-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2824-2826
doi:10.5923/j.ajmms.20241411.31
Received: Oct. 16, 2024; Accepted: Nov. 10, 2024; Published: Nov. 13, 2024

Clinical and Demographic Characteristics of Patients Included in the Registers
Turaev Hikmatilla Negmatovich1, Ziyadullaev Shukhrat Khudayberdievich2, Ismailov Jamshid Abduraimovich3
1Assistant of the Department of Clinical Pharmacology of the Pharmaceutical Faculty of the Samarkand State Medical University, Uzbekistan
2Doctor of Medical Sciences, Professor, Deputy Director of the Institute of Immunology and Human Genomics of Academy of Sciences of Uzbekistan, Uzbekistan
3Head of the Department of Internal Medicine №4, Samarkand State Medical University, PhD, Associate Professor, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Sudden cardiac death (SCD) as an irreversible outcome and the result of sudden cardiac arrest reaches 50% among other outcomes in persons 35–50 years old, predominantly male, but recently there has been a tendency to increase the proportion of females, as well as adolescents and young adults. The risk of sudden cardiac death is higher in men and increases with age due to the higher prevalence of coronary artery disease among older people. The number of cases of SCD ranges from 1.4 per 100 thousand person-years (95% CI - 0.95-1.98) in women to 6.68 per 100 thousand person-years (95% CI - 6.24 –7.14) in men. The number of cases of SCD among the younger generation is 0.46–3.7 per 100 thousand person-years, which translates into 1100–9000 deaths in Europe and 800–6200 deaths in the United States each year. Data on the prevalence of SCD in Uzbekistan are limited, including the peculiarities of SCD registration in different countries.
Keywords: Arrhythmia, Antithrombotic therapy, Coronary heart disease
Cite this paper: Turaev Hikmatilla Negmatovich, Ziyadullaev Shukhrat Khudayberdievich, Ismailov Jamshid Abduraimovich, Clinical and Demographic Characteristics of Patients Included in the Registers, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2824-2826. doi: 10.5923/j.ajmms.20241411.31.
1. Annotation
- Myocardial infarction is the most frequent cause of the development of rhythm disorders. Structurally, myocardial infarction is characterised by prolonged ischaemia of a single section of heart muscle, the causes of origin of which may be atherothrombotic coronary artery disease, coronary embolism, coronary spasm, prolonged tachyarrhythmia, blood loss, severe anaemia or respiratory failure [3,5]. Ultrastructural changes begin to occur at the 10th minute (has been determined in the human ischemic heart), and include glycogen depletion, myofibril relaxation, sarcolemma rupture, functional abnormalities of mitochodria, and others; these changes are followed in the next few hours by necrosis and programmed types of cell death such as apoptosis and autophagy [2,6].During ischaemia, the absence of oxygen by one mechanism leads to suppression of oxidative phosphorylation in mitochondria, which is restored by reperfusion of the ischaemic site, but there is also an abrupt release of reactive oxygen species originating from complex I in the electron transport chain. Succinate increases the respiration associated with complex II succinate dehydrogenase, possibly causing an overload of the capacity of the electron transport system and triggering a reverse electron transport to complex I and a further increase in the generation of reactive oxygen species. These phenomena contribute to further mitochondrial dysfunction and damage, which causes cardiomyocyte death and aggravation of myocardial damage [1,7].Restoration of blood supply to the ischemic area causes dramatic biochemical and metabolic changes that cause ischemia-reperfusion injury based on excessive production of reactive oxygen species, opening of mitochondrial permeability transition pores, decreased ATP production, release of pro-inflammatory signalling molecules, induction of apoptosis and other types of programmed cell death, and other mechanisms [7,9]. Unfavourable consequences of ischemia-reperfusion injury development may include myocardial stagnation and hibernation, phenomenon of no blood flow recovery, ventricular arrhythmias, contractile dysfunction and lethal reperfusion injury. Lethal reperfusion injury represents an additional inducer of cell death distinct from ischaemic injury [8]. In turn, cardiomyocytes possess molecular mechanisms, the induction of which increases their resistance to ischaemic-reperfusion injury - cardioprotection [2,3].
2. Materials and Methods
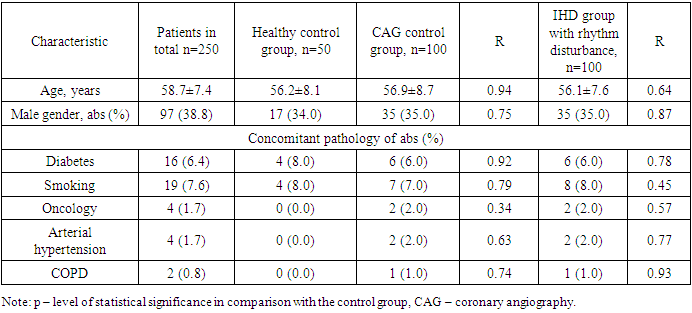
- The work was structured in several stages. At the first stage, data from international and national registers of patients with cardiac rhythm disorders were analysed. For this purpose, a search was performed in PubMed and MEDLINE search engines, using the following keywords: arrhythmia, coronary heart disease, rivaroxaban, dabigatran, warfarin, atrial fibrillation, new oral anticoagulants, direct oral anticoagulants, arrhythmia, coronary heart disease, real clinical practice, Rivaroxaban, Dabigatran, Apixaban, Warfarin, atrial fibrillation, new oral anticoagulants (NOACs), direct oral anticoagulants (DOACs). Registries included in the analysis had to fulfil the following criteria: international and national registries of patients with cardiac rhythm disturbances resulting from myocardial ischaemic injury and including information on the presence of antiplatelet therapy. The retrieved studies were analysed according to the following criteria: design, number and characteristics of included patients, risk stratification for stroke, antithrombotic therapy administered.At the second stage, a retrospective pharmacoepidemiological study was conducted to investigate the pharmacoepidemiology of antithrombotic therapy in heart rhythm disorders. The object of the continuous retrospective pharmacoepidemiological study were medical records of inpatients (form 003/u) with the diagnosis of ‘Atrial fibrillation’ (ICD-10 code - I48), consecutively admitted to the cardiology department of the MU of Samarkand and Ufa. It was decided to focus on this category of patients due to the high frequency of thromboembolic complications in this group and the highest incidence among other manifestations of rhythm disorders. At this stage, 382 case histories of inpatients were included in the analysis. Inclusion criteria: age of patients older than 18 years, established diagnosis of atrial fibrillation (ICD-10: I48.0, I48.1, I48.2) of ischaemic genesis. Exclusion criteria: Cardiomyopathies of non-ischaemic genesis (I42- I43 according to ICD-10), thyrotoxicosis (E05 according to ICD-10), congenital heart defects (I34- I36 according to ICD-10), rheumatic heart lesions (I01, I05-I09 according to ICD-10), acute coronary syndrome (I20-I24 according to ICD-10), endocarditis (I33 according to ICD-10), myocarditis (I40-I41 according to ICD-10), pericarditis (I30-I32 according to ICD-10), pulmonary embolism (TELA) (I26 according to ICD-10).For comparison with the indicators of the haemostasis system of healthy volunteers and patients with thrombosis, a sample of patients (n=100) staying in the cardiology department of GBUZ RKB named after G.G. Kuvatov and a control group of healthy volunteers (n=50) was formed, which did not differ in the main criteria from the patient groups. Table 1 presents demographic and clinical parameters of patients included in the prospective part of the study.
|
3. Result
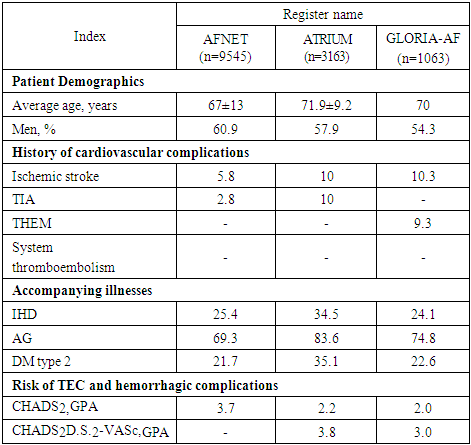
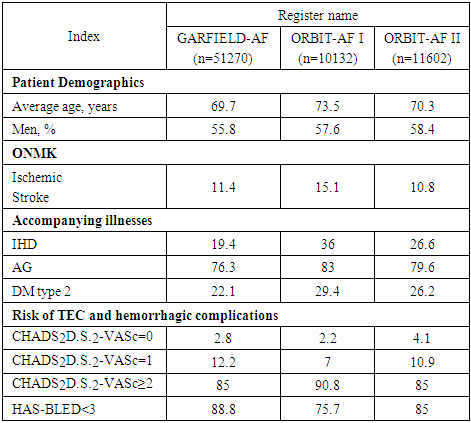
- Clinical and demographic data of patients included in the international registries AFNET, ATRIUM, GLORIA-AF are presented in Table 2.
|
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML