-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2818-2823
doi:10.5923/j.ajmms.20241411.30
Received: Oct. 22, 2024; Accepted: Nov. 8, 2024; Published: Nov. 12, 2024

Transcranial Magnetic Stimulation for Early Rehabilitation Using Improved Cylindrical Cages in Patients with Complicated Cervical Spine Hernia
Shаdmаnov B. R., Sattarov A. R., Saidov S. S., Rizaeva D. Sh
The National Centre of Rehabilitation and Prosthetics of Person with Disabled’s, Tashkent, Uzbekistan
Correspondence to: Shаdmаnov B. R., The National Centre of Rehabilitation and Prosthetics of Person with Disabled’s, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

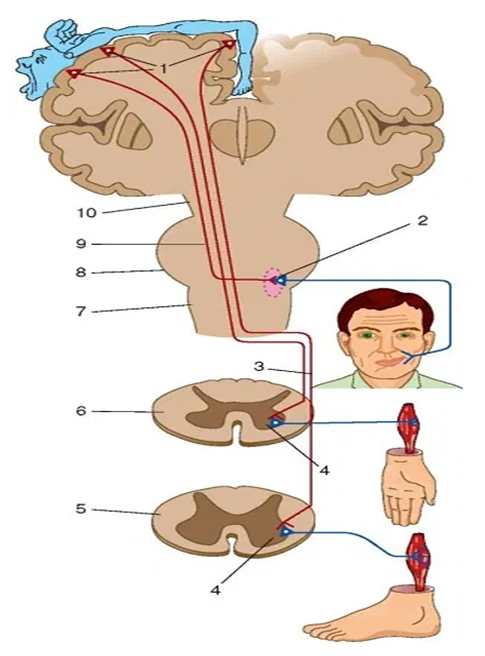
According to US population health statistics [1], most people under the age of 45 are limited in their activities due to persistent back and neck pain, and the prevalence of chronic spinal pain among the elderly population reaches 26-32%. Spinal pathology ranks 5th among the causes of hospitalization and 3rd among indications for surgical treatment [1]. Diseases of the peripheral nervous system account for more than 50% of the disability of the elderly population of Russia. High level of disability: disability occurs in 80% of cases due to secondary damage to the peripheral nervous system on the background of spinal diseases [2]. In addition, neck and back pain restrict vital activity, reduce the quality of life, change the psyche and behavior. More than half of patients with osteochondrosis of the spine have symptoms of chronic emotional stress [2]. One of the modern and promising neurotherapeutic methods is high-intensity magnetic stimulation in the early period after the removal of herniated discs. The magnetic field has no thermal effect, is easier to tolerate by patients than electromagnetic exposure, and has fewer contraindications. The magnetic field causes positive (positive) changes in the physiological and biological processes of the nervous system [3]. When treated with a magnetic field, the sensitivity of the receptors of the peripheral nervous system decreases, which leads to a decrease in pain and an improvement in conductivity; axon growth, improving axon myelination and inhibiting the development of connective tissue in them, promotes the regeneration of damaged peripheral nerve endings [4,5].
Keywords: TMS stimulation
Cite this paper: Shаdmаnov B. R., Sattarov A. R., Saidov S. S., Rizaeva D. Sh, Transcranial Magnetic Stimulation for Early Rehabilitation Using Improved Cylindrical Cages in Patients with Complicated Cervical Spine Hernia, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2818-2823. doi: 10.5923/j.ajmms.20241411.30.
1. Introduction
- So, in 2014, S.C. Barros Galvão and others investigated the effectiveness of randomized double low-frequency placebo-controlled stimulation of the M1 cortex (1 Hz) of the intact cerebral hemisphere in relieving post-stroke spasticity. After 10 sessions of stimulation and a course of physical therapy, 90% of patients immediately and 55.5% at the next 4-week study showed a decrease in spasticity by 1 point or higher on the Ashford scale [4]. The aim of our study is to improve the results of patients with complicated herniated discs of the cervical region using advanced cylindrical cages and transcranial magnetic stimulation in the early period after the removal of herniated discs.
2. Material and Methods
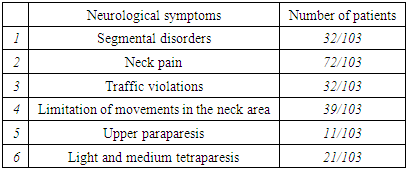
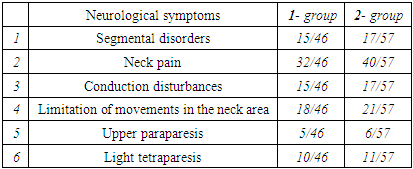
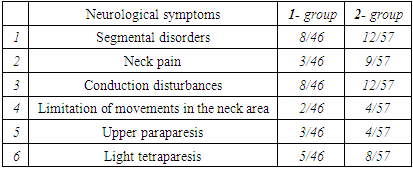
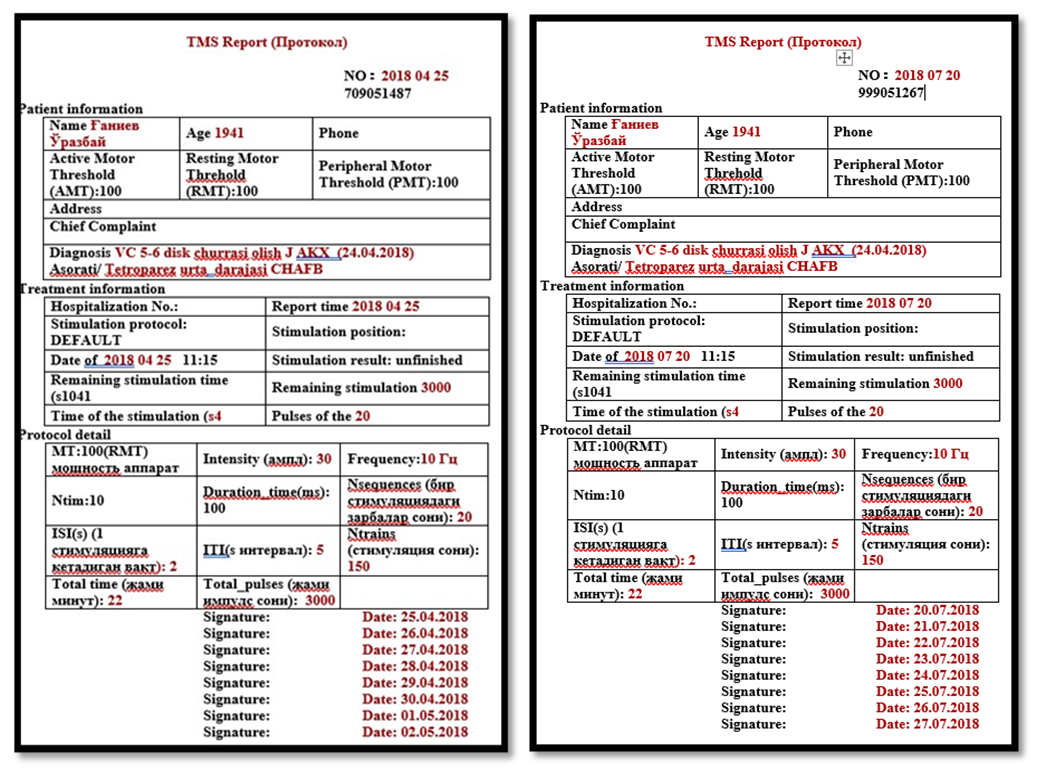
- The study was based on the analysis of 103 patients (70 (67.8%) men, 33(32.2%) women aged 24-83 years, average age – 55.1±0.68 years) with hernias of the cervical spine. All patients underwent surgery for cervical spine discectomy in the period 2018-2023 at the National Center for Rehabilitation and Prosthetics of Persons with Disabilities. The patients are divided into two groups. The first (main) group of 46 (44.6%) patients underwent "discectomy with decompression of the spinal cord, followed by stabilization with an improved cylindrical cage of the clinic and of these 15 (14.5%) patients using TMS stimulation in the early/long-term postoperative period." The second group of patients underwent discectomy, using cylindrical cages, corporectomy, stabilization with MESH and plates, and of these 17 (16.5%) patients received TMS stimulation.In the middle part of the cervical spine, in the VC 5-6 and VC6-7 segments, disc herniation is the most common. All patients underwent neurological examination, neuro-visual examination, EMS (European Myelopathic Scale) assessment, ENMG, functional radiography, Dopplerography as needed, as well as examinations by neurologists and related specialists before and after treatment. Clinical signs before the start of treatment. (before the operation, P<0.001, Ri=0.8).
|
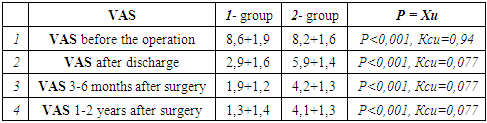
3. Results and Discussion
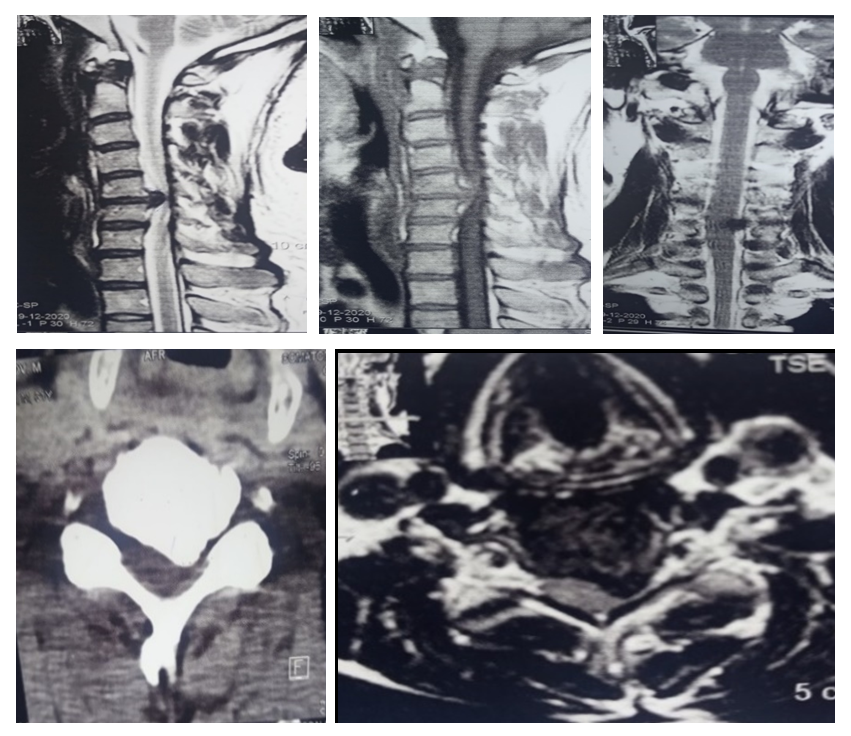
- The results of open surgical interventions were evaluated in two groups, according to the performed surgical intervention and the use of TMS. The first (main) group of 46 (44.6%) patients underwent "discectomy with decompression of the spinal cord, followed by stabilization with an improved cylindrical cage of the clinic and of these 15 (14.5%) patients using transcranial magnetic stimulation in the early/long-term postoperative period." The second group of patients underwent discectomy using cylindrical cages, corporectomy, stabilization with mesh and plates, stabilization with telescopic mesh, and of these 17 (16.5%) patients received TMS stimulation. Patients of the first group underwent left-sided anterior parapharyngeal surgery under the control of EOP under general intubating anesthesia.A clinical example. Patient R.S., 49 years old. Medical history No. 1784/1332. Hospitalized on 06/22/2018. I've been worried about it for 2 years now. Complaints: pain in the left arm, pain when moving the neck, dizziness, numbness of the fingers of the left hand, tingling (Lermitt's symptom is positive), slight weakness in the legs and arms. 13-14 points on the EMS scale. ENMG conclusion: Edema along the left radicular segment of the neck C6, signs of radiculomyelopathy with a compression-irradiation component. The final diagnosis: "Osteochondrosis of the cervical vertebrae. Herniated intervertebral disc L5-6. Secondary stenosis VC 5-6 of the spinal canal. Compression myelomalacia VC5-6. Mild tetraparesis. Partial violation of CHUBB."
 | Figure 2 |
 | Figure 5 |
|
|
|
4. Conclusions
- 1. After adequate decompression of the spinal cord by parapharyngeal access in hernias of the cervical spine, it is advisable to use an improved cylindrical cage of the clinic in order to stable stabilization of one or more segments. 2. The use of transcranial magnetic stimulation in the early postoperative and long-term periods for herniated discs of the cervical spine makes it possible to awaken and restore long-lost neurological deficits, lost muscle groups and, in some cases, entire organizations early. 3. The use of the clinic's advanced cylindrical cage for herniated discs of the cervical spine does not require the use of additional plates in cases of displacement and instability of the vertebrae, as well as in osteoporosis of the vertebrae, which increases economic efficiency for the patient and the hospital.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML