Halimova E. M., Karimova N. N.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
For the Study, 105 women with a permanent resident of the Bukhara region, diagnosed with relapsing ovarian polycystosis aged 19-35 years, 27 healthy women of reproductive age in the control group were studied. The study found that thus, in tpks patients with obesity and not observed obesity, Lp-PLA2 and LOX-1 factors were statistically reliably increased in Lp-PLA2 levels compared to the control group in both patient groups when patients were tested on TMI independent As such, when its prognostic (AUC) and pathogenetic significance (RR) were examined, it was found that in patients with obesity they were 0.82 and 4.93, respectively, and these results were confirmed in statistical reliability. On the other hand, in patients without obesity, however, it was found to have a prognostic efficacy of 0.60 and a nisbif havf factor of 1.45.
Keywords:
Relapsing polycystosis syndrome, Obesity, Molecular markers, Lipoprotein-associated phospholipase (Lp-PLA2), LOX-1, Obesity, Insulinresistence
Cite this paper: Halimova E. M., Karimova N. N., The Importance of Lp-PLA-2 and LOX-1 Biochemical Markers on Lipid Metabolism in Ovarian Polycystic Relapse, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2929-2932. doi: 10.5923/j.ajmms.20241411.54.
1. Introduction
Functional ovarian cysts occur in 60% of women of reproductive age and tend to increase, rising from 6-12% to 25% [1,2,3,6]. Between surgical interventions performed in gynecological departments, this pathology reaches 25-30% [4,5]. Dyslipidemia is the main metabolic disorder in the development of TPKS [6,7]. As such, patients in the main group were divided into two groups, depending on the TMI indicator in them, in order to more deeply determine the pathogenetic significance of obesity, which is one of the factors inducing ovarian polycystosis syndrome, and in order to identify new molecular markers of practical importance in the prognosis of tpks in the case of obesity. That is, tpks li patients with obesity were 50 (the main group - 55.6%), and tpks patients with obesity were 40 (the comparative group – 44.4%). First of all, the marker of pathophysiological changes characteristic of obesity was examined for biochemical changes. Markers such as lipoprotein-assosiirovannaya phospholipase (Lp-PLA2), and LOX-1 were examined in order to identify new molecular markers in obesity-induced ovarian polycystosis syndrome development. Obesity is often associated with TPKS that are accompanied by anovulation. Insulinresistance in ovarian polycystosis syndrome is one of the main pathogenetic processes bulib, hyperinsulinemia disrupts normal folliculogenesis [8,9,10]. Negative factors associated with obesity disrupt ovarian function and reduce oocyte quality, in addition, can have a subtle negative effect on the receptor apparatus of the endometrium [7,11,12]. Research objective: to study the importance of lp-pla-2 and lox-1 biochemical markers on lipid metabolism in ovarian polycystic relapse.
2. Research Materials and Methods
Prospective investigations examined a total of 132 women in 2020-2022, who were studied in groups of 3. Group 1 is our core group and is made up of 57 women with obesity relapsed TPS. Group 2 was a comparative group of 48 women with non-obesity relapsed TPS. Our group 3 was gynecologically healthy women, which numbered 27. Biomarkers in all groups of women have been identified in serum samples.
3. Results and Discussion
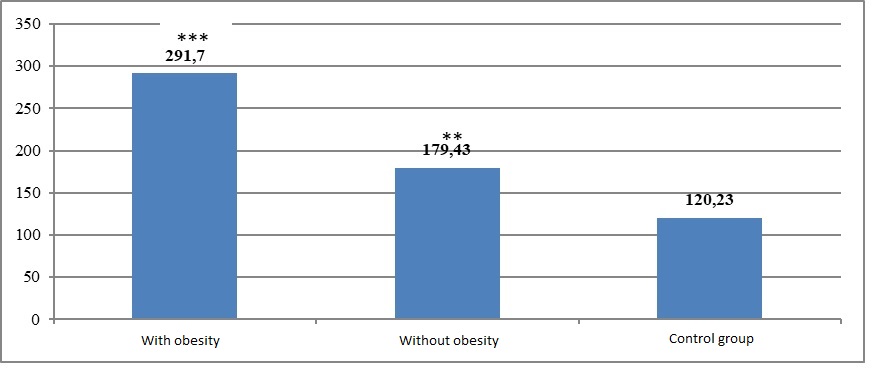
1. the result of the Lp-PLA2 indicator, as shown in Figure-2, was 291.7±13.71 PG/ml (p<0.001) in patients with tpks who were diagnosed with obesity, whereas in patients with tpks who were not diagnosed with obesity, and in the control group, this indicator was 179.43±16.6 PG/ml (p<0.01) and 120.23±6.38 PG/mL, respectively. On the hot side, it was applied that the Lp-PLA-2 concentration indicator is in the normal range (<200 PG/ml), although compared with the control group result, it was found that the qiesian group increased by 1.49 times (p<0.05). In the main group, this increase is even more recent, with an increase of 2.47 (p<0.001) and 1.63 (p<0.01) marobata compared to the control and comparative group indicators.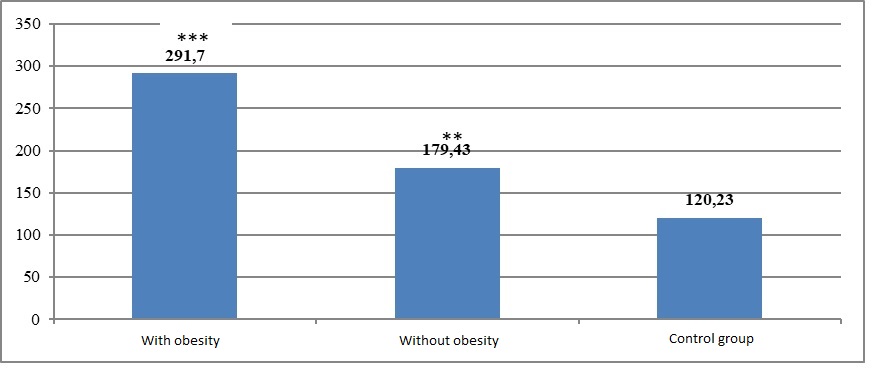 | Figure 1. Lp-PLA2 indicator results (PG/ml) in different guruches. Instruction: * * * - relative to control guru – p<0.001; relative to control guru – p<0.01 |
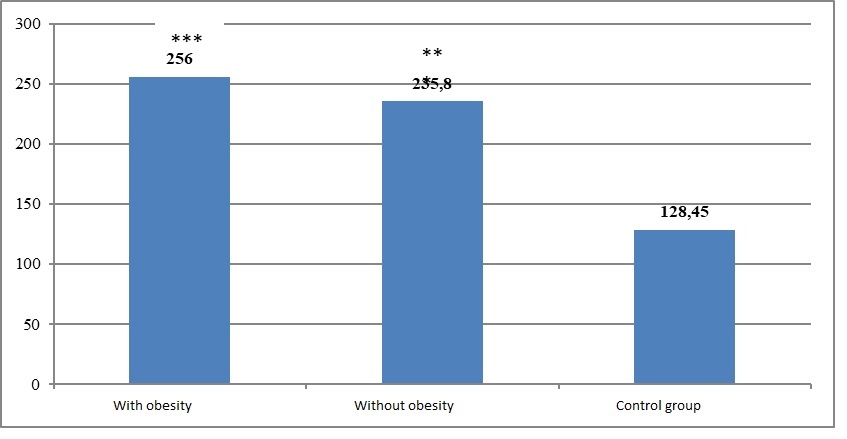
Based on this, the pathogenetic significance of the Lp-PLA2 marker in an independent manner has been investigated, both in TPKS patients where normal weight has been determined. In doing so, tpks that have obesity and do not have obesity have been examined in patients, such as susceptibility (SE); specificity (SP), diagnostic efficacy (AUC), relative havf factor (RR) to test for pathogenetic significance (Table 1). As presented in Table 1, when the importance of the Lp-PLA2 marker in the development of abberant high concentration in the development of TPKS was tested in patients who did not experience obesity in an obese manner and independent of it, the prognostic importance of the cited marker was 0.92 and 0.55 in sensitivity, respectively; the yield was 0.67 for both groups, This applied to the fact that the prognostic significance of the cited marker was very good at predictoring in the case of obesity, and unsatisfactory in the case of non-obesity of Tpks (diagnostic efficacy was assessed as follows: 100-90% or 1.0 – 0.9-excellent, 90-80% or 0.9 – 0.8-very good, 80-70% or 0.8 – 0.7-good, 70-60% or 0.7 – 0.6-average, at the level of 60-50% or 0.6-0.5 bloodless. As such, the next factor examined in the main and control group during our study was lectin-like oxidized zplp receptor-1 (LOX-1), the result of which is shown in Figure 1.2. As shown in Figure 2, Serum LOX-1 concentration, obesity is present, and obesity has been observed in patients with statistically reliable T 2 (p<0.001) and increased by 1.84 (p<0.84) times, respectively, to 256.2±16.78 PG/ml and 235.8±15.2 PG/ml, in the control group this figure was 128.45±6.38 PG/ml. That said, the difference between the groups was not observed much, the main group had a tendency to decrease compared to the control group indicators, the results of these two groups did not differ statistically reliably.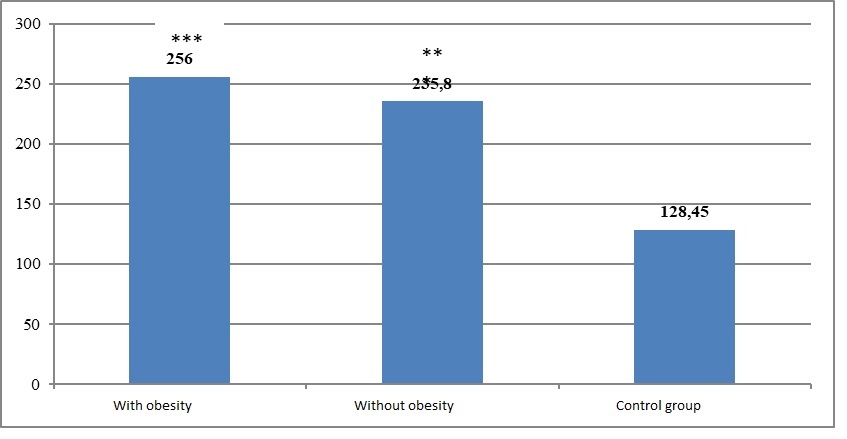 | Figure 2. The results of the concentration of lox-1 in blood serum (PG/ml) determined in different groups. *** – relative to the control group-p<0.001 |
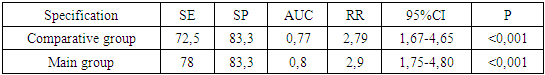
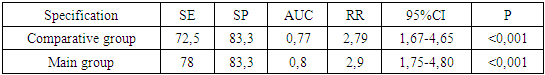
The findings suggest that the LOX-1 concentration constituted a higher concentration in tpks patients in a manner unrelated to their TMI. Shunga monand noted the prognostic and pathogenetic importance of The LOX-1 factor in both groups and compared them (see Table 1).Table 1. The importance of the factor LOX-1 in serum in obesity and the prognosis of ovarian polycystosis syndrome in an independent way for it
 |
| |
|
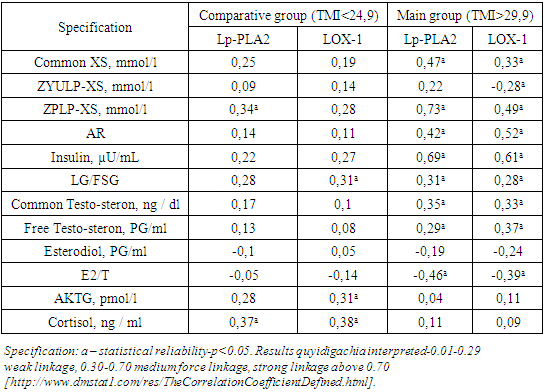
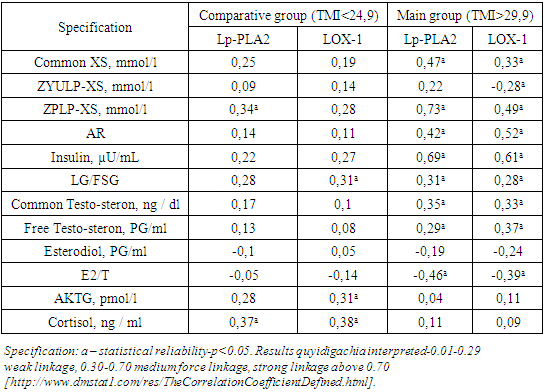
As presented in Table 1, tpks patients with obesity and non-obesity had the LOX-1 factor, 0.78 and 0.725 in sensitivity, respectively; the incidence was 0.83 for both groups, and the diagnostic efficacy was 0.8 and 0.77. Similarly, in the relative risk factor (RR) index, LOX-1 was found to increase tpks developmental risk by 2.79 times (95% CI: 1.67-4.65; p<0.001) in non-obese patients, and 2.9 times (95% CI: 1.75-4.80; p<0.001). The data cited found that increased serum LOX-1 concentration increases tpks risk in patients in an independent manner to TMI.Thus, in TPKS patients where obesity is present and obesity is not observed, Lp-PLA2 and LOX-1 factors were found to have statistically reliable increases in Lp-PLA2 levels compared to the control group in both patient groups when patients were tested on TMI independent Xol. As such, when its prognostic (AUC) and pathogenetic significance (RR) were examined, it was found that in patients with obesity they were 0.82 and 4.93, respectively, and these results were confirmed in statistical reliability. On the other hand, in patients without obesity, however, it was found to have a prognostic efficacy of 0.60 and a nisbif havf factor of 1.45 (p>0.05). This means that the Lp-PLA2 factor is important in tpks development when the obesity factor is added, not in an independent case. On the other hand, the amount of the Lox-1 marker was found to be a statistically reliable balance relative to the control group in both patient groups. At the same time, its prognostic effectiveness was found to be very good and good in comparison to patients with obesity and not observed. According to the relative risk factor indicator, due to the importance of The LOX-1 marker in both patient groups as an increase in the development risk of ham TPKS, we concluded that the LOX-1 marker is a significant factor in the prognosis of TPKS in patients independent of TMI.As such, with the goal of a deeper understanding of the pathogenetic significance of the markers examined, cross correlation analysis was conducted between the Lp-PLA2 and LOX-1 biomarkers, as well as the results of some biochemical tests (see Table 2). As presented in Table 2, patients with non-obese Tpks were found to have Lp-PLA2 activity and zplp-Xs levels, statistically reliable mean-strength positive bond among cortisol indicators, and with LOX-1, positive mean-strength bond between LG/FSG, AKTG, and cortisol levels.Table 2. Correlation analysis of LP-PLA2 and LOX-1 biomarkers in patient groups with other biomarkers
 |
| |
|
On the other hand, it has been found that tpks patients with obesity have strong positive binding between Lp-PLA2 and ZPLP-Xs, a common Xs, AR indicator, insulin, LG/FSG, while between common testosterone there is a medium-strength positive binding and with free testosterone there is weak positive binding, and with E2/T there is a medium-strength negative binding. In addition, The LOX-1 indicator and other biomarkers were found, notably the general Xs, ZPLP-Xs, AR, insulin, LG/FSG ratio, the presence of a positive mid-strength bond between the general and free testosterone indicators, and the mid-strength reverse bond with the E2/T ratio. When the results of the induced correlation analysis were predicted, it was found that there was a statistically reliable Association of Lp-PLA2 and LOX-1 markers with tpks-specific biomarkers (LG/FSG, total and free testosterone, estradiol, and E2/T ratio) only in patients with obesity, on the other hand such a result was not observed in non-obese patients. This means that correlation analysis indicator Lp-PLA2 and LOX-1 biomarkers do not have the acamicity in the development of obesity-independent xolda TPKS.
References
| [1] | Alieva, F. N. Izuchenie osnovnix etiopathogeneticheskix michanov formirovaniya syndroma polycystoznix yaichnikov / F. N. Alieva, N. V. Samburova // molodezhny nauchny forum: estestvennie i medisinskie nauki. – 2017. – № 2(41). - S. 16-25. |
| [2] | Blesmanovich, A. E. Syndrome polikistoznich yaichnikov: classics I Sovremennie nyuansi / A. E. Blesmanovich, Yu. A. Petrov, A. G. Alexina // magazine nauchnix statey Zdorove I obrazovanie v XXI veke. – 2018. - T. 20. – № 4. - S. 33-37. |
| [3] | Glukhova M. V. Osobennosti klinicheskix, hormonalnix I metabolicheskix narusheniy u bolnix s syndromom polikistoznix yaichnikov s raznimi tipami ojireniya I normalnoy Massoy tela / M. V. Glukhova, T. V. Draznina, T. V. Karpov [I dr.] // Upravlenie kachestvom medisinskoy pomotshi. – 2016. – № 1-2. - S. 33-37. |
| [4] | Grigoryan, O. R. Syndrome polycystaznix yaichnikov-atdalennie risk / o. R. Grigoryan, E. N. Andreeva // Effektivnaya pharmacotherapy. – 2015. – № 5. - S. 20-25. |
| [5] | Nayimova N.S., Karimova N.N. Specificity of changes in hormones and enzymes in early ovarian failure // a new day in medicine. - Tashkent, 2023. - №8(58). - S.52-56. |
| [6] | Nayimova N.S., Karimova N.N. Innovasionnie biosimicheskie marktor reproduktivnogo zapasa he jentshin s prejdevremennoy nedostatochnostyu yaichnikov // a new day in medicine. - Tashkent, 2023. - №3(53). - S.170-175. |
| [7] | Nayimova N.S., Karimova N.N. Osobennosti ultazvukovix izmeneniy u jentshin s prejdevremennoy nedostatochnostyu yaichnikov // Novosti dermatovenerologii I reprodutivnogo zdorovya. - Tashkent, 2023. - №1(101). - S.28-30. |
| [8] | Nayimova N.S. Osobennosti vzaimosvyazi biosimichesix izmeneniy u jentshin c prejdevremennoy nedostatochnostyu yaichnikov s indexom massi tela I drugimi zabolevaniyami / / Journal teoreticheskoy I klinicheskoy medisini. - Tashkent, 2023. -№2. - S.154-157. |
| [9] | Karimova N.N., Naimova N.S., Halimova E.M., Karimov D.N. Metodi korrektsii hormonalnogo dysbalansa U jentshin s syndromom prejdevremennoy nedostatochnosti yaichnikov // New Day in medicine. - Tashkent, 2021. -№3(35/1). - S. 203-206. |
| [10] | Nauimova, N.S., Karimova, N.N. (2022) Disharmony and its correction in premature ovarian insufficiency. Journal of Pharmaceutical Negative Results, 13, DOI: 10.47750/pnr.2022.13.S08. 409. |
| [11] | Yoldoshevich, P. O., & Nabidjanovna, K. N. (2020). Retrospective analysis of the birth histories of women who have suffered bleeding in order to optimize approaches to the prediction and prevention of postpartum bleeding. European Journal of Molecular and Clinical Medicine, 7(2), 6236-6243. Retrieved from www.scopus.com. |
| [12] | Karimova N.N., Ayupova F.M., Rustamov M.U. "Analysis of childbirth stories with postpartum hemorrhage, taking into account rehabilitation measures and future of reproductive system after massive obstetric bleeding" International // Journal of Pharmaceutical Research, / Jan-Mar 2019/Vol 11. Issue 1. - R.1690-1695. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML