-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2777-2780
doi:10.5923/j.ajmms.20241411.22
Received: Sep. 18, 2024; Accepted: Oct. 14, 2024; Published: Nov. 12, 2024

Effectiveness of Videolaparoscopic Correction of Reflux Gastritis in Patients with Postcholecystectomic Syndrome
Mardonov Bobosher Amirovich1, Kurbaniyazov Zafar Babajanovich1, Rakhmanov Kosim Erdanovich1, Davlatov Salim Sulaymonovich2
1Department Surgical Diseases №1 and Transplantology, Samarkand State Medical University, Samarkand, Uzbekistan
2Department of Faculty and Hospital Surgery. Bukhara State Medical Institute named after Abu Ali ibn Sino. Bukhara, Uzbekistan
Correspondence to: Davlatov Salim Sulaymonovich, Department of Faculty and Hospital Surgery. Bukhara State Medical Institute named after Abu Ali ibn Sino. Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. Gallstone disease (GSD) is one of the most common pathologies of the gastrointestinal tract, affecting 10-30% of the working age population. Over the past two decades, laparoscopic cholecystectomy (LCE) has become the “gold standard” for surgical treatment of cholelithiasis due to its minimal morbidity, reduction in hospitalization and rehabilitation. The aim of the study was to study the effectiveness of videolaparoscopic correction of reflux gastritis in patients with postcholecystectomy syndrome. Materials and methods. The study is based on an analysis of clinical data from 80 patients treated in the surgical department from 2017 to 2023. To determine the incidence of postcholecystectomy reflux gastritis (PCE RG), the total number of patients diagnosed with gallstone disease (GSD) admitted during this period was determined - 571 people (100%). Of these, 160 patients (27.8%) presented with symptoms of postcholecystectomy syndrome (PCES), while 48 (45.7%) of them were diagnosed with RG, and 50 patients (17%) required exclusively surgical correction. The results and discussion. In patients with postcholecystectomy syndrome, reflux gastritis (RG) of varying severity occurred in 45.9% of cases after cholecystectomy (CE) performed open or laparoscopically. Of these, 17% of patients with RG required only surgical correction. In 24% of cases, the cause of the development of RG was insufficiency of the pyloric sphincter, and in 76% - a chronic disorder of duodenal patency (functional or organic in nature). Conclusion. Thus, the method of video laparoscopic anti-reflux intervention in patients with PCES, developed and improved by us, is highly effective, which allows improving both immediate and long-term results of operations.
Keywords: Postcholecystectomy syndrome, Postcholecystectomy reflux gastritis, Gallstone disease
Cite this paper: Mardonov Bobosher Amirovich, Kurbaniyazov Zafar Babajanovich, Rakhmanov Kosim Erdanovich, Davlatov Salim Sulaymonovich, Effectiveness of Videolaparoscopic Correction of Reflux Gastritis in Patients with Postcholecystectomic Syndrome, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2777-2780. doi: 10.5923/j.ajmms.20241411.22.
Article Outline
1. Introduction
- Gallstone disease (GSD) is one of the most common pathologies of the gastrointestinal tract, affecting 10-30% of the working age population. Over the past two decades, laparoscopic cholecystectomy (LCE) has become the “gold standard” for surgical treatment of cholelithiasis due to its minimal morbidity, reduction in hospitalization and rehabilitation [1,3,7]. However, the quality of life of patients after surgery remains an important criterion for the effectiveness of LCE. 25 years after the introduction of LCE into surgical practice, it remains clear that surgery does not always eliminate the complex pathophysiological changes caused by cholelithiasis. Properly performed cholecystectomy prevents the need for repeated operations, but does not exclude ongoing or periodic drug therapy [2,5,9,11].Unfortunately, removing the gallbladder does not always solve all the patient’s problems. Some patients continue to experience pain and dyspepsia, known as postcholecystectomy syndrome (PCES). The problem of treating cholelithiasis remains relevant, despite many studies and publications. In the postoperative period, 8-87% of patients experience pain and dyspeptic disorders [5,10]. The development of PCES is promoted not only by the pathology of the common bile duct and the major duodenal papilla, but also by insufficient diagnosis of motor-evacuation disorders of the stomach and duodenum in patients with cholelithiasis [3,6,11].Diagnosis and treatment of PCES is a pressing problem for physicians, gastroenterologists and surgeons. Surgeons believe that postoperative complaints are caused by insufficient preoperative examination and correction. 30% of patients with PCES require repeated surgical interventions. One of the key reasons for PCES is untimely diagnosis and correction of reflux gastritis, which in the long-term postoperative period is complicated by postcholecystectomy reflux gastritis [4,8,9]. An analysis of the existing literature shows a lack of research on the prevention and treatment of postcholecystectomy reflux gastritis [5,7].In this regard, the development of new methods for surgical correction and prevention of postcholecystectomy reflux gastritis is the basis for this study.
2. The aim of the Study
- The aim of the study was to study the effectiveness of videolaparoscopic correction of reflux gastritis in patients with postcholecystectomy syndrome.
3. Materials and Methods
- The study is based on an analysis of clinical data from 80 patients treated in the surgical department from 2017 to 2023. To determine the incidence of postcholecystectomy reflux gastritis (PCE RG), the total number of patients diagnosed with gallstone disease (GSD) admitted during this period was determined - 571 people (100%). Of these, 160 patients (27.8%) presented with symptoms of postcholecystectomy syndrome (PCES), while 48 (45.7%) of them were diagnosed with RG, and 50 patients (17%) required exclusively surgical correction.Patients (n=80) were divided into three groups: two main and one control. The first group (n=35) included patients with PCE RG who underwent laparoscopic or traditional surgery with correction of RG. The second group included 17 patients with cholelithiasis and RG, who underwent prophylactic correction of RG during cholecystectomy (CE) to prevent the development of PCE RG. The control group (n=28) consisted of patients with PCES, for whom a retrospective analysis of medical records was carried out to determine the reasons for the development of PCES RG.Among patients with PCE RG, 9 (25%) were men and 26 (75%) women, ages ranged from 36 to 75 years. The majority of patients with PCE RG were of working age (from 37 to 50 years) and accounted for 66% (n=23). Patients of the first group were previously operated on for cholelithiasis and were hospitalized at various times after cholecystectomy.After a survey of patients in the first group, it turned out that 58% of them did not notice any improvement in their health after cholecystectomy (CE). These patients continued to experience periodic pain, mainly in the epigastric region, heartburn, nausea, sometimes progressing to vomiting. The remaining 42% initially felt better, but over time the condition worsened and the disease began to progress. All patients repeatedly turned to various specialists or self-medicated, which brought only short-term relief.Upon admission to the clinic, the main complaints of patients were pain, which was observed in 87% (n=31) of patients. Of these, 82% (n=29) complained of pain in the epigastric region, 16% (n=8) of pain in the left hypochondrium, and 30% (n=15) of pain in the right hypochondrium. A small proportion of patients also complained of nausea (76%, n=27), heartburn (48%, n=17), belching (36%, n=13), vomiting (22%, n=11) and bitter taste in the mouth (25%, n=9). Complaints of decreased appetite, general weakness and fatigue were present in all examined patients.After a comprehensive examination, it was found that the main cause of the development of reflux gastritis (RG) is insufficiency of the pyloric sphincter (24%, n=8) and duodenal obstruction (DO), both mechanical (65%, n=23) and functional (18%, n=6).Among the mechanical causes of DO were identified: proximal (n=2), distal (n=3) and total (n=5) periduodenitis, high fixation of the duodenojejunal junction (n=13), as well as arteriomesenteric compression (n=3) caused by compression of the ascending duodenum between the superior mesenteric artery and the aorta. Of the functional causes, the hypotonic form of DO was identified in 4 patients, and the hypertensive form - in 5 patients. It is important to note that in 4 patients with pyloric sphincter insufficiency, the mechanical form of DO was also diagnosed in the form of high fixation of the duodeno-jejunal junction.It should be noted that in patients of the first and second groups, a thorough examination revealed not only pathologies of the hepatopancreatobiliary system, but also diseases of other systems, complicating the course of the underlying disease. Pancreatitis was often diagnosed in both groups: in 13 patients of the first group and in 9 patients of the second group. Among the concomitant pathologies in the first group, choledocholithiasis and external abdominal hernias predominated, identified in 9 and 8 patients, respectively. Reflux esophagitis was also diagnosed in 7 patients, terminal common bile duct stenosis in 5, cardiovascular diseases in 6, liver cirrhosis in 1, diabetes mellitus in 3 and peptic ulcer in 2 patients. 8 (53.6%) patients had a combination of two or more of the listed diseases. In the second group, choledocholithiasis and stenosis of the terminal common bile duct were most often diagnosed (n=10).Patients were taken for surgery after a thorough preoperative examination and appropriate preparation. The nature and extent of the operation depended on the causes of the development of reflux gastritis (RG) and concomitant pathologies identified during the study, which are described in detail in the next section. It is important to emphasize that patients in the pre- and postoperative period received complex conservative treatment aimed at reducing inflammatory processes.All patients admitted to the clinic underwent a comprehensive clinical, laboratory and instrumental analysis. The patients' complaints were carefully studied and the medical history was carefully collected. Clinical examinations were performed, including general examination, abdominal examination, palpation, percussion and auscultation. Patients underwent a plain chest x-ray, an electrocardiogram (ECG), a consultation with a cardiologist, and an ultrasound examination of the abdominal organs. To diagnose reflux gastritis (RG), special research methods were used, such as Doppler ultrasound of the superior mesenteric artery (SMA), esophagogastroduodenoscopy (EFGDS), polypositional X-ray contrast study, floor-by-floor manometry, determination of bile acids in gastric juice, study of gastric secretion and acidity, diagnosis of helicobacteriosis and, if necessary, endoscopic retrograde cholangiopancreatography (ERCP). In cases where reflux gastritis (RG) occurred due to insufficiency of the pyloric sphincter along the anterior wall, functional chronic duodenal obstruction (CFDO) in the subcompensated stage, or mechanical CPDO caused by a high position of the duodeno-jejunal junction, preference was given to laparoscopic correction.Patients of the first and second groups, after preoperative preparation, underwent various operations, the type of which depended on the identified causes of RG. The operations were aimed at correcting the detected pathology. In addition to eliminating RG, other identified pathologies requiring surgical intervention were also corrected. After establishing the final diagnosis, we sought to perform correction of RG using minimally invasive methods.To achieve better results in the surgical treatment of RG, various correction methods were used, some of which were improved.Five patients with a combination of RG, choledocholithiasis and stenosis of the terminal common bile duct underwent endoscopic papillosphincterotomy (EPST) with stone extraction at the first stage, and correction of RG at the second stage. Two days after the first stage, closed laparoscopic pyloroplasty and laparoscopic dissection of the Treitz ligament with reduction of the duodenojejunal junction were performed (Fig. 1).
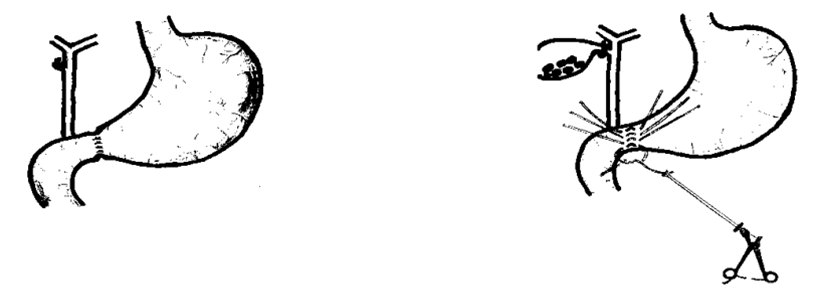 | Figure 1. Process of performing closed laparoscopic pyloroplasty (A). General view after surgery (B) |
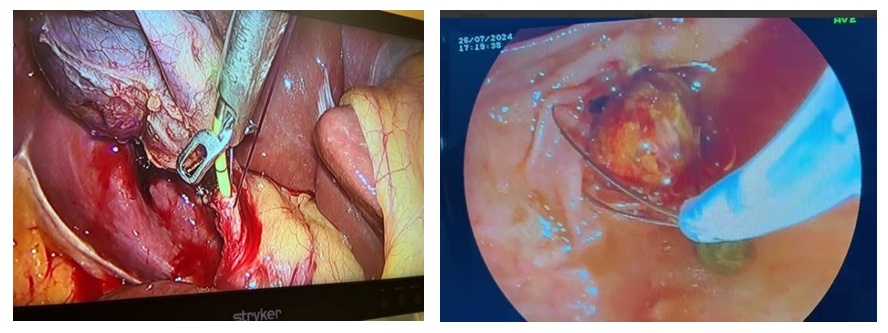 | Figure 2. EPST with lithoextraction of stones using a Dormia basket in combination with endovideosurgical cholecystectomy and dissection of the ligament of Treitz |
4. The Results and Discussion
- In patients with postcholecystectomy syndrome, reflux gastritis (RG) of varying severity occurred in 45.9% of cases after cholecystectomy (CE) performed open or laparoscopically. Of these, 17% of patients with RG required only surgical correction. In 24% of cases, the cause of the development of RG was insufficiency of the pyloric sphincter, and in 76% - a chronic disorder of duodenal patency (functional or organic in nature).The immediate causes of postcholecystectomy reflux gastritis are incomplete examination of patients with cholelithiasis during initial treatment and hospitalization, lack of a rational method and access for performing cholecystectomy, refusal to conduct a full intraoperative examination of the stomach, duodenum and duodeno-jejunal junction in cholecystectomy, as well as the performance of CE by young specialists who do not have experience in performing combined operations for the correction of RG during CE. The use of methods such as ultrasound, fibroesophagogastroduodenoscopy in combination with X-ray examination using a contrast agent and floor manometry, as well as the study of gastric juice for the content of bile acids plays an important role in the diagnosis of RG.With videolaparoscopic correction of postcholecystectomy reflux gastritis, excellent and good results were obtained in 93.7% of patients, satisfactory – in 4.2%, unsatisfactory – in 2.1%.
5. Conclusions
- Thus, the method of video laparoscopic anti-reflux intervention in patients with PCES, developed and improved by us, is highly effective, which allows improving both immediate and long-term results of operations.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML