-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2785-2790
doi:10.5923/j.ajmms.20241411.24
Received: Sep. 19, 2024; Accepted: Oct. 16, 2024; Published: Nov. 12, 2024

Current Approaches to Treatment the Patients with Widespread Purulent Peritonitis
Sattarov Shokir Khasanovich1, 2, Ruzibaev Sanjar Abdusalomovich2, Rakhmanov Kosim Erdanovich2, Davlatov Salim Sulaymonovich3
1Samarkand Branch of the Republican Scientific Center for Emergency Medical Care, Uzbekistan
2Samarkand State Medical University, Uzbekistan
3Bukhara State Medical Institute named after Abu Ali ibn Sino, Uzbekistan
Correspondence to: Sattarov Shokir Khasanovich, Samarkand Branch of the Republican Scientific Center for Emergency Medical Care, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background. Treatment of disseminated peritonitis is one of the most complex and intractable problems of emergency abdominal surgery. Disseminated purulent peritonitis is a severe variant of complicated intra-abdominal infection and is a life-threatening complication of most acute surgical diseases of abdominal cavity. Objectives. To improve the results of surgical treatment of disseminated purulent peritonitis on the basis of a differentiated approach to the choice of treatment depending on the degree of abdominal sepsis. Materials and methods. The study is based on the results of treatment of 276 patients with widespread purulent peritonitis admitted to the surgical department of the Samarkand branch of RCEMP in the period from 2015 to 2024. Patients were conditionally divided into two groups: 132 (47.8%) patients were operated on in 2015-2019, who were included in the comparison group, and 144 (52.2%) patients were operated on from 2020 to 2024, who were included in the main group. Results. A study of the results of combination therapy using ozonated 0.03% sodium hypochlorite solution for abdominal cavity sanitation and intravenous management in patients with abdominal sepsis showed encouraging results. There was a marked decrease in the rate of postoperative purulent inflammatory complications from 32.4% to 16.7% in SIRS - 0 and SIRS abdominal sepsis (p<0.05), and from 51.5% to 41.4% and from 70.6% to 36.0% in SIRS - 1 and SIRS - 2 abdominal sepsis (p<0.05), respectively. Fatal outcome decreased from 15.1% to 4.9% and from 41.2% to 20.0% in abdominal sepsis SIRS - 1 and SIRS - 2 (p<0.05), respectively. Conclusions. Complex application of ozonized sodium hypochlorite solution in the postoperative period contributes to faster recovery of patients, decreased incidence of complications and improved overall clinical results.
Keywords: Peritonitis, Ozone, Sodium hypochlorite solution, Treatment
Cite this paper: Sattarov Shokir Khasanovich, Ruzibaev Sanjar Abdusalomovich, Rakhmanov Kosim Erdanovich, Davlatov Salim Sulaymonovich, Current Approaches to Treatment the Patients with Widespread Purulent Peritonitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2785-2790. doi: 10.5923/j.ajmms.20241411.24.
Article Outline
1. Introduction
- Treatment of disseminated peritonitis is one of the most complex and intractable problems of emergency abdominal surgery. Disseminated purulent peritonitis (DPP) is a severe variant of complicated intra-abdominal infection and is a life-threatening complication of most acute surgical diseases of abdominal cavity [1,2,3]. Despite all the achievements of clinical medicine, this pathology is accompanied by inexorably high figures of postoperative complications and mortality without a tendency to decrease over the last few decades. Postoperative mortality in widespread peritonitis is 15.1-18%, and when septic shock develops, the mortality reaches 70-80% [4,5,6,7]. In the light of the above, the need to improve the known and develop new effective measures of prevention and treatment of this formidable disease becomes obvious.Analysis of modern literature shows that there are several directions in the treatment of DPP: traditional surgical interventions, videolaparoscopic interventions. “However, the most accessible direction in everyday practice remains open surgical interventions for widespread purulent peritonitis” [8,9,10,11].The analysis of the literature shows that at the present time the therapeutic and diagnostic tactics in DPP P is one of the urgent and unresolved problems of modern healthcare [12,13,14]. In this regard, there is a necessity to revise the sanation interventions in DPP depending on the informativeness of non-invasive methods of medical imaging, which allow preoperatively to assess the character of exudate and to detect signs of disease aggression, in this connection, the optimization of diagnostic algorithm to choose the most complete tactics of surgical treatment in each specific case becomes especially urgent.Despite a lot of ongoing studies and seemingly solved problems, the development of modern methods of treatment of widespread peritonitis and, first of all, the use of laparoscopic surgery, has led to a lot of new unexplored issues, the need to solve which confirms the relevance of the present research topic.
2. The Purpose of Study
- To improve the results of surgical treatment of disseminated purulent peritonitis on the basis of a differentiated approach to the choice of treatment depending on the degree of abdominal sepsis.
3. Materials and Methods
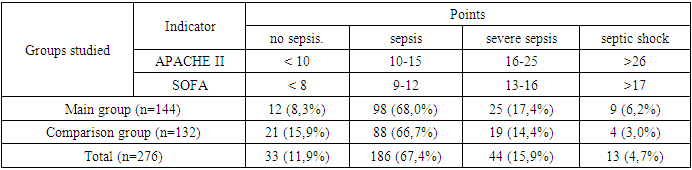
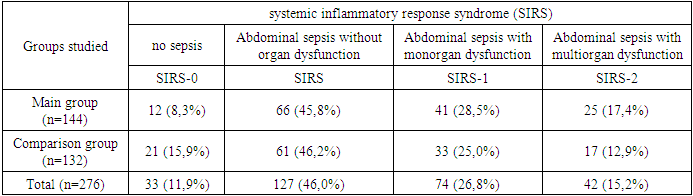
- The study is based on the results of treatment of 276 patients with widespread purulent peritonitis admitted to the surgical department of the Samarkand branch of RCEMP in the period from 2015 to 2024. Patients were conditionally divided into two groups: In 2015-2019, 132 (47.8%) patients who constituted the comparison group were operated on, they underwent traditional methods of treatment, elimination of the source, sanation of the abdominal cavity with antiseptics and drainage of the abdominal cavity by both open and laparoscopic methods. From 2020 to 2024, 144 (52.2%) patients were under our observation and were included in the main group. Depending on the severity of peritonitis stage, the patients of the main group were conditionally divided into two subgroups. The 1st subgroup consisted of 78 (54,2% out of 144) patients, they used ozonized sodium hypochlorite solution as an antiseptic for the purpose of abdominal cavity lavage. Subgroup 2 consisted of 66 (45.8% out of 144) patients, in this subgroup patients with severe form of abdominal sepsis, who required intravenous injection of ozonated sodium hypochlorite solution in addition to abdominal cavity lavage with ozonated sodium hypochlorite solution.Disseminated purulent peritonitis was of different genesis. The most frequent cause of peritonitis in both groups of patients was destructive forms of acute appendicitis (38.8%) and perforated gastric and duodenal ulcer (22.1%). Preoperatively, the severity of the patients' condition was determined according to the APACHE II scale, SOFA and the severity of abdominal sepsis. The indicators of preoperative examination of patients are presented in Tables 1. Both groups were comparable in terms of the severity of the condition and severity of peritonitis.
|
|
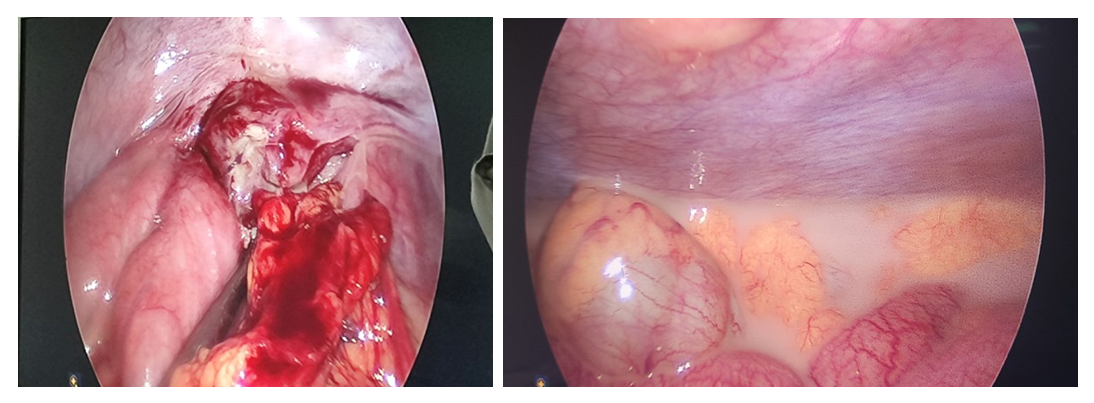 | Figure 1. Diagnostic laparoscopy in spilt purulent peritonitis |
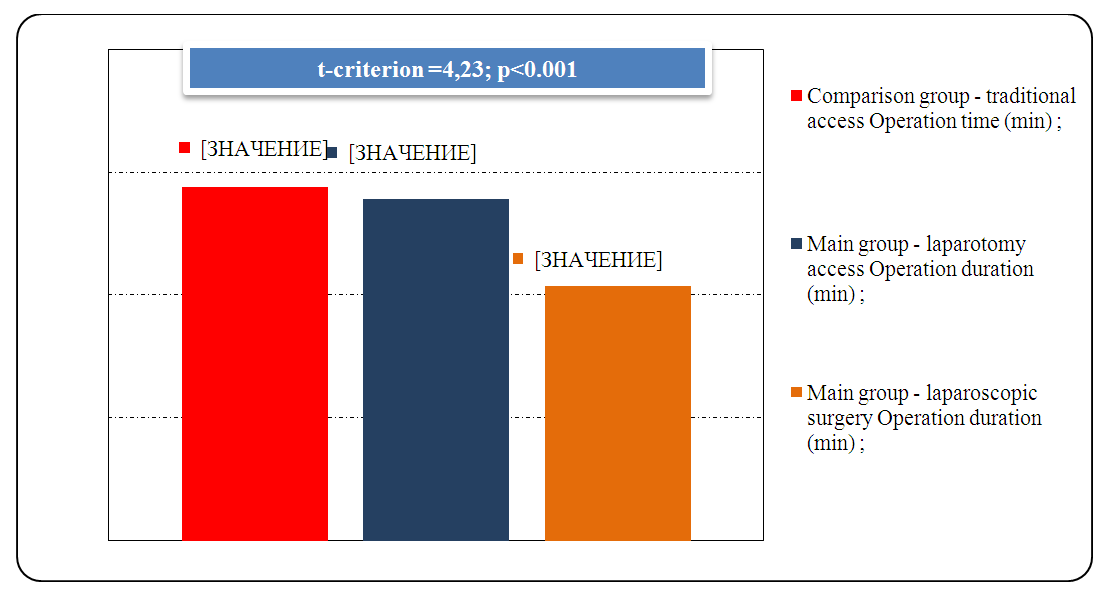 | Figure 2. Comparative indices of operation duration (min) depending on the access undertaken |
4. Results of the Study
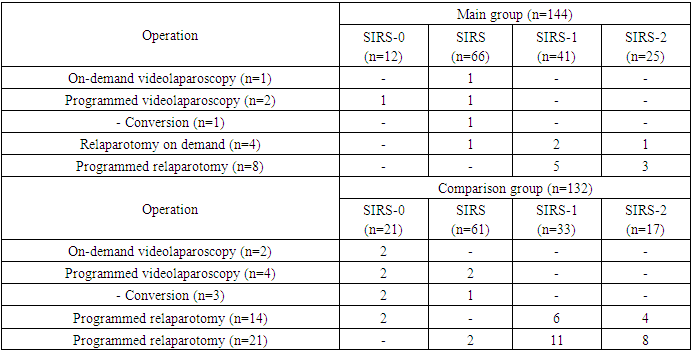
- In case of disseminated purulent peritonitis, 5 (3.5%) patients with abdominal sepsis underwent repeated interventions on demand in the main group. In the comparison group, 16 (12.1%) patients with abdominal sepsis underwent repeated interventions on demand (Table 3).
|
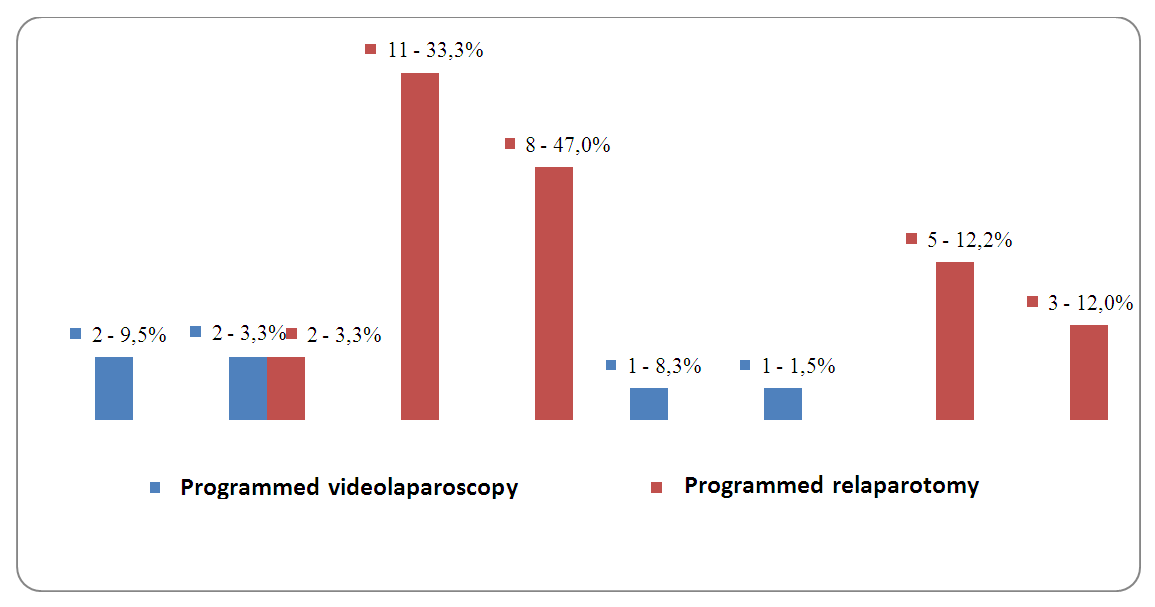 | Figure 3. Number of programmed sanitary surgical interventions |
|
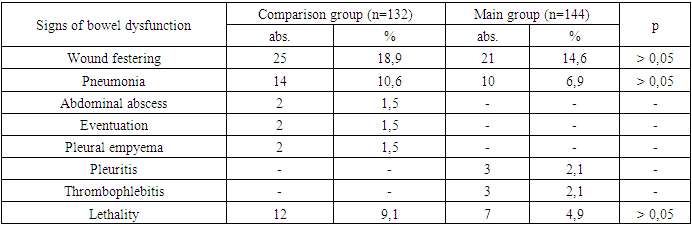
5. Funding
- A study of the results of combination therapy using ozonated 0.03% sodium hypochlorite solution for abdominal cavity sanitation and intravenous management in patients with abdominal sepsis showed encouraging results. There was a marked reduction in the rate of postoperative purulent inflammatory complications from 32.4% to 16.7% in SIRS - 0 and SIRS abdominal sepsis (p<0.05), and from 51.5% to 41.4% and from 70.6% to 36.0% in SIRS - 1 and SIRS - 2 abdominal sepsis (p<0.05), respectively. In addition, there was a reduction in the mean duration of hospitalization from 12.9 days to 10.1 days for abdominal sepsis SIRS - 0 and SIRS (p<0.05) and from 21.1 days to 16.6 days for abdominal sepsis SIRS - 1 and SIRS - 2 (p<0.05). Lethality decreased from 15.1% to 4.9% and from 41.2% to 20.0% in abdominal sepsis SIRS - 1 and SIRS - 2 (p<0.05), respectively.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML