-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2912-2918
doi:10.5923/j.ajmms.20241411.51
Received: Nov. 6, 2024; Accepted: Nov. 20, 2024; Published: Nov. 21, 2024

Impact of Appointment Scheduling in Patient Experience
Anshuman Srivastava1, Rishika Sharma2, Shagun Sinha3
1Family Medicine, Family Healthcare Network, 305 E Center Avenue, Visalia CA 93291, USA
2Pediatric, Family Healthcare Network, 305 E Center Avenue, Visalia CA 93291, USA
3Student, New York University, 726 Broadway, 3rd Floor, New York, NY 10003, USA
Correspondence to: Anshuman Srivastava, Family Medicine, Family Healthcare Network, 305 E Center Avenue, Visalia CA 93291, USA.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Appointment booking plays a key role in shaping how patients feel about their healthcare visits. A good booking process can boost a patient’s experience by cutting down on wait times, making care easily accessible, and making visits overall more efficient. On the flip side, a poor booking process often causes long waits, lowering patient satisfaction. This paper looks at how appointment booking affects patient satisfaction, showing how a good booking system can lead to better results. Key points include how tech helps improve booking, such as online systems and automatic reminders, which can make the process easier and reduce missed appointments. Also, having flexible booking choices and managing time slots are vital to meeting patient needs and avoiding disruptions. When healthcare providers focus on making appointment scheduling more accessible, it improves the patient's experience. This leads to better care, more loyal patients, and better health results overall. Good scheduling doesn't just make things run - it's key to putting patients first. It makes sure they get the right care at the right time.
Keywords: Appointment scheduling, Patient experience, Wait times, Healthcare access, Scheduling technology, Patient satisfaction
Cite this paper: Anshuman Srivastava, Rishika Sharma, Shagun Sinha, Impact of Appointment Scheduling in Patient Experience, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2912-2918. doi: 10.5923/j.ajmms.20241411.51.
Article Outline
1. Introduction
- In the changing face of healthcare, patient experience is becoming pivotal to comprehensive quality care and satisfaction. One of the ways this experience is influenced is through appointment scheduling, the process that is the first port of call for patients to their healthcare providers. Providers require efficient appointment scheduling systems that are fundamental to timely care, shortened wait times, and lessened administrative burdens. Inaccurate, mismanaged scheduling can lengthen wait times, heighten patient frustration, and ultimately cause decreased health outcomes.Is there more to patient experience than convenient appointment scheduling? A look at several different stages of the healthcare delivery process such as, how well appointment information matches up with actual appointments made by patients, and how easy it is to schedule an appointment in the first place or get a response from a healthcare facility. The benefits include better patient flow, optimal provider efficiency, and an increased ability to facilitate overall healthcare management.The present paper explores the role of appointment scheduling in determining overall patient experience from multiple perspectives. It examines how recent scheduling innovations, from automated algorithms and linked electronic health records to more standardized processes, play out in patient satisfaction, access to care, and operations. Additionally, the study will investigate what difficulties and obstacles exist for healthcare providers to implement and sustain scheduling systems that work.How appointment scheduling can be optimized in order to positively influence patient experience. The results are expected to provide direction for healthcare administrators and policymakers who work to enhance service delivery and patient outcomes in an evolving healthcare system.Primary care clinics, specialty care clinics, and hospitals have been using appointment scheduling systems to manage access to providers and schedule elective surgeries. Multiple factors that affect the performance of appointment systems, such as arrival and service time variability, patient and provider preferences, available information technology, and the scheduling staff experience. As per one of the studies, the fundamental difficulty in scheduling is to deal effectively with uncertainty and variability. Variability in service times is essential in specialty care and surgery, and scheduling in healthcare is often confronted with random no-shows, cancellations, walk-ins, and emergencies (Çayirli & Veral, 2003; Çayirli et al., 2006; Deceuninck et al., 2018; Gupta & Denton, 2008; Zacharias & Pinedo, 2014), [2-6].
2. Importance of Appointment Scheduling
- Appointment scheduling plays an important role in healthcare management and contributes massively to patient experience. One can take the context of accessibility, efficiency, and satisfaction to better understand why it is important. Here are a few reasons why appointment scheduling is crucial for enhancing patient experience:Reducing Wait Times: Efficient appointment scheduling systems are pivotal to lowering wait times and are considered one of the most important factors in patient satisfaction. Delays can make patients quite understandably frustrated and leave them with poor perceptions of the quality of care. By deploying a state-of-the-art scheduling system, healthcare providers can attend patients in a timely manner and reduce waiting time ensuring a pleasing experience.The utilization of healthcare services depends on how long a patient waits to be seen by a doctor. Longer wait times are seen as a barrier to obtaining services and keep patients waiting unnecessarily, causing stress for both the patient and the doctor. [7,8]Improving Access to Care: A well-organized scheduling system ensures that patients are able to get the care they need on time. A proper system enables health providers to use slots more efficiently, and make it possible for a patient to get an appointment at the actual date & time. Specifically in patients who need urgent care or have a regularly scheduled follow-up.Advanced access is an appointment scheduling system that allows patients to receive health care from their providers at the time of their choosing. Traditional scheduling systems arrange appointments for future dates, resulting in each physician's patient care time being mostly scheduled well in advance, [9]. Enhancing Provider Efficiency: This not only helps patients, but also increases provider efficiency. It also helps providers streamline their workflow, make the most of their time, and minimize scheduling-related administrative work by eliminating double-booked appointments and empty appointment slots. This efficiency equates to less wasted time and more time spent on direct patient engagement, translating directly to better patient care. Studies have suggested that scheduling lower-variance, shorter appointments earlier in the clinic (conversely, higher-variance, longer appointments later) results in overall less patient waiting without reducing physician utilization or increasing clinic duration, [11].Decreasing No Show and Cancellation Rates: An effective appointment scheduling system would reduce no-shows and cancellations by sending regular reminders or communication. Sending automated reminders to patients via phone, text, or email can prevent no-shows and help ensure doctors are able to use their time servicing patients in need. Patients arriving with appointment requests may choose one of the days offered to them or leave without an appointment. Patients with scheduled appointments may cancel or not show up for the service. The service provider collects a “revenue” from each patient who shows up and incurs a “service cost” that depends on the number of scheduled appointments, [12].Improving Communication: More sophisticated scheduling systems may have capabilities that allow for improved communication between patients and healthcare providers. This may involve online scheduling portals, patient access appointment management portals, and even in-line text communication to hash out schedule alterations. Better communication helps patients feel more knowledgeable and engaged in their care, leading to an improved patient experience overall.Improves patient satisfaction: Patient satisfaction is fundamental to the success of your appointment scheduling overall. And patients can be quite happy with their care if they get through scheduling procedures intelligently and efficiently. Such high levels of satisfaction, in turn, result in higher patient loyalty, more referrals, and an enhanced brand for providers.Supporting Personalized Care: Today, advanced scheduling systems can connect to electronic health records (EHRs) and other healthcare technology to help your practice deliver excellent personalized care. By tapping into patient history and preferences, providers can personalize appointment times and follow-up schedules to patients' specific needs – enhancing the value and quality of care provided.Appointment scheduling is a foundational element of the patient experience as it’s the starting point in the patient’s journey. By investing in effective scheduling systems and practices, healthcare providers can significantly improve the quality of care and overall experience for their patients.It has been widely recognized that a well-designed healthcare process must provide timely and easy access to healthcare facilities for all patients [13]. Appointment Scheduling (AS) can reduce patient wait times and thus enhance the utilization of expensive staff and facilities’ medical resources. AS aims to build an appointment system that optimizes a specific quality standard in a healthcare application of scheduling tasks under uncertainty. Healthcare management programs’ primary function is to minimize patient wait times and thus improve patient satisfaction [14]. There might be several obstacles to healthcare services coping with many outpatients. For example, a longer wait time for treatment may negatively impact the patient's experience and diminish the quality of care [15]. In general, healthcare facilities such as hospitals and clinics accumulate more patients needing their services. To cope with this, hospitals must implement quick and adequate healthcare facilities to accommodate new patients and keep people prioritizing them [16]. They must successfully identify the bottlenecks, anticipate the effects of diversity on demand, and compute the optimal capacity distribution [17]. Healthcare centers are evaluated by recognizing the best methods, applying measurable techniques, and having an obligation to improve. Clinics use decision support systems to provide low-cost and assessable services to individuals to preserve the care and quality of services [18]. The solutions present in this literature aim to reduce waiting times by developing decision-support systems to manage outpatient clinic services [19]. Over recent years, the healthcare system has been strained to provide patients with high-quality services despite in sufficient funding. One of the most important issues in healthcare is ASP, which has improved quality and provided prompt access to health facilities. Time is essential in ensuring patient safety and performance, and time is a crucial determinant of patient satisfaction [20].
3. Critical Components of Scheduling
- This is an important aspect of healthcare where there are multiple parts that involve deciding when to schedule patients for appointments and balancing the schedule so that physicians, patients, and staff (eg. nurse) can utilize their time optimally. Essential elements of appointment scheduling in healthcare:Appointment Scheduling System: This is the scheduling software or platform that you use to make appointments. It may be an independent system or incorporated with healthcare platforms such as Electronic Health Records (EHRs).Features: It involves applications related to creating appointments, rescheduling an appointment, and cancelling appointments with varying types of appointments and durations.Patient Check In & Intake: Patient information- Obtain and store Patient Demographics, Medical History, and Insurance details. Intake Forms- taking required forms and consents (can be completed online, in-office) before the appointment.Appointment Types and Slots: Examples include Appointment Types (specific appointments such as regular check-ups, urgent visits, specialist consultations..). Time Slots- Controlling the time slots of different types of appointments and making sure they match healthcare providers’ availability.Provider Availability: Scheduling Providers, Tracking and Managing the availability of Healthcare Providers: working hours, days off, and specializations.Managing Resource Allocation: This includes managing the appointment slots so that they do not exceed the number of providers available and other necessary resources such as examination rooms and medical equipment.Follow-up management: due dates before they approach, via automated tasks and notifications.Appointment Reminders: It sends phone calls, text, or email reminders to patients who have an upcoming appointment scheduled. Notifications for follow-up appointments or any such required pre-appointment actions.Patient Communication: Allowing patients to schedule, confirm, or change appointments via online portals; mobile apps; or phone-based courtesy calls.Supporting the customer: Patient assistance in troubleshooting scheduling problems and appointment related inquiries.Management of No-Show and Cancellations: Monitoring no-show and late cancellation rates to identify process improvements for appointment scheduling and patient communications. Policy Enforcement- Creating policies and procedures for handling high no-show or cancellation rates, which can include fees and rescheduling processes.Well-Integrated with EHR (Electronic Health Records): Synchronize with clinical scheduling to have all requisite info in patient records for that appointment and relevant notes etc. Information Access- Providing healthcare providers with additional patient information and background when scheduling an appointment, to customize the visit accordingly.Analytics and Reporting: Key points for consideration Performance Metrics: Appointment volume, wait times and other access metrics, patient satisfaction, and provider efficiency. Data analysis - The use of data in order to spot trends, schedule better, and manage appointments more efficiently.The Interface and Accessibility: User Interface: Creating a friendly and intuitive design for all users (for both patients as well as healthcare workers) with the goal of facilitating the easiest experience when scheduling an appointment. Accessibility- Confirm that the scheduling system is accessible to those with disabilities and provided in multiple languages if required.Mobile and Online Access: Attending online scheduling solutions using patient portals or mobile apps; helping patients in booking and managing appointments. Mobile Integration- Including mobile-responsive scheduling options to improve access and usability for busy patients.Primary and specialty care has been using appointment scheduling systems to manage access to service providers, as well as by hospitals to schedule elective surgeries. There are many factors that affect the performance of appointment systems, including arrival and service time variability, patient and provider preferences, available information technology, and the experience level of the scheduling staff [21], and patient satisfaction with an appointment system when they attempt to book a non-urgent appointment and it is affected by the ability to book with a provider of choice and to book an appointment at a convenient time of day. For a medical condition requiring urgent attention, patients had quick access to a familiar physician. For example, access to same-day/urgent slots is essential for the clinic. A significant challenge when designing an outpatient appointment system is the difficulty of matching randomly arriving patients’ booking requests with physician's available slots in a manner that maximizes patients’ satisfaction as well as clinic revenues. What makes this problem difficult is that booking preferences are not tracked, may differ from one patient to another, and may change over time [23].
4. Challenges & Consideration of Advance Scheduling Systems
- In healthcare industry implementing advanced scheduling systems poses certain challenges & resistance. Clinicians and administrative staff in the workplace may be hesitant to embrace any new technology or could be fear of what their experience/role will be post implementation. That resistance might be due to uncertainty about the future, discomfort with change, or distrust that the system itself will really do a better job & replace their existing role. This resistance can be overcome through forging trust, effectively communicating the rationale and benefits of the change and giving concerned staff a voice in the decision-making process which often ensures buy-in and less friction when implementing something new.On Technology side, the integration of the new scheduling system with existing infrastructure (e.g., electronic medical records or other enterprise systems) represents another key challenge. Data needs to flow seamlessly from system to system, and ensuring that will keep errors at bay and the process running efficiently. Yet, that can be a complicated process, providers need time, knowledge, and resources to implement such integration. Another vital factor is data privacy, since healthcare organizations are required to follow strict regulations such as HIPAA in the US or GDPR in the EU. Protecting patient data during the integration and operational phases may be a challenge and is critical, which makes the implementation to be carefully thought through. However, the benefits of advance scheduling system outweighs the human, technology & privacy challenges.A more sophisticated scheduling system can contribute immensely to getting an advanced experience by creating utmost convenience, shortening the wait time, and enhancing communication. Offering online self booking, automated reminders, status update reminders, and real-time appointment availability, all of which allow patients to book or cancel an appointment whenever they like, anywhere they like, without beating to the physician office phone chorus during work hours. This type of flexibility provides patients with flexibility and no more waiting on long hold times or time of day when they are able to speak with a care team. Sending automated reminders further minimizes missed appointments, which translates into improved adherence to care plans and seamless patient care delivery.Finally, more sophisticated scheduling systems tend to optimize appointments more effectively minimizing patient wait times and maximizing provider time utilization. These systems are capable to reduce wait times, by reducing empty slots between timetable and also to help from over booked, so that patients do not spend long time waiting in the waiting area. In addition, improved patient flow implies that the healthcare provider will be able to provide more personalized and timely care.
5. Future Scope
- The future potential of appointment scheduling in healthcare looks set to take great strides forward, fuelled by new technologies and changing patient demands. The changing landscape of appointment scheduling is rapidly evolving with advanced technologies:Advanced AI and Machine Learning IntegrationPredictive Analytics: AI-powered scheduling systems will utilize predictive analytics to predict appointment demand, slot availability, and no-shows. Predictive algorithms using historical data will determine patient needs, and schedules can be adjusted accordingly by the AI.Custom Scheduling: AI algorithms empower custom scheduling options according to the patient and past experiences, which will make way for a better patient journey.Telehealth Integration ImprovedHybrid Scheduling Models: Combining telehealth with scheduling enables virtual and in-person appointments to occur interchangeably, offering more convenient options for patients and providers.Advanced Telehealth Platforms: Next-gen scheduling systems will combine a suite of advanced telehealth capabilities, including virtual waiting rooms, fully integrated video conferencing tools, and real-time patient-provider communication.High-End Patient Portals: Patients with high-end portals will be able to book, reschedule, and cancel appointments on the fly and get a whole range of additional appointment-specific information.Mobile-First: As smartphone usage increases, more and more mobile-first solutions will come up to solve scheduling problems using interfaces that are customized for on-the-go appointment management.Streamlined EHR Integration: Moving forward, future scheduling software will have even greater integration with EHRs so that patient records can be automatically updated as well as appointment history and care plans to help coordinate care and improve efficiency.Data-Based Insights: Better integration with EHRs will deliver rich insights into patient scheduling patterns, which can be used by healthcare providers to optimize their workflows and care delivery.Automated Scheduling Algorithms: Sophisticated algorithms will automate the scheduling process, saving time from handling administrative work and cutting down human error. These systems will be able to handle complex scheduling situations, e.g. scheduling multiple providers and availability of resources.Robotic Process Automation (RPA): RPA can be used to execute all repetitive scheduling tasks like reminders to send, appointment status updates, and cancellation processing.Personalized Communication: In the future, systems will allow for more custom communication like reminders, follow-up messages, and appointment preparation instructions configured to meet the specific needs of individual patients.Patient Preferences: Systems will allow for the customization of appointment times, types, and communication preferences resulting in a more personalized and ultimately satisfactory experience.Advanced Analytics & ReportingReal-Time Analytics: Scheduling systems will give real-time analytics and dashboards to keep an eye on appointment metrics, individual practice flow, and provider performance as the scheduling evolution unfolds ensuring better decision making backed by data.Predictive Reporting: More advanced reporting tools will leverage predictive analytics to predict appointment trends, determine where bottlenecks could occur, and provide suggestions for changes to improve the efficiency of the process.Patient Feedback Integration: Future systems will feature an option for automated collection and analysis of patient feedback on the scheduling process in order to improve the experience.Improved Security Protocols: As data security regulations that complement privacy requirements evolve, scheduling systems will adopt a more robust set of security measures to keep all patient identifying information (PII) secure and compliant with the likes of HIPAA.Compliance Automation: Compliance checks should be enforced for best practices and compliance against industry standards, scheduling industry. As healthcare goes global, scheduling systems will feature multi-language support and grow to accommodate different regional practices and regulations.When making an appointment, patients are generally unaware of how much clinician time is available to address their concerns. Similarly, the primary care clinician is often unaware of what the patient expects to accomplish during the visit, leading to uncertainty about how much time they can allot to each sequentially appearing concern, and whether they can reasonably expect to address necessary preventive services and chronic disease management, [22]. The scheduling of outpatient departments has become more important in healthcare systems aiming at the efficient utilization of available hospital resources to provide satisfactory services to patients. Patient access to healthcare services and extended wait durations have been identified as major problems in ambulatory care systems [23,24].
6. Conclusions
- The ability of a patient to schedule an appointment is crucially important in the healthcare industry and impacts both patient experience and operational efficiency. While healthcare continues to change, efforts like these are proving how intelligent scheduling tactics and applied technology (AI, Predictive analytics, and Tel Health) disrupt conventional renewals at scale. The advancements are said to increase precision and efficiency in appointment management, and in turn reduce patient wait times and provide provider workflows. These technologies will enable healthcare to be more convenient, and provider schedules more agile in response to patient demands. Though, the future of appointment scheduling will drift towards an even more personalized and automated scheduling experience. Optimized scheduling for individual patient preference and predictability of needs based on more accurate AI, machine-learning prediction models Advanced AI, machine learning algorithms, increasing ability to predict patient need; significant reduction in no show rates. New patient self-service offerings and mobile-first capabilities will make it easier and more convenient for patients to take control of their scheduling. Such a move towards more tailored and automated procedures will allow healthcare professionals to offer a better experience to their patients at the same time as enhance in total operational efficiency.To Summarize, the changing landscape of appointment scheduling is a microcosm of the broader adoption of health technology and data-driven solutions. And, as the systems get better not only saving time but helping patients achieve an ultimately more engaging and effective experience. Further developments in scheduling tools will continue to have the potential to revolutionize the way health professionals engage with their patients, ultimately leading to healthier individuals and a more responsive healthcare infrastructure. While these changes progress, it will be necessary for healthcare providers to keep pace with technology advancements and how their services can scale to include the needs of the patients of today.
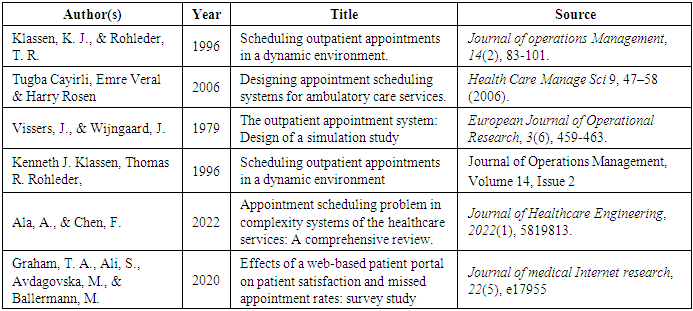
7. Literature Review
- Literature review on the impact of appointment scheduling on patient experience presented in a tabular format. Each entry summarizes the key findings, methodologies, and implications of relevant studies.
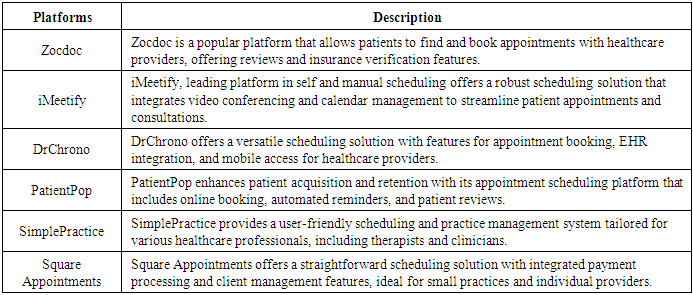
8. Existing Players in Appointment Scheduling
- Here are a few leading online appointment scheduling players in the ecosystem.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML