Islomov N. K.1, Mustafakulov E. B.1, Julbekov K. I.2
1Samarkand State Medical University, Samarkand, Uzbekistan
2Samarkand Branch of the Republican Scientific Center of Emergency Medical Care, Samarkand, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Nowadays laparoscopic surgical interventions have firmly entered the daily practice of most medical institutions. On the basis of complex randomized studies conducted in many countries of the world, the main advantages of laparoscopic surgeries in relation to open methods of similar interventions have been formulated, namely the lower degree of pain sensations after the operation, reduction of anesthetic agents consumption, shorter period of hospital stay after the operation, quick return to the usual life and work, good cosmetic effect, low frequency of postoperative hernia development.
Keywords:
Extraction methods, Laparascopy, Appendectomy, Ectopic pregnancy
Cite this paper: Islomov N. K., Mustafakulov E. B., Julbekov K. I., Review of Different Methods of Macro Specimen Extraction During Laparoscopy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2940-2943. doi: 10.5923/j.ajmms.20241411.57.
1. Introduction
Laparoscopy, often referred to as minimally invasive surgery, has revolutionized the field of surgical procedures by allowing surgeons to perform operations through small incisions, using a camera and specialized instruments [5]. This technique has become increasingly popular due to its benefits, such as reduced postoperative pain, shorter recovery times, and minimal scarring compared to traditional open surgery [1].A critical aspect of laparoscopic surgeries is the extraction of macroscopic specimens, such as tumors, diseased organs, or tissue samples, which need to be removed for further examination or treatment. The extraction process presents unique challenges due to the limited size of the incisions and the need to ensure the integrity and sterility of the specimen [2].There are various methods employed to facilitate the effective and safe extraction of specimens during laparoscopy. These methods vary based on the type and size of the specimen, the specific surgical procedure, and the equipment available [6]. Techniques can range from the use of retrieval bags to morcellation and the enlargement of incision sites for direct retrieval. Each method has its advantages and limitations, requiring surgeons to choose the most appropriate approach based on the clinical situation [3].In summary, understanding the range of methods available for specimen extraction in laparoscopic surgery is crucial for optimizing surgical outcomes and ensuring patient safety [4].
2. Materials and Methods
Since laparoscopy nowadays covers a wide range of operations such as removal of large tumors (myomas, large ovarian tumors), appendectomy, ectopic pregnancy, splenectomy, colon resection and some others, the most important is to reduce the volume of the tumor or tissue and remove it from the peritoneal cavity through an incision with the smallest possible size. In the early days of laparoscopy, myomectomy was rarely performed, but now, over the years, as suturing techniques and skills have improved, laparoscopic myomectomy has become increasingly popular. Currently, the size and number of myomas to be removed are not contraindications to laparoscopic surgery, the contraindication to laparoscopic removal of myomas currently depends more on the experience of the surgeon.
3. Results
At the present moment there are a number of methods of tissue removal from the abdominal cavity during laparoscopy available. The choice of the method of extraction depends on the organ to be removed, its size, tumor type, surgeon's preferences, availability of instruments, and cost-effectiveness. In this article, we will describe all methods of tissue extraction during laparoscopy. Trocars of 10 mm size are used in almost all laparoscopic surgeries. These same trocars can be used to remove tissues like cyst capsules, fallopian tubes, fetus in ectopic pregnancy, appendix etc. Using an instrument with a diameter of 5 mm through a 10/5 mm adapter with a 10 mm trocar allows easy and quick removal of tissues. If there is a mismatch between the size of the tissue to be removed and the trocar, it is possible to reduce the size of the tissue by using spiral incisions along the length of the tissue, which facilitates tissue extraction through a 10 mm diameter laparoport.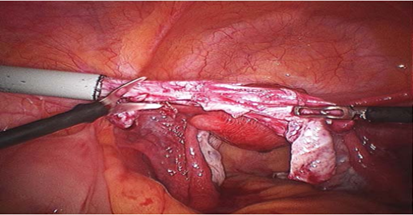 | Figure 1. Spiral incision of the cyst capsule to reduce its size |
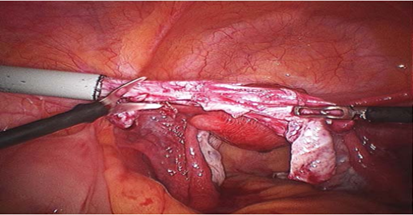
In cases when the diameter of all trocars during the operation is 5 mm, it is possible to replace a 5 mm trocar with a trocar with a diameter of 10 mm to widen the port. Sometimes when it is impossible to extract tissue even through a 10 mm trocar (e.g., empyema of the appendix, gallbladder), it is possible to use a 10/20 mm portorrhodilator. In lower abdominal surgeries, a laparoport in the lower left quadrant of the abdomen is usually used for extraction because it is usually not visible because it is located in the bikini area; in cases of cholecystectomy, a laparoport under the mesoid process is usually used because of the lower risk of postoperative hernia development.  | Figure 2. Extraction of the worm through a 10 mm trocar in the left iliac region using sterile gloves as an endobag |
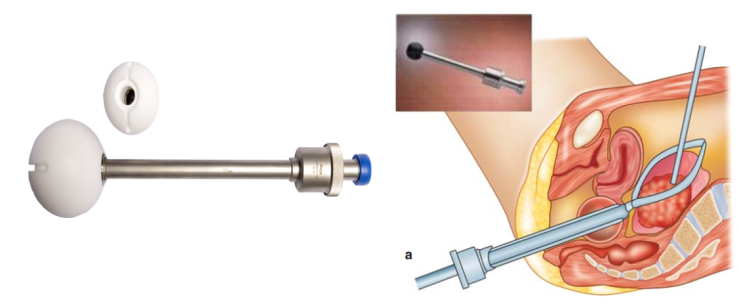
Colpotomy.It is a fairly simple and effective technique for macropreparation extraction. This technique is used mainly for the extraction of myomas and ovarian neoplasms, the macro preparation is placed in the endobag. The essence of this method is that the Douglas space is used to extract the macro preparation. The progress of laparoscopic surgery was hindered by the difficulties arising during tissue extraction in cases of mismatch of their sizes with the sizes of traditional trocars. The problem was that transabdominal tissue removal required a large incision, which negated all the advantages of laparoscopy, while transvaginal removal resulted in CO2 leakage. These technical difficulties were overcome with the introduction of the CCL (Colpo-Coeliochirurgie Lausanne) vaginal extractor (Figure 3), which consists of a trocar fitted with a sphere-shaped head at one end. The round surface of the sphere fits well against the posterior vaginal vault and has a horizontal groove on the surface, which serves as a guide at the time of peritoneal incision.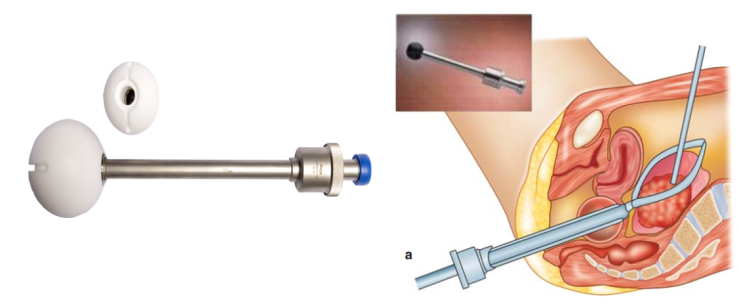 | Figure 3. Vaginal CCL extractor |
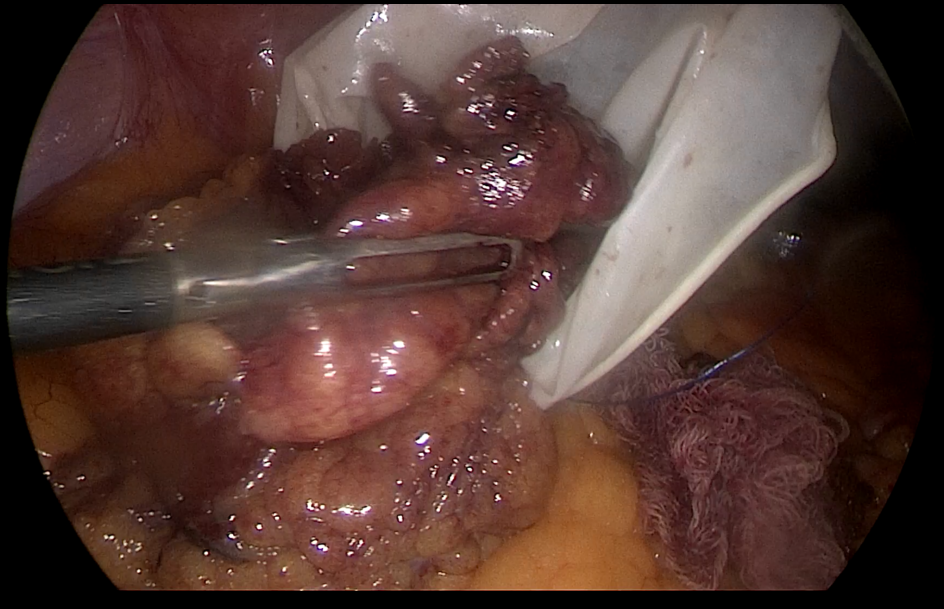
A vaginal extractor or forceps with a sponge at the end are inserted intravaginally in order to prevent gas leakage and to determine the location of the colpotomy. Using a monopolar hook, scissors or a laparoscopic scapula, an incision is made above the CCL extractor, between two uterosacral ligaments (Figure 3). After an incision in the posterior arch of the vagina, 10-millimeter forceps are driven, a macro-preparation or endobag is seized and removed. After that, the incision can be sewn vaginally or laparoscopically. The procedure is safe because it takes place under endoscopic visual control. The above method is mainly used for the extraction of ovaries, organic cysts, fetal ectopic pregnancy, fibroids.The application of endobag.Endobag is widely used in operations such as laparoscopic ovariectomy and cystectomy to prevent the spillage of the contents of macropreparations. There is evidence that the use of endobag bags reduces the operation time. The outpouring of the incurable macropreparations into the abdominal cavity usually occurs either during surgery or at the time of its removal from the abdominal cavity. In cases with ovarian cysts, it is recommended not to pierce and aspirate the contents of the cyst to prevent the dissemination of malignant cells. In such cases, the ideal solution is to use Endobag.Endobag are commercially available, can be injected into the abdominal cavity through a laparoport in the lower left quadrant of the abdomen, a laparoport in the umbilical region, as well as endobag can be injected through a vaginal CCL extractor. After insertion into the abdominal cavity, the endobag unfolds. A cyst, a worm-like process, or another facet to be removed is placed inside the package. The contents of the cyst, gallbladder can be sucked out to reduce the volume of tissue to be removed, but manipulation should be carried out inside the Endobag bag. This method, when properly performed, prevents the contents of the macropreparation from pouring into the abdominal cavity. After that, the thread is tightened to close the lumen of the bag. The macropreparation can be removed through the laparoport sites on the anterior abdominal wall or using a vaginal CCL extractor transvaginally, depending on the operation performed and the surgeon's preferences (Figure 4.).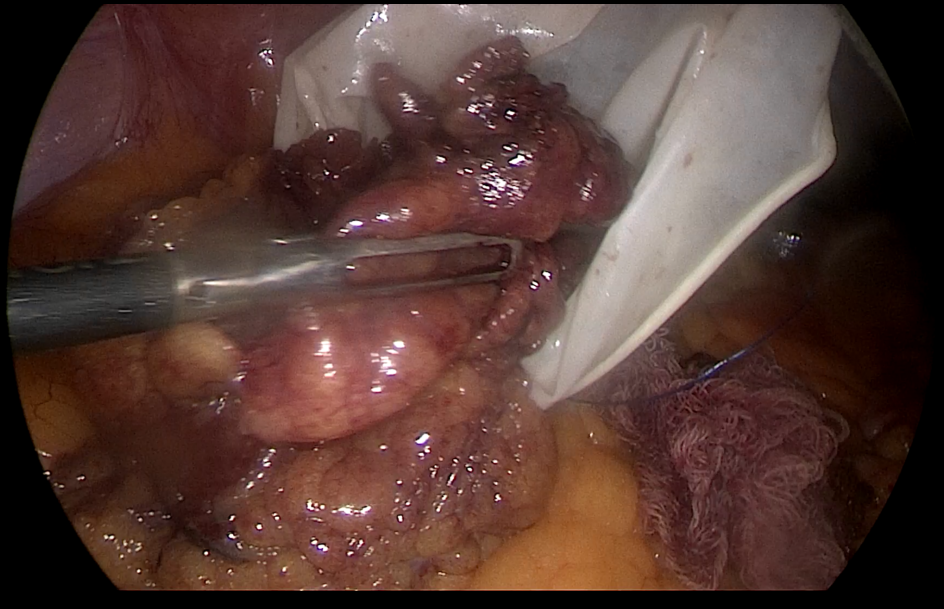 | Figure 4. The macropreparation is placed in a homemade bag |
In developing countries, homemade evacuation systems made of sterile gloves, condoms, and plastic bags are used instead of endobag. Another modification of the homemade endobag is a sterile glove with a pouch seam at the entrance and bandaged at the base of the fingers.After placing the cyst, gallbladder in the bag, the pouch is tightened. An option is possible with suction of the contents of the macropreparation to reduce its size, the suction procedure is strictly performed inside the pouch to prevent the outpouring of the contents of the macropreparation. The extraction of the sac can be performed by traction by a thread either transvaginally or through laparoports on the anterior abdominal wall. This method is cost-effective in the absence of Endobag systems for free sale.Cases of using sterile condoms as Endobag are described. Their use is justified in cases where Endobag is not available for free sale. The advantage of tissue extraction with a condom is the lubricant applied to the surface of the condom, which facilitates the process of slipping it through the tissues of the anterior abdominal wall during traction.Electromechanical morcellation.Laparoscopic operations for the removal of large formations such as fibroids or uterus are still a problem of minimally invasive surgery. Despite the fact that at the moment there are many methods of tissue extraction specifically designed for the removal of large macro-preparations, all of them have disadvantages in the form of the fact that the procedure takes a long time, often requires an expansion of the incision or even sometimes an additional incision is required, as for example in the case of transvainal removal of drugs. In 1973, the world's first manual morcellator was developed for crushing and removing samples during laparoscopic operations. Despite this, even removing small samples required considerable time, since the tool worked due to manual effort. In 1993, the Steiner morcellator revolutionized laparoscopic surgery. Unlike a manual morcellator, the electromechanical tool made it possible to remove even large macropreparations in a matter of minutes without additional incisions.The electromechanical morcellator consists of a cutting tube powered by an engine, which can be inserted into the abdominal cavity through an installed trocar. The rotation speed can be pre-selected, the instrument is activated by the pedal. There is a possibility of clockwise, counterclockwise rotation, rotation by oscillatory movements. A toothy clamp is inserted into the abdominal cavity through a cutting tube. After the macropreparation is captured by the forceps, the forceps are pulled back to the cutting edge of the rotating morcellator. The fabrics are cut in the shape of a cylinder. Thus, even a large macropreparation can be removed within a few minutes without additional incisions. The use of a morcellator also ensures the preservation of tissue for subsequent histological examination.The Rotocut tool from Karl Storz was proposed to remove macro-preparations of larger formations. In addition to the usual 12 mm port, 15 mm ports are offered for larger macro products. The device is powered by a heavy-duty electric motor. The blade is protected by a safety mechanism that prevents any unintended cutting of the fabric. The new Rotocut has many additional safety features and higher speed compared to its predecessors.An important economic aspect is the possibility of reusable use. Therefore, this reusable device is preferred over its disposable counterparts. However, it should be borne in mind that despite the one-time use, the Gynecare morcelling tool is also in great demand.After modeling, an important stage of the operation is the closure of the abdominal cavity defect to prevent the development of Richter's infringement, since this extraction method uses laparoports with a diameter of 12-15 mm. A special needle is used to close the defect from the laparoport. After removing the morcellator, the needle is inserted into the abdominal cavity through one edge of the wound, while the needle is inserted into the abdominal cavity along with a vicryl thread. In the abdominal cavity, the thread is removed from the needle and the needle is removed. The needle is re-inserted through the opposite edge of the wound, but without a thread. In the abdominal cavity, the free end of the vicryl thread is put on the needle, and it is removed from the abdominal cavity together with the needle. After suturing, the defect of the peritoneum closes properly, thereby eliminating the risk of internal organs coming out.
4. Conclusions
In conclusion, the review of different methods for macro specimen extraction during laparoscopy highlights the diversity and complexity of this integral surgical process. Each extraction technique comes with its unique set of advantages and disadvantages. For instance, the use of retrieval bags is beneficial for containing specimens and minimizing contamination risk, whereas morcellation allows for the removal of large specimens through small incisions but can pose challenges related to tissue dissemination.Choosing the appropriate extraction method requires a careful assessment of several factors, including the size and type of the specimen, the patient's condition, and the surgeon’s experience and proficiency with the available techniques. Moreover, considerations around minimizing operative time and ensuring minimal invasiveness should guide the selection process.Advancements in laparoscopic technology, along with continuous improvements in surgical instruments, promise to enhance the effectiveness and safety of specimen extraction methods. Future developments may focus on refining current techniques, developing new instruments, and incorporating innovative strategies that further reduce complications and improve patient outcomes.Ultimately, staying informed about the latest advancements and understanding the nuances of each technique will allow surgical teams to maximize the benefits of laparoscopic surgery while maintaining the highest standards of patient care.
References
| [1] | Audebert AJ. Laparoscopic surgery of ovarian cyst. Current Opinions in Obstetrics and Gynecology. 1996; 8: 261-5. |
| [2] | Campo S, Garcea N. Laparoscopic conservative excision of ovarian dermoid cysts with and without an endobag. Journal of the American Association of Gynecologic Laparoscopists. 1998; 5: 165-70. |
| [3] | Steiner RA, Wight E, Tadir Y, et al. Electrical cutting device for laparoscopic removal of tissue from the abdominal cavity. Obstet Gynecol. 1993; 81: 471-4. |
| [4] | Carter JE, McCarus SD. Laparoscopic Myomectomy. Time and cost analysis of power vs. manual morcellation. J Reprod Med. 1997; 42: 383-8. |
| [5] | Kresch AJ, Lyons TL, Westland AB, et al. Laparoscopic supracervical hysterectomy with a new disposable morcellator. J Am Assoc Gynecol Laparosc. 1998; 5: 203-6. |
| [6] | Stringer HM, Walker JC, Meyer PM. Comparison of 49 laparoscopic myomectomies with 49 open myomectomies. J Am Assoc Gynecol Laparosc. 1997; 4: 457-64. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML