.Purpose of the study: the objective of this study was to evaluate cellular immunity factors, including the levels of CD3+ T-lymphocytes, CD4+ T-helper cells, CD8+ T-suppressor cells, CD16+ T-killer cells, CD20+ B-lymphocytes, and the immunoregulatory index in umbilical cord blood from newborns diagnosed with hemolytic disease due to Rh incompatibility. This assessment specifically targeted infants whose mothers received treatment through intrauterine intravascular blood transfusion during the antenatal period.
2. Research Materials
- This study involved a total 50 newborns delivered at the Republic Perinatal Center in 2024. The participants were categorized into three groups. The first main group comprised 20 newborns diagnosed with hemolytic disease who underwent intrauterine intravascular blood transfusion during the antenatal period. The second comparison group also included 20 newborns with hemolytic disease, but these infants did not receive any fetal interventions during the antenatal period. The third control group consisted of 10 healthy newborns.
3. Immunological Research Methods
- Studies of the immune status of newborn in umbilical cord blood were conducted on the first day of life in the laboratory of Fundamental immunology of the Institute of Immunology and Human Genomics of the Academy of science of Uzbekistan. Cellular immunity parameters, including CD3+, CD4+, CD8+, CD20+, CD16+/56+ cell counts, were measured from BD (USA) through flow cytometry (BD Accuri C6). The immunoregulatory index (IRI), which is the ratio of the number of CD4+ T-helper cells to the CD8+ T-lymphocytes, was calculated manually. In the healthy children and adults, the IRI typically exceeds one.
4. Statistical Analysis
- Statistical processing of the result involved both parametric and non-parametric analysis methods. Data accumulation, adjustment, systematization, and visualization were performed in Microsoft Office Excel 2018. Further statistical analysis was conducted using IBM SPSS Statistics v.26 (IBM Corporation). Further comparisons of means in normally distributed quantitative data sets, Student’s t-test was applied. The resulting t-test values were assessed against critical values, with differences considered statistically significant at a significance level of p< 0.05.
5. Results and Discussion
- This study aimed to conduct an immunological assessment to evaluate effectiveness of intrauterine fetal intravascular blood transfusion by analyzing cellular immunity in newborns who underwent this procedure. Immunological examinations of cellular markers were performed on umbilical cord blood from newborns with hemolytic disease of the newborn (HDN) who received intrauterine blood transfusions and those who did not. The results of these analyses are summarized in table 1.
|
6. Conclusions
- 1. In newborns from the comparison group, who did not undergo fetal interventions, the number of CD3+ T-lymphocytes and CD4+ T-helper cells were reduced by 2.2 times compared to the control group. The immunoregulatory index (IRI) was also lower in the comparison group, showing a 2,7-fold decrease, while no notable changes were observed in the main group. 2. The number of CD8+ cytotoxic lymphocytes and CD16+ killer lymphocytes was increased by 1.4 times and 1.8 times, respectively, in the comparison group compared to the control group. 3. The levels of CD20+ B-lymphocytes in both the main and comparison groups showed no appreciable differences compared to the healthy control group. 4. Intrauterine intravascular blood transfusion not only improves fetal hematological parameters but also positively affects cellular immunity. Specifically, it boosts the number of T-lymphocytes, which enhances T-cell immunity and helps prevent the onset of immunodeficiency at birth.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML