-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2738-2741
doi:10.5923/j.ajmms.20241411.12
Received: Oct. 12, 2024; Accepted: Nov. 5, 2024; Published: Nov. 7, 2024

Improvement of Surgical Tactics in Cases of Acute Stone Colecystitis with Diaphragm Hernia
Urokov Sh. T.1, Kholikov F. Y.2
1Department of Surgical Diseases, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
2Bukhara Branch of the Republican Scientific Center for Emergency Medical Care, Bukhara, Uzbekistan
Correspondence to: Urokov Sh. T., Department of Surgical Diseases, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The scientific work was carried out in 2017-2024 at the Bukhara branch of the Republican Emergency Medical Research Center in the I-II emergency surgery departments. Laboratory and instrumental examination methods were used to examine such patients. Clinical and laboratory methods of diagnostic algorithm, ultrasound and endoscopic examination of abdominal organs, condition of large duodenal tube, endoscopic examination of the upper part of the gastrointestinal tract, MSCT, x-ray contrast examination of the gastrointestinal tract were performed according to the instructions. Based on An in-depth comparative analysis of early and long-term results of surgical treatment has shown an improvement in the effectiveness of surgical treatment of patients with cholelithiasis associated with gastroesophageal reflux disease and hiatal hernia. In practice, the choice of tactics is carried out by the calculation method using the original formula. Thanks to the research, it was possible to optimize the tactics of surgical treatment of patients with comorbidities.
Keywords: Acute calculous cholecystitis, Hiatal hernia, Cholecystectomia, Combined pathology
Cite this paper: Urokov Sh. T., Kholikov F. Y., Improvement of Surgical Tactics in Cases of Acute Stone Colecystitis with Diaphragm Hernia, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2738-2741. doi: 10.5923/j.ajmms.20241411.12.
1. Introduction
- Researchers have established a close relationship between gallstone disease, particularly acute cholecystitis, and diaphragmatic esophageal hiatal hernia. R.B. Avakyan and A. L. Guscha, in particular, caused by gastroesophageal reflux, is considered to be a natural combination of the development of diaphragmatic esophageal hernia and gallstone disease. Clinical syndromes described over many years of surgical history support these views. One of these syndromes is Saint's triad, which includes a combination of diaphragmatic esophageal hiatal hernia, gallstone disease, and diverticulosis of the colon, diagnosed in 3.2-5% of cases. The next syndrome is Kasten's triad, which occurs in 7.2% of cases and is characterized by a combination of gallstone disease, duodenal ulcer, diaphragmatic esophageal hernia. A separate combination of acute cholecystitis and diaphragmatic esophageal hernia occurs in 4.5-60% of patients [1,2,3,4,5,6].Although conventional and laparoscopic cholecystectomy methods have been well studied and improved, the results of surgical treatment of patients with cholelithiasis still cause certain problems. According to the literature, up to 20% of patients who have had their gallbladder removed continue to have problems known as "Postcholecystectomy Syndrome" [7,10]. This syndrome includes new onset of upper abdominal pain and indigestion after cholecystectomy.In more than 10-20% of cholecystectomy patients, the appearance of pain attacks in the abdominal cavity in the postoperative period is noted. It should be noted that more than 80% of unsatisfactory cases after cholecystectomy are not directly related to the operation itself [8,9].The purpose of the work: to increase the effectiveness of surgical tactics and treatment in cases where acute cholecystitis and esophageal hiatus hernias are present.
2. Materials and Methods
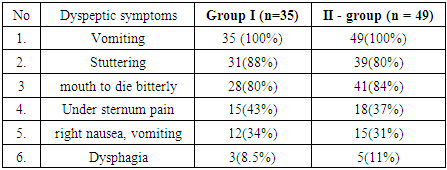
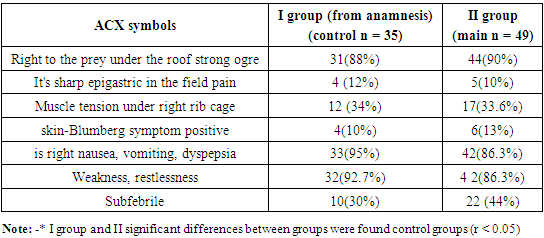
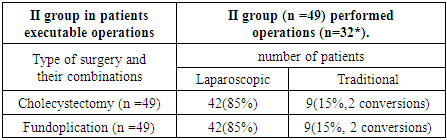
- The scientific work was carried out in 2017-2024 at the Bukhara branch of the Republican Emergency Medical Research Center in the I-II emergency surgery departments.Laboratory and instrumental examination methods were used to examine such patients. Clinical and laboratory methods of diagnostic algorithm, ultrasound and endoscopic examination of abdominal organs, condition of large duodenal tube, endoscopic examination of the upper part of the gastrointestinal tract, MSCT, x-ray contrast examination of the gastrointestinal tract were performed according to the instructions.Control patients were divided into 2 groups. Group I included patients with acute stone cholecystitis who were operated on at different times (cholecystectomy) but had dyspeptic complaints (n=35). These patients complained of various dyspeptic symptoms in the postoperative period: boils in the urine, abdominal pain, bitter taste in the mouth, pain under the chest after eating, belching. Diaphragmatic esophageal hernia (DEG) and various degrees of reflux-esophagitis and gastroesophageal reflux disease (GERD) were detected among this group of patients when the above-mentioned instrumental examination methods were performed. Clinical symptoms in these patients mostly a retrospective disease histories on the surface and current h on the surface inspections take went II is the main group patients (n =49) referred with ACD hanging came and in complaints main attack symptoms tash q ari, time dyspeptic suffering with symptoms smoked in patients, in addition, the above - mentioned instrumental inspection methods the spleen is crushed h ahead different level patients with advanced DVT separate received by difference women (36 men and 48 women) advantage it happened.
3. Results and Discussion
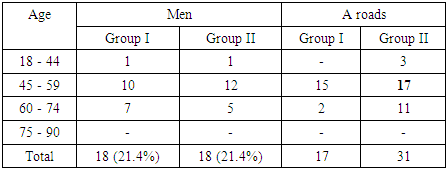
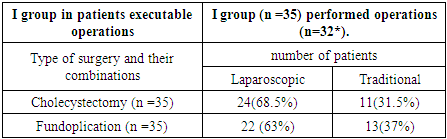
- All patients in the control group underwent laparoscopic cholecystectomy for acute calculous cholecystitis in different clinics and at different times over the past 10 years. The diagnosis of concomitant GERD and hiatal hernia was established in 12 (35.3%) patients in the control group before LCE. In all these patients, reflux complaints increased after LCE.The basis for choosing surgical tactics in the control group was the standard method for determining the area of the hiatal opening without taking into account the above factors.According to statistical calculations using the Student's t-criterion, a statistically significant difference was found between the effectiveness of treatment in the main and control groups (significance level p < 0.05).The reliability of the improvement in the treatment results of patients in the main group compared to the control group was statistically confirmed, in connection with which it can be said that the factors taken into account in the original formula for calculating the choice of surgical tactics in the treatment of combined pathology are of fundamental importance.The distribution of patient by age and gender is presented in Table 1.
|
|
|
|
|
4. Conclusions
- Patients presenting with acute stone cholecystitis have a symptom complex consisting of general dyspeptic symptoms characteristic of chronic stone cholecystitis and diaphragmatic esophageal hernia diseases for a long time. In the treatment of patients, in the pre-operative period, when there is a suspicion of esophageal hernia, gastroesophageal reflux disease, additional instrumental examinations should be conducted.The sequence of operations should be maintained in patients with acute stone cholecystitis, who are referred to esophageal hiatus hernias, GERK. First of all, cholecystectomy, and in the second stage, performing a fundoplication operation, replacing the instruments with ultrasound devices.The advantages of using laparoscopic surgical methods over traditional methods are low traumatization, as well as low probability of development of specific complications for laparotomic wounds (suppuration, formation of postoperative hernias). Also, simultaneous operations in this category of patients are more appropriate from a medical and economic point of view.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML