-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2748-2750
doi:10.5923/j.ajmms.20241411.15
Received: Oct. 19, 2024; Accepted: Nov. 5, 2024; Published: Nov. 7, 2024

The State of the Sympatho-Adrenal System in Patients with Ischemic Heart Disease in Combination with Chronic Obstructive Pulmonary Disease
Mamathuzhaev Zohidbek Sadirdin Ugli, Khuzhamberdiev Mamazair Akhmedovich, Uzbekova Nelly Rafikovna
Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Mamathuzhaev Zohidbek Sadirdin Ugli, Andijan State Medical Institute, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

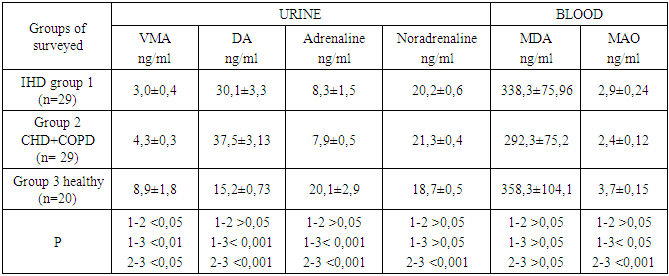
The article presents a comparative analysis of the indicators of catecholamines (CA) - adrenaline, norepinephrine and dopamine, the metabolite – vanillylmindal acid (IUD) in daily urine, as well as malonic dealdehyde (MDA) and the enzyme oxidative deamination of KA - monoamine oxidase (MAO) in serum in patients with coronary heart disease and coronary heart disease in combination with chronic obstructive pulmonary disease. The results showed significant violations of the sympathoadrenal system function, namely: a decrease in the level of adrenaline, an increase in the level of norepinephrine and dopamine, which indicates a violation of the activity of the sympathoadrenal system in this category of patients. In IHD, as well as in combination with IHD and COPD, there is a significant decrease in the activity of monoamine oxidase relative to the control group, which indicates a change in its catalytic properties.
Keywords: Sympatho-adrenal system, Catecholamines, Ischemic heart disease, Chronic obstructive pulmonary disease
Cite this paper: Mamathuzhaev Zohidbek Sadirdin Ugli, Khuzhamberdiev Mamazair Akhmedovich, Uzbekova Nelly Rafikovna, The State of the Sympatho-Adrenal System in Patients with Ischemic Heart Disease in Combination with Chronic Obstructive Pulmonary Disease, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2748-2750. doi: 10.5923/j.ajmms.20241411.15.
1. Introduction
- Cardiovascular pathology continues to be one of the most important problems of humanity, occupying a leading position in countries with high and average living standards, not only in terms of morbidity, but also in terms of mortality [1]. The widespread prevalence of cardiovascular diseases (CVD) is a problem not only for medicine, but also for society as a whole, with the frequent development of severe complications leading to disability of people of working age, as well as premature death [4]. Ischemic heart disease (IHD) occupies a predominant share in the structure of CVD, according to various authors, IHD, as a cause of death, accounts for 42 to 61% of the total number of deaths in economically developed countries. This problem is also relevant in Uzbekistan. According to the results of WHO research, the Republic of Uzbekistan, like many other countries of the world, belongs to countries with a high risk of developing CVD. Uzbekistan has entered the top five leading countries in terms of mortality from cardiovascular diseases. According to the latest data published by World of Statistics on Twitter, in 2023, 61% of deaths in Uzbekistan are associated with diseases of the circulatory system [5].Over the last decade, there has been a tendency to increase the number of patients with comorbidity of ischemic heart disease and COPD. This is due to the common risk factors of these diseases. Persistent inflammation is one of the leading mechanisms of atherogenesis and CVD in COPD. The combination of coronary heart disease and COPD, according to various studies, ranges from 10% to 62.8%, in the elderly up to 78% [2]. Ischemic heart disease and COPD are often combined in one patient. Chen J. et al. After conducting a large-scale epidemiological study involving 201,752 patients with coronary heart disease, we obtained data indicating that COPD occurs in such patients in 21% [3]. Recent studies have shown that in order to understand the pathogenesis of coronary heart disease, further study of circulatory regulation systems is necessary, in particular the sympathetic adrenal system (SAS), the function of which is assessed by the excretion of catecholamines, metabolic products of biogenic amines and enzymes involved in their metabolism [6].Purpose of the study: To study the state of the sympathoadrenal system in patients with ischemic heart disease in combination with chronic obstructive pulmonary disease.
2. Material and Methods
- The object of the study was 58 patients, of whom 29 were diagnosed with coronary heart disease and 29 patients with a combination of ischemic heart disease and COPD, 20 healthy volunteers were taken as a control group. All participants had written consent to participate in the study. The content of catecholamines - adrenaline, norepinephrine and dopamine, the metabolite – vanillylmindal acid (VMA) in daily urine, as well as malonic dealdehyde (MDA) and the enzyme oxidative deamination of KA - monoamine oxidase (MAO) in blood serum were determined in all patients. The indicators were determined by the ELISA method using standard kits manufactured by Demeditec Diagnostics GmbH (Germany) on the Mindray MR-96 ELISA analyzer (China).Statistical data processing was performed using the Microsoft Excel – 10 software package with the calculation of the average values (M) of their arithmetic mean errors (m), as well as the confidence coefficient of the difference between the Student's compared values (t).
3. The Results and Discussion
- A comparative analysis of the results obtained by the studied groups showed that in patients with coronary heart disease, relative to patients with a combination of coronary heart disease and COPD, the content of vanillylmandelic acid (VMA) in daily urine was significantly (p<0.05) lower by 43.3% (Table 1). Relative to the control group, the indicators of both studied groups of patients were statistically significantly lower (p<0.05) by 196.7% and 107.0%, respectively, groups 1 and 2.
|
4. Conclusions
- A comprehensive examination of patients with IHD in combination with COPD showed significant dysfunction of the sympatho-adrenal system, namely: a decrease in adrenaline levels, an increase in norepinephrine and dopamine levels, which indicates a violation of the activity of the sympatho-adrenal system in this category of patients. In IHD, as well as in combination with IHD and COPD, there is a significant decrease in the activity of monoamine oxidase relative to the control group, which indicates a change in its catalytic properties.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML