-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2795-2803
doi:10.5923/j.ajmms.20241411.26
Received: Oct. 9, 2024; Accepted: Nov. 9, 2024; Published: Nov. 12, 2024

Comprehensive Therapy of Children with Abdominal Obesity and Metabolic Syndrome Using Transcranial Physiotherapy
Garifulina Lilya Maratovna1, Bolotova Nina Viktorovna2
1Samarkand State Medical University, Samarkand, Uzbekistan
2Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia
Correspondence to: Garifulina Lilya Maratovna, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

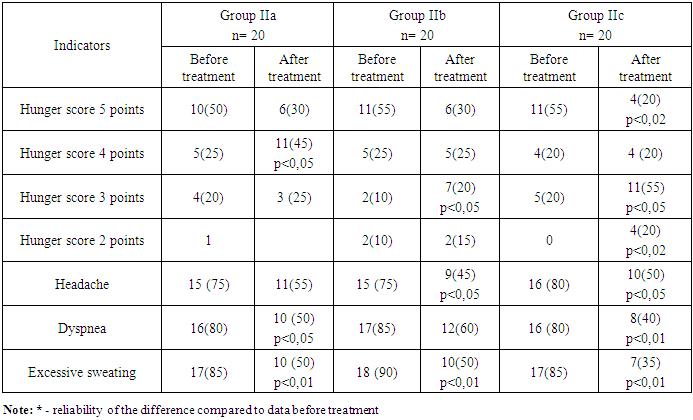
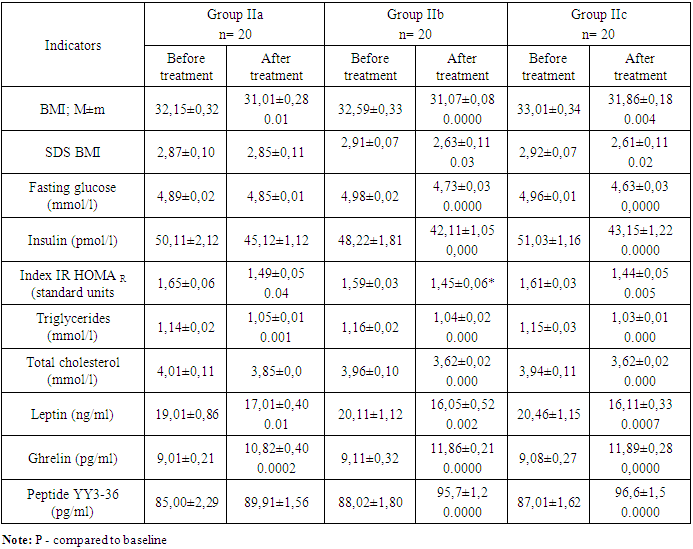
Introduction. Despite diet, work with a psychologist, lifestyle changes, most children with obesity have insufficient motivation to lose weight, which is accompanied by a short-term decrease in body weight. These facts contribute to the search for effective and safe treatment methods applicable to children. The aim of the study: to evaluate the effectiveness of the combined use of ά-lipoic acid, vitamin D, transcranial magnetic therapy and electrical stimulation in the treatment of children with abdominal obesity and manifestations of metabolic syndrome. Materials and methods: 128 children with abdominal and generalized obesity were studied, the state of carbohydrate and lipid metabolism, the level of vitamin D, leptin, ghrelin and peptide YY3-36 were determined. Various methods of therapy were used with the use of ά-lipoic acid, vitamin D, transcranial magnetic therapy and electrical stimulation. Results of the study: children with abdominal obesity and generalized obesity had significant pathology of carbohydrate and lipid metabolism with more severe manifestations in children with visceral obesity. Obesity in children is accompanied by a significant increase in basal leptin production, a decrease in fasting ghrelin secretion and peptide YY3-36, while the degree of pathology of these indicators depended on the type of obesity. The frequency of MS in children with abdominal obesity was 54.5%, while all children had vitamin D deficiency. Conclusion: When using ά-lipoic acid, vitamin D, transcranial magnetic therapy and electrical stimulation against the background of motivational training for weight loss, positive dynamics are determined in reducing eating behavior, biochemical parameters, levels of anorexigenic and orexigenic hormones in the following group of studies.
Keywords: Children, Abdominal obesity, Metabolic syndrome, ά-lipoic acid, vitamin D, Transcranial magnetic therapy, Electrical stimulation
Cite this paper: Garifulina Lilya Maratovna, Bolotova Nina Viktorovna, Comprehensive Therapy of Children with Abdominal Obesity and Metabolic Syndrome Using Transcranial Physiotherapy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2795-2803. doi: 10.5923/j.ajmms.20241411.26.
1. Introduction
- According to the World Health Organization, obesity is a global problem of world society that deserves close attention. It is important that the obesity epidemic is spreading at an alarming rate among children [1,2,3].The development of obesity in childhood contributes to the development of a high risk of early manifestation of severe comorbid conditions with the formation of metabolic syndrome (MS), which is a factor in reducing life expectancy and contributes to premature mortality in adulthood [4,5,6]. In this regard, the prevention and treatment of obesity and its complications are of great clinical importance and social significance.Successful treatment of obesity and its complications in children is possible only with complex and long-term therapy aimed at changing the lifestyle of the child and his family members, changing the diet, promoting physical activity, as well as psychological assistance that helps prevent or treat eating disorders [6,7,8].Despite diet, work with a psychologist, lifestyle changes, most children with obesity have insufficient motivation to lose weight, which is accompanied by a short-term decrease in body weight. These facts contribute to the search for effective and safe treatment methods applicable to children.Such methods of therapy include the use of alpha lipoic acid, which has a good therapeutic effect without disrupting homeostasis in the body, normalizing metabolic processes, this is especially important to consider in childhood. The hypoglycemic effect of alpha lipoic acid is known with an increase in tissue sensitivity to insulin, and intracellular glucose transport and, as a result, insulin resistance decreases. α-lipoic acid also reduces the formation of cholesterol and its atherogenic fractions [9,10,11].Thus, alpha lipoic acid influences all factors that determine the overall risk of developing carbohydrate and lipid metabolism disorders that form metabolic syndrome.Literary data indicate that the use of only traditional therapy in children with manifestations of MS is insufficient, in connection with which the method of physiotherapeutic transcerebral influence was used.The impact on central regulatory mechanisms is an important component in the treatment of obesity. Correction of the mechanisms of the hypothalamic-pituitary-endocrine gland system by pharmaceutical means is practically impossible, since the blood-brain barrier prevents the action of drugs. This contributed to drawing attention to physiotherapeutic approaches that affect the structures of the brain. Among physical factors, the best is the magnetic field: it easily penetrates tissues, does not have a warming effect, is a natural factor, has vasodilatory, antispasmodic, hypotensive, anti-edematous, neurotrophic and immunomodulatory properties [6,13,14]. Complex treatment of patients with adolescent hypothalamic syndrome using transcranial magnetic therapy (TcMT) has achieved significant positive results. Recently, combined physiotherapeutic methods with a unidirectional effect have been considered more effective. From this point of view, it is recommended to combine TcMT with transcranial electrical stimulation (TES), the main effect of which is to increase endogenous opioids, especially endorphins, in the blood, which can make it easier for the patient to change his or her eating behavior.The relevance of the problem of prescribing increased doses of vitamin D to children with concomitant pathology in the form of obesity and overweight in children is still being discussed in many countries to this day [15].In children and adolescents with obesity, the use of vitamin D to initiate weight loss gives very contradictory results, but its use has been proven to reduce the risk of negative consequences of excess weight [16]. A consensus has been reached regarding the need for mandatory administration of vitamin D preparations in children and adolescents with obesity, but there are no generalized standards for daily dosage and duration of therapy [17].Taking into account the above data, we set the following research objective: to evaluate the effectiveness of the complex use of ά-lipoic acid, vitamin D, transcranial magnetic therapy and electrical stimulation in the treatment of children with abdominal obesity and manifestations of metabolic syndrome.
2. Material and Methods
- The studies were conducted at family clinics in the city of Samarkand, as well as Samarkand regional branch of the Republican specialized endocrinology scientific and practical medical center named after academician E.H. Turakulov (Uzbekistan).The study involved 128 children aged 8 to 18 years with exogenous-constitutional obesity, with an average age of 12.11±0.61 years. The control group consisted of 40 children of the same age (12.19±0.18) with body weight having normal indicators, all children had no chronic diseases and acute diseases at the time of examination.Anthropometric studies were conducted using standard measuring devices. Anthropometric measurements include height, weight, waist and hip circumference. Comparison of the obtained data and assessment of physical development were performed using WHO age and gender distribution centile charts of height and weight for children aged 5-19 years [18]. Body mass index (BMI) was calculated using the generally accepted formula.At the initial examination stage, anthropometric studies were conducted and assessed using standard deviations of the body mass index (SDS) in accordance with the recommendations of the World Health Organization (WHO) [18]. The basis for establishing the diagnosis of obesity was the determination of the intersection point of age and BMI above +2.0 SDS BMI [1].In accordance with the set objectives, the children of the main group were divided into 2 main groups: Group 1 - 60 children with abdominal obesity, had a BMI of +2.0 to ≥+3 SDS (obesity from I-III degree). Waist circumference in this group exceeded the 90th percentile for the corresponding age and gender. The average BMI in children of this group (32.89±0.61 kg/m2) significantly exceeded the indicators of the control group (p<0.001).Group 2 - 68 children with a generalized type of obesity, also included patients with a BMI of +2.0 to ≥+3 SDS, (obesity group I-III) but with WV within the normal range according to percentile deviations according to age and gender. On average, BMI was 31.99±0.45 kg/m2.The control group consisted of 40 children of the same age (on average 12.00±0.21 years) with normal body weight of 19.36±0.28 kg/m2 (BMI less than +1 SDS for a given gender and age).All children in the main sample had their WV and HV determined, with subsequent determination of the WV/HV ratio, which served as an objective indicator of the presence or absence of abdominal obesity. WV was correlated with the WV percentile tables for gender and age, and abdominal obesity was diagnosed with WV values corresponding to the 90th percentile and above for a given age and gender [19]. For children aged 16 years and above, the criterion was WV ≥ 94 cm for boys and ≥ 80 cm for girls.The results showed that in children with abdominal obesity, the WV was within 102.12±1.52 cm, which was significantly higher compared to the control group 65.54±0.80 cm (p<0.001), and children with generalized obesity 81.32±0.15 (p<0.001). At the same time, the HV in children with abdominal obesity was (86.11±2.11 cm) and did not differ from the indicators of children in the control group (78.23±1.22 cm; p>0.05). The WV/HV ratio characterizing the presence of abdominal obesity averaged 1.02±0.01 cm (p<0.001 compared to the control and comparison group) and in children with a generalized type of obesity 0.92±0.00 cm (p<0.001), in the control 0.79±0.01 cm.Blood pressure was measured using the Korotkov method, using cuffs of different lengths, corresponding to the circumference of the children's arm. To diagnose AH in obese children, special tables were used, based on the results of studies of the population of children, taking into account the age, sex and height of the child [19].Plasma glucose level was estimated by glucose oxidase method using GLUCL reagent kit for Abbott Architect 8000 analyzer. Serum insulin level was estimated using enzyme immunoassay method, reagent kit and calibrators manufactured by Roche Diagnostics ELECSYS Insulin. (Germany) for Cobas e411 analyzer. Standard oral glucose tolerance test (OGT, glucose load 1.75 g/kg, no more than 75 g) was performed with measurement of fasting glucose level (glucose 0') and 120 minutes after glucose load (glucose 120'). Insulin resistance index (HOMA-IR) was calculated by the formula: fasting insulin (pmol/l) × fasting glucose (mmol/l)/155. Values less than 3.2 were taken as normative HOMAR index.The lipid profile was studied on an automatic biochemical analyzer Cobas Integra 400 plus (Roche, Germany) using original test systems (Roche, Germany) with the determination of concentrations of total triglycerides, high-density lipoprotein cholesterol by absorption photometry.Determination of leptin, ghrelin and YY3-36 was carried out by the enzyme immunoassay method on the HumaReader HS device, using the Human LEPTIN ELISA Kit, Human GHRL (Grelin) ELISA Kit, ELISA DSL-10-33600 test systems (manufactured by Elabscience USA).Transcranial magnetic therapy (TMT) and transcranial electrical stimulation (TES) were used using the AMO-ATOS-E device (LLC Trima, Saratov; registration certificate № FSR 2009/04781). Considering that physical impact is better absorbed by the body if its frequency parameters are close to the frequencies of the functioning of the main body systems, magnetotherapy with a running magnetic field was carried out in the scanning frequency range of 1–12 Hz. Sessions with the “Headband” attachment were carried out with the patient in a sitting position. Induction on the surface of the emitter was 20–45 mT (depending on age). Impact with a running magnetic field was carried out from the temporal lobe to the occipital lobe synchronously on both hemispheres of the brain for 7–12 min. The modulation frequency and exposure time were gradually increased with each procedure, starting with the minimum values. In the last sessions, the regular scanning mode was replaced by the “Stochas” mode. TES was carried out with an output voltage of 15–20 V and an average current of no more than 25 mA. Pulse packs followed with a frequency of 50–80 Hz. The course of treatment consisted of 15 daily procedures [13].As part of the complex therapy of children with manifestations of MS, α-lipoic acid was used at 100 mg 3 times a day for children under 14 years old, 200 mg 3 times a day for children over 14 years old for 1 month. Cholecalciferol was used in a dosage in accordance with the SDS of the BMI. In children with a BMI of +1.0 to +2.0 SDS, vitamin D was used at a daily dose of 2000 U/day, BMI >+2<+3 SDS at a daily dose of 3000 U/day and in children with a BMI ≥+3 SDS at a dose of 4000 U/day for 3 months.Statistical processing of the obtained data was carried out on a personal computer using the Statistica 10 program. The methods of variational parametric and nonparametric statistics were used with the determination of the arithmetic mean (M), standard deviation (σ), standard error of the mean (m), relative values (frequency, %). The statistical significance of the obtained measurements was determined by the Student criterion (t) with the calculation of the probability of error (P). Correlation analysis by the Pearson method (r).
3. Results and Their Discussion
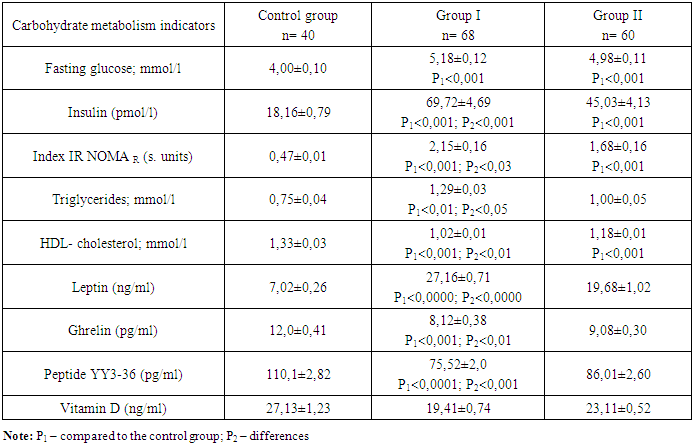
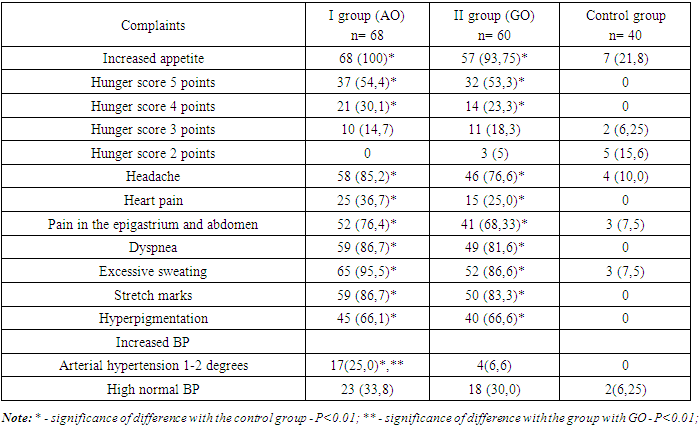
- The metabolic status of children was identified by determining the level of carbohydrate and lipid metabolism. Comparative characteristics of the average level of the obtained result showed that children with abdominal obesity had the highest pathological results compared to children with a generalized type of obesity. At the same time, the average results of the metabolic indicators did not go beyond the reference limits (Table 1).
|
|
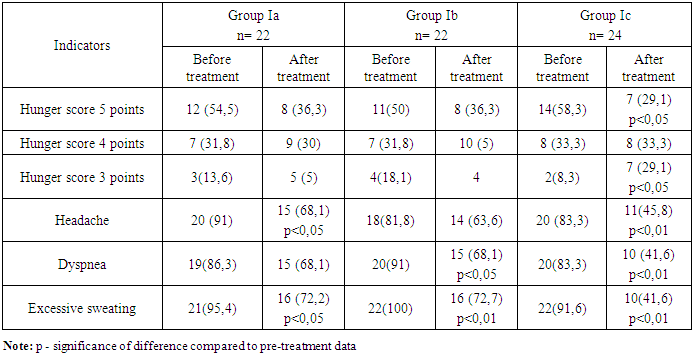
|
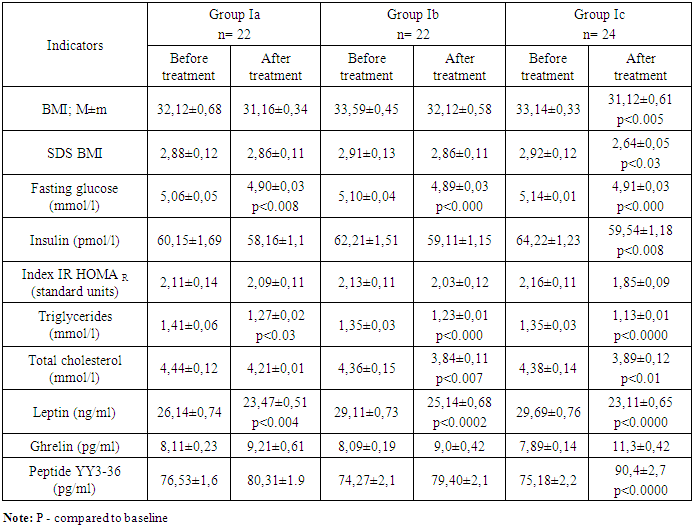
|
|
|
4. Conclusions
- In children with abdominal obesity and generalized obesity, significant pathology of carbohydrate and lipid metabolism was observed, with more severe manifestations in children with visceral obesity.Obesity in children is accompanied by a significant increase in basal leptin production, a decrease in fasting ghrelin secretion and peptide YY3-36, while the degree of pathology of these indicators depended on the type of obesity.The frequency of MS in children with abdominal obesity was 54.5%, with AO+4 components diagnosed in 19.11%, AO+3 components diagnosed in 20.58%, and the frequency of incomplete MS in the form of AO+2 components diagnosed in 14.7% of children with abdominal obesity.In children with obesity, statistically significant pathology of vitamin D metabolism was observed, characterized by cases of deficiency of 76.5% and cholecalciferol insufficiency of 46.7% in children with abdominal obesity compared to children with a generalized type of obesity.Children with various types of obesity have significant disturbances in the nature of nutrition, accompanied by a strong, uncontrollable feeling of hunger with the consumption of a large volume of food.The proposed combination treatment, including transcranial magnetic therapy and electrical stimulation against the background of motivational training on weight loss and the use of ά-lipoic acid, and differentiated prescription of vitamin D depending on the degree of obesity, contributed to a decrease in body weight in children with and was accompanied by correction of eating behavior, positive dynamics in the level of fasting glucose, insulin, blood, triglycerides, as well as anorexigenic and orexigenic hormones, regardless of the type of obesity.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML