-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2751-2754
doi:10.5923/j.ajmms.20241411.16
Received: Oct. 5, 2024; Accepted: Nov. 1, 2024; Published: Nov. 7, 2024

Investigation of the C1431T Polymorphism of the PPARG Gene Among Patients with Type 2 Diabetes Mellitus
Khomidov Feruz Kasimovich
PhD, Independent Applicant, Bukhara State Medical Institute, Uzbekistan
Correspondence to: Khomidov Feruz Kasimovich, PhD, Independent Applicant, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article will address the issues of C1431T polymorphism of the PPARG gene among adult patients with type 2 diabetes mellitus. The purpose of the work is to study the polymorphism C1431T of the PPARG gene depending on some biochemical parameters. Material and methods. PCR analysis of the C1431T PPARG gene and the study of fasting glucose, glycated hemoglobin and vitamin D. Results. It has been shown that, in order to identify risk factors for type 2 diabetes mellitus and correct clinical and metabolic disorders, the study of gene polymorphism is an important aspect.
Keywords: Type 2 diabetes mellitus, Polymorphism C1431T of the PPARG gene, Glucose, Glycated hemoglobin, Vitamin D
Cite this paper: Khomidov Feruz Kasimovich, Investigation of the C1431T Polymorphism of the PPARG Gene Among Patients with Type 2 Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2751-2754. doi: 10.5923/j.ajmms.20241411.16.
1. Introduction
- The problem of excess weight and diabetes mellitus (DM) has become increasingly relevant to modern medicine due to the rising incidence worldwide. The specific conditions and lifestyle of people in the 21st century, associated with physical inactivity; consumption of foods high in carbohydrates, salt, fats, and synthetic additives; frequent stressful situations caused by the accelerated pace of life; bad habits, and many other factors form the basis for weight gain, the development of metabolic syndrome (MS), and type 2 diabetes (T2DM). Numerous genetic and environmental factors also play a significant role in the spread of this pathology. Today, DM is one of the most common non-communicable diseases after cardiovascular and oncological pathologies, leading to disability and often resulting in fatal outcomes. DM, often simply referred to as diabetes, is a serious chronic progressive disease characterized by elevated blood serum glucose levels (hyperglycemia), which is associated with various comorbid conditions, such as impaired vision, poor wound healing, erectile dysfunction, renal failure, heart disease, etc.T2DM is a heterogeneous disease that develops as a result of a combination of genetic and acquired factors. The predisposition to T2DM is primarily determined by an individual's genome, which may contain gene alleles that, under the influence of environmental factors, can trigger the development of the disease.A feature of T2DM is its potential prevention through prophylaxis. Another distinction in the development of T2DM is that the disease does not begin at the moment of detecting significant hyperglycemia but develops gradually [17].
2. Materials and Methods
- To identify the risk factors for T2DM, we examined the serum of 170 patients aged 18-90 years who were receiving treatment at the Republican Specialized Scientific and Practical Medical Center of Endocrinology named after Academician Y. Kh. Turakulov. The study focused on the polymorphisms of the PPARy gene genotype C1431T using the polymerase chain reaction method in real-time mode. All clinical and laboratory data (HbA1c values, glucose, clinical biochemical and genetic analyses, and information from questionnaires) were transferred to a unified database after completing the first stage of the study. Statistical analysis was performed using a standard data processing package.
3. Results and Discussion
- The main pathogenic mechanisms of T2DM development include insulin resistance, a secretory defect of β-cells, and hyperproduction of glucose by the liver. Numerous factors affect blood glucose levels, determining the functional activity and amount of glucose released into the blood throughout the day. The circadian regulation of glycemic homeostasis is determined by the degree of physical activity, dietary habits, the state of the psycho-emotional sphere, and more. According to researchers, prediabetes, impaired glucose tolerance, and other manifestations of carbohydrate metabolism disorders are independent risk factors for developing cardiovascular diseases. When carbohydrate metabolism disorders are detected early, these data can serve as a prognostic sign of the development of DM and cardiovascular pathology [5,15].In recent years, researchers have shown interest in using ligands of the nuclear receptor peroxisome proliferator-activated receptors (PPARs) in type 2 diabetes (T2DM) and metabolic syndrome, which contribute to the development of insulin resistance (IR). PPARs are nuclear transcription factors that directly affect genes involved in the development of metabolic syndrome. PPARs integrate signals from the external environment in the form of ligands, which interact with PPARs and induce a cellular response by activating specific genes. Ligands, or agonists of the main PPAR isoforms, can include fatty acids and their metabolites, prostaglandins, and certain medications. It has been proven that individuals with low PPAR activity tend to develop excess body weight, IR, T2DM, and vascular complications at a young age. Currently, three subtypes of nuclear PPAR receptors have been identified: α, β/σ, and γ. PPARα is involved in the uptake and oxidation of fatty acids, mainly in the liver and heart. PPARβ/σ is engaged in the oxidation of fatty acids in muscles. PPARγ is expressed in adipose tissue and is strongly associated with the development of IR [20,21]. Normally, PPARs are responsible for balancing the oxidation of fatty acids in hepatocytes (PPARα) and their accumulation in adipocytes (PPARγ), which determines the role of PPARs in the development of metabolic syndrome and their potential impact on the development of dyslipidemia [8].In this study, we investigated polymorphisms of the PPARγ gene genotype C1431T using the real-time polymerase chain reaction method and conducted a comparative analysis of patient data. Furthermore, the frequency of risk alleles in the genes of individuals with T2DM was compared with the frequency of this indicator in individuals from the Uzbek population.The PPARG gene encodes the PPARγ receptor, which is involved in controlling the expression of genes that regulate fatty acid metabolism. Mutations in the "functional" regions of the gene lead to increased glucose concentration in the blood, resulting in excess body weight and the development of diabetes [17].
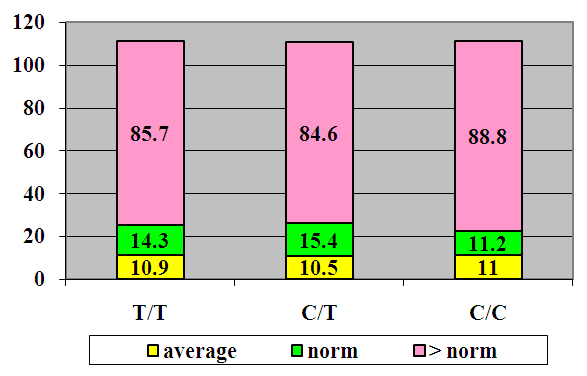 | Figure 1. Glucose Levels in Patients with Type 2 Diabetes (T2DM) |
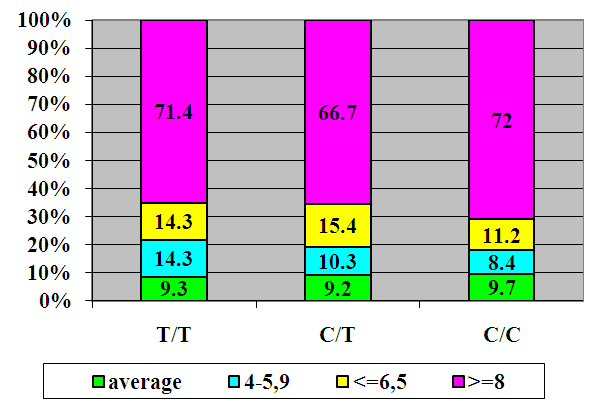 | Figure 2. HbA1c Levels |
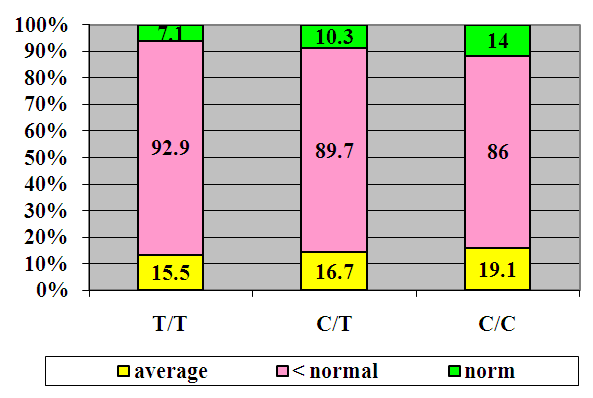 | Figure 3. Vitamin D Levels |
4. Conclusions
- Thus, the study of gene polymorphisms in patients with T2DM contributes to the early diagnosis of disease complications and the prevention of diabetes, which is very important for patients. However, these observations are ambiguous and require further research.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML