Mirzaev Valijon1, Urokov Shuhrat2
1Bukhara Branch of the Republican Scientific Center of Emergency Medical Care, Bukhara, Uzbekistan
2Department of Surgery Diseases, Bukhara State Medical Institute named after Abu Ali Ibn Sino, Bukhara, Uzbekistan
Correspondence to: Mirzaev Valijon, Bukhara Branch of the Republican Scientific Center of Emergency Medical Care, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
According to the authors, in the last 30 years, the growth rate of acute pancreatitis worldwide has been observed twice or more. The course of acute pancreatitis is characterized not only by the inflammatory process of the pancreas, but also by damage to many other organs. Investigation is to improve the tactics of diagnosis and treatment of acute pancreatitis in cases accompanied by chronic diffuse diseases of the liver. The ban work is based on the analysis of 120 patients who were undergoing inpatient treatment in the 1st and 2nd surgical department of the Bukhara branch of the Republican Scientific Center for Emergency Medical Care during 2015-2019. The medical histories of 120 patients with different severity levels of Acute Pancreatitis (moderate and severe late patients) were analyzed in the I-control group, and the conservative and surgical methods, observed complications and mortality rates were retrospectively analyzed. Patients without Cirrhosis of the Liver were taken as a background disease. Patients in this group underwent standard conservative therapy and operative treatment operations.2,550 patients admitted to the II main group during 2019-2023 with various degrees of acute pancreatitis and its complications were admitted. The acute inflammatory process in the pancreas complicates the functional state of the liver and leads to a decrease in metabolism and an increase in the pathological focus. It is worth noting that the early onset of the inflammatory process leads to the spread of the inflammatory process to the surrounding tissues and the presence of complicated pancreatitis and an increase in the atypical clinical manifestations of the disease.
Keywords:
Acute pancreatitis, Chronic diffuse diseases of the liver, Surgical treatment
Cite this paper: Mirzaev Valijon, Urokov Shuhrat, Diagnosis and Treatment Tactics in Patients with Liver Cirrhosis and Acute Pancreatitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2730-2737. doi: 10.5923/j.ajmms.20241411.11.
1. Introduction
According to the authors, in the last 30 years, the growth rate of acute pancreatitis worldwide has been observed twice or more. [1,2,8]The course of acute pancreatitis is characterized not only by the inflammatory process of the pancreas, but also by damage to many other organs [11,14].According to a number of authors, the frequency of other organ damage and complications in acute pancreatitis ranges from 60.8% to 96.5% [5,6]. The pathological process, especially destructions of various levels, provokes the inflammatory process and accelerates the systemic inflammatory reaction [8,9].In acute pancreatitis, the development of functional liver failure is observed in 40.8% of cases. At the same time, changes in liver function were noted in 23.3% of cases in patients with inflammatory forms of severe pancreatitis, and in 83.9% of cases in destructive forms [12,13].Acute Pancreatitis and Cirrhosis of the Liver are two serious medical conditions that can affect each other and make the disease worse.Acute pancreatitis and Cirrhosis of the Liver together creates a difficult diagnostic task, because their symptoms are similar and the appearance of the disease is changed. A special approach is required to accurately distinguish and manage these conditions. Patients with acute pancreatitis and liver cirrhosis often have high morbidity and mortality, worsening disease course and mortality. This condition, in turn, requires careful study of individual treatment strategies to reduce negative consequences [2,17,18,20].Although the pathological process is covered in the literature, Cirrhosis of the Liver is not always taken into account in the treatment tactics of OP due to the fact that the clinical appearance of Cirrhosis of the Liver is often hidden [8,11,13,19].The purpose of the investigation is to improve the tactics of diagnosis and treatment of acute pancreatitis in cases accompanied by chronic diffuse diseases of the liver.
2. Research Materials and Methods
The scientific work was carried out at the clinical base of the Department of "Surgical Diseases" of the Bukhara State Medical Institute named after Abu Ali Ibn Sina (I-II Emergency Surgery Departments of the Bukhara branch of the Republican Scientific Center for Emergency Medical Care). Between 2015 and 2019, 2,410 medical histories treated in the clinic for acute pancreatitis were retrospectively analyzed, and 35 (1.4%) of patients with acute pancreatitis and Liver Cirrhosis (in different stages of Liver Cirrhosis) as a comorbidity were diagnosed with Liver Cirrhosis of various degrees.The medical histories of 120 patients with different severity levels of Acute Pancreatitis (moderate and severe late patients) were analyzed in the I-control group, and the conservative and surgical methods, observed complications and mortality rates were retrospectively analyzed. Patients without Cirrhosis of the Liver were taken as a background disease. Patients in this group underwent standard conservative therapy and operative treatment operations.2,550 patients admitted to the II main group during 2019-2023 with various degrees of acute pancreatitis and its complications were admitted. During the clinical, anamnestic, laboratory and additional and in-depth instrumental examinations of these patients, 128 (5%) of them had liver cirrhosis of various degrees. In order to improve the results of treatment in patients, planned examination and treatment (conservative and surgical) methods were used and taken as the main group. In addition to the standard treatment, Ulinastatin, Glutathione and Remaxol drugs were used in the first days of the main group of patients. After the elimination of dyspeptic symptoms (nausea and vomiting) in the patients from 3 days on, enteral feeding through a tube Nutricomp Standard (B. Brown company) enteral feeding was started.
3. Results and Discussion
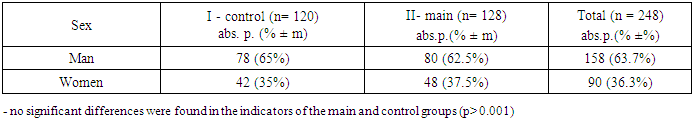
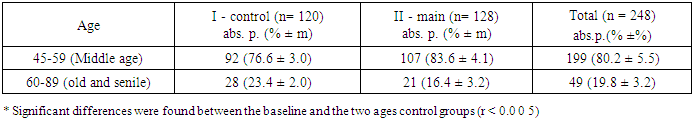
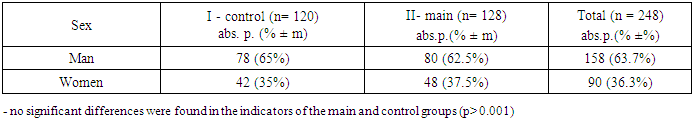
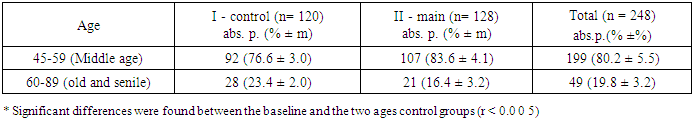
JTs were diagnosed using abdominal cross-sectional imaging, computed tomography, and magnetic resonance imaging.In 128 patients included in this group, in addition to the above-mentioned standard examination and treatment procedures, JTs were diagnosed according to the guidelines, as a result of CT scan, MRPXG, elastography, and intraoperatively.Patients were diagnosed based on anamnesis, clinical data, laboratory and instrumental examination methods. Patients came to the branch, through the emergency line, through a referral from the polyclinic or by private car, and were admitted.At the initial stage, the research groups were compared according to various clinical, laboratory and endoscopic data - age, gender, blood pressure, money, hemoglobin, red blood cells, urea, sugar in the blood, biochemical tests (bilirubin, amylase, ALT, AST, urea, creatine, total oxygen and albumin, prothrombin index, thrombotest, HBsAg, HBeAg, anti-HBe, anti-HBc markers were determined.Young. In terms of structure, the two observational groups were similar in terms of gender (r >0.05). In the structure of patients by age groups, according to the classification of the World Health Organization [1963], observation I and II - more than half of the patients who developed AP on the background of JTs in the groups are middle 45-59 (76.6% and 83.6%, respectively) he said K -axes and old age are 60-89 (23.4% and 16.4%, respectively). According to the mean age, both observational groups were homogeneous (r >0.0 0 5). Table 1.Age of patients in group I was 60±6.5 years, in group II - 64±2.2 years. The three observation groups were similar in terms of mean age, and no statistically significant differences were found (r >0.0 05).Table 1. AP on the background of Liver Cirrhosis (primary) and Liver Cirrhosis developed by you (control) according to gender
 |
| |
|
In other age groups (45-59 years, 60-89 years) there is no significant difference between the main and control groups (r >0.0 0 5). (Table 2).Table 2. In the background of Liver Cirrhosis of OP and Liver Cirrhosis developed patients age distribution
 |
| |
|
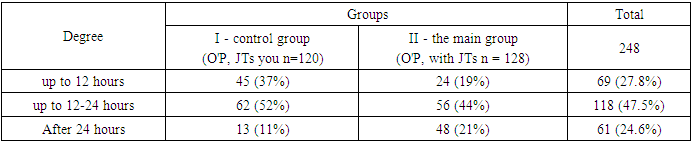
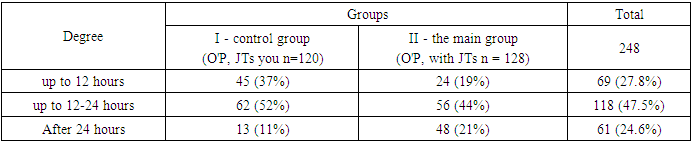
When dividing the patients by sex, it was revealed that female patients were 2 times less likely to be infected than men, 65% of group I patients were male and 35% female, 62.5% of group II patients were male. and 37.5% were roads.The clinical presentation of acute pancreatitis against the background of liver cirrhosis consists of a complex interaction of symptoms and signs that are difficult to separate from the symptoms of the disease. The presence of liver cirrhosis can mask or change the classic clinical presentation of acute pancreatitis, which obviously makes it difficult for medical professionals to diagnose.Acute pancreatitis is diagnosed when at least two of the following three symptoms are present:1) abdominal pain characteristic of acute pancreatitis;2) a 3-fold increase in the level of lipase in q or amylase in q in relation to the upper limit of the norm;3) identification of characteristic signs during ultrasound and contrast CT, MRI.The time of onset of the disease is considered to be the time of appearance of usual abdominal pain.Table 3. Patient referral times after onset of illness
 |
| |
|
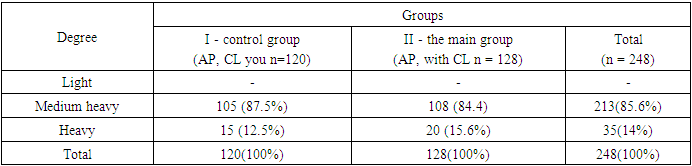
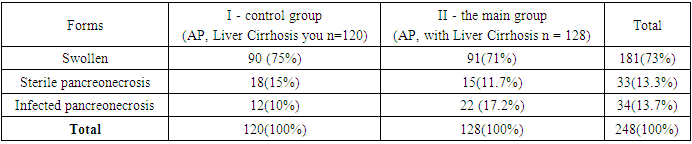
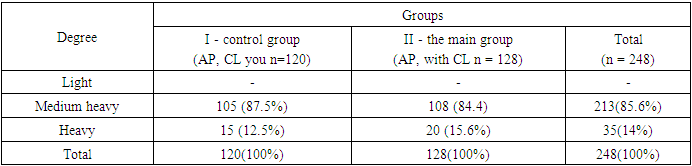
It was found that patients in both groups were referred after the onset of the disease, while patients in the control group were referred earlier. This situation, in our opinion, was due to the presence of Liver Cirrhosis in the main group of patients and the fact that the disease was associated with this disease.For the purpose of traditional conservative therapy, infusion, spasmolytic, pain-relieving, antibacterial drugs were used.4th generation cephalosporins are used for antibacterial therapy.Glucose, amino acids (vamin), fat emulsions (intralipid, lipofundin) are used for parenteral nutrition. Nutricomp Standard was used for the purpose of early enteral feeding in the main group of patients.Atlanta 2012 classification, patients with moderate and severe conditions were included in the control groups.According to this classification, patients of both groups were divided into groups on the day of arrival depending on the degree of AP severity.Based on this, moderate patients were 105(87.5%) and 108(84.4%) in the control and main groups, respectively, and 15(12.5%) and 20(15) patients in the control and main groups, respectively. 6%) (table 1).Local complications of acute pancreatitis include acute parapancreatic fluid collection, pancreatic pseudocyst, acute necrotic collection, and circumscribed necrosis. Systemic complications are an exacerbation of a previously existing disease, for example, as a result of pancreatitis, there is an exacerbation of cardiovascular diseases or chronic lung diseases.Table 4. Distribution of patients in groups according to the Atlanta classification
 |
| |
|
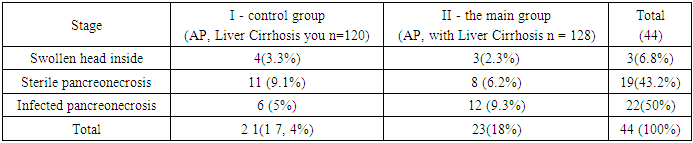
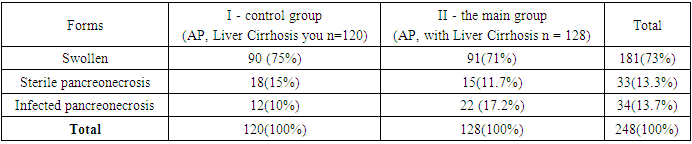
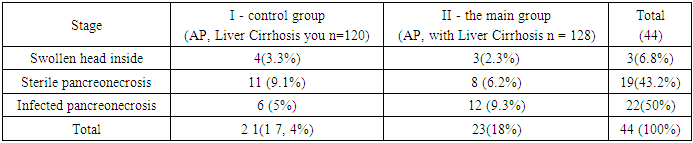
Mortality rates by groups: In the control group, the mortality in the tumor stage was 4(3.3%), in the stage of sterile pancreonecrosis was 11(9.1%), and in infected pancreonecrosis was 6(5%).In the main group, there were 3 (2.3%) deaths in the tumor stage, 8 (6.2%) in sterile pancreonecrosis, and 12 (9.3%) in infected pancreonecrosis. A total of 21(17.5%) and 23(18%) were observed in both groups. (table 5).Table 5. Forms of OP control and main groups
 |
| |
|
Taking both groups, 19 (43.2%) patients died as a result of pancreatogenic shock and polyorgan failure during sterile pancreonecrosis, and 22 (50%) died as a result of septic complications during infected pancreonecrosis. (Table 6.)Table 6. Distribution of mortality rates by stages of pancreatic necrosis
 |
| |
|
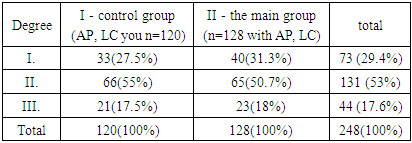
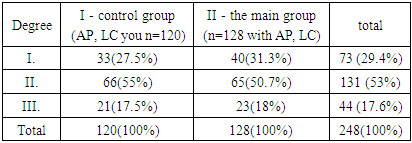
Pathogenetically, in acute destructive pancreatitis, taking into account the fact that the origin of polyorgan failure is endogenous intoxication and SIRS, the assessment of the severity of the condition by indicators of endogenous intoxication reflects objectively.Table 7. Distribution according to the degree of endotoxicosis
 |
| |
|
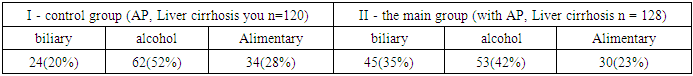
In both groups of patients, the I degree of endotoxicosis was on average 73 (29%), while the II-III degree was 71%. (table 7.) The distribution of the groups according to the development of endotoxicosis is represented by the results obtained in the first days of the patients.Alcohol consumption is a common cause of both COPD and cirrhosis. In the scientific literature, there is limited information on the epidemiological relationship between AP and JTs, and the results of treatment of AP against the background of LSs are unknown.Table 8. Distribution of patients in research groups according to the etiology of AP
 |
| |
|
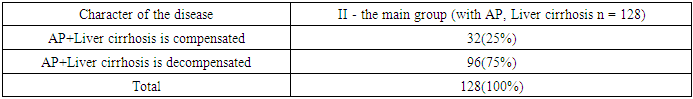
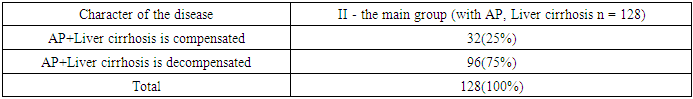
More than 52 (41%) of the main group of patients did not know that they had liver disease at the time of admission to the surgical hospital, and it was detected during examinations, while the majority of them, 76 (59%), knew that they had the disease and had been treated before.We conducted a retrospective study to compare AP outcomes in cirrhotic patients and non-cirrhotic patients admitted to our institution. Patients who developed liver cirrhosis were also divided into two subgroups: compensated cirrhosis and decompensated cirrhosis.Comparison of decompensated and compensated cases of liver cirrhosis was performed in group analysis. When analyzed according to the Child-Pugh scale, Child-Pugh class A was considered compensated, Child-P and V and C were considered decompensated (table 9).Table 9. Distribution of patients by the nature of liver damage in LC (n=128)
 |
| |
|
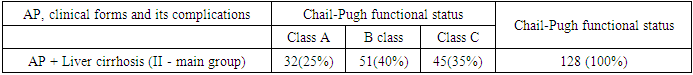
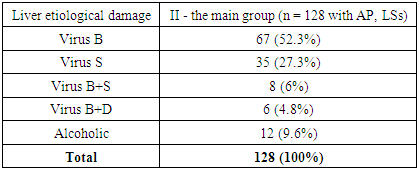
32 patients with JTs (25%) had Child-P yu A, 51 patients (40%) had Child-P yu B, and 45 patients (35%) had Child - P yu S.All patients of the main group (n =128) were divided according to the Child-Pugh scale according to AP complications and liver functional disorders. Analysis of the etiological causes of LC revealed the following. The main etiological factors of JTs are infections, more than half of the patients were viral hepatitis V 67(52.3%) and viral hepatitis C infection was 35(27.3%), which accounted for a quarter of the studied patients.Table 10. There was AP in the background of Liver cirrhosis (main group II) distribution of patients according to the main group Child-Pugh according to the functional state of the liver (n=128)
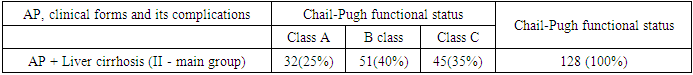 |
| |
|
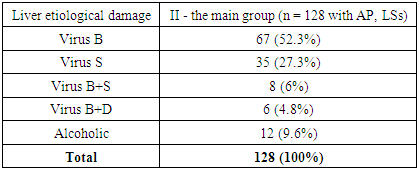
In the remaining cases, mixed virus infection was B+C 8(6%) and B+D 6(4.8%), respectively. According to anamnestic data and negative PTsR analysis, alcoholic liver diseases were calculated, and 12 (9.6%) cases were recorded in the respective groups. (Table 11).Table 11. Etiologically isolated LS (n =128)
 |
| |
|
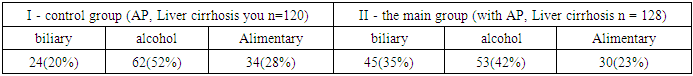
Clinical and laboratory research methods. Clinical analysis. In the diagnosis of liver diseases, great importance was attached to the traditional examination method, which includes general clinical examinations, complaints, anamnesis, general and local condition study. Minor symptoms of liver failure (lethargy, general weakness, increased irritability, reduced work capacity, lack of motivation); pain syndrome under the right rib cage and its nature, discomfort, heaviness, boils in urine, dyspeptic complaints and similar symptoms were determined. Manifestations of hemorrhagic syndrome include bleeding from the gums, bleeding from the lower and upper extremities. It is also manifested by signs of portal hypertension syndrome (bleeding from the stomach and hemorrhoidal vessels, splenomegaly, hepatomegaly). They are manifested by cholestacholestatic syndrome (itching of the skin, yellowing of the skin, dark color of urine, white stool).Laboratory diagnostics included a routine set of clinical and biochemical blood tests that were taken for everyone. It is necessary to check urine, bile pigments for urobilin, and feces for stercobilin. These indicators are of clinical significance in the period of increasing or persistently high hyperbilirubinemia. General clinical studies have complemented functional research methods, which play an important role in the diagnosis of liver diseases. Functional studies were performed according to the generally accepted program.The main biochemical syndromes of viral hepatitis and indicators of markers related to them (in particular, HBV, HCV, HDV) were determined. We used the following pointers:1. Cytolytic syndrome - ALT, ACT;2. mesenchymal-inflammatory - gammaglobulins, thymol, sulemic tests;3. cholestatic syndrome - total and bound bilirubin, IF;4. hepatodepressive syndrome-albumin and prothrombin.Cytolytic syndrome was considered as one of the main indicators of pathological process activity in the liver. ALT and mild forms of chronic hepatitis according to the increased level of AST (ALT and ACT Less than 3 standards), moderate (up to 5 standards) and severe (increased from 5 to 10 standards) were distinguished. Indicators of mesenchymal-inflammatory syndrome were used to assess the stage of the disease, the activity of the pathological process, and to determine the prognosis of the disease. The degree of impairment of the synthesis function of the liver was assessed by changes in the indicators of hepatodepressive syndrome. Changes in the indicators of cholestatic syndrome reflected the violation of bile secretion and blood circulation.To determine the functional state of the blood coagulation system and its rheology, the following parameters were determined: blood coagulation time according to Lee-White, recalcification time in plasma according to Bergergar, plasma tolerance to heparin - according to Sutt's method, plasma tolerance to heparin according to Sutt's method, fibrinogen activity in blood - according to Ritberg's method, fibrinolytic in blood - The duration of prothrombin time and the content of fibrinogen were determined by Kowalski-Kolen-Nevarenyi, colometric method.Instrumental research and treatment methods. Ultrasound sonography.UTS examination was performed in all the examined patients. UTS focuses on two things, namely the liver parenchyma. The condition of the liver parenchyma, the unevenness of its surroundings (edges), its size, the blood vessels entering and leaving the liver, their size, as well as the condition of the anastomoses of the portal blood circulation and portal system in some patients, using ultrasound sonography and dopplerography by "Sonoline Vera Pro" firm "Siemens" (Germany) and "Echo Camera SSD-680" firm "Aloka" (Japan) were studied using a 3.5 MHz convex sensor.Relatively equivalent changes are observed in parameters such as the size of the liver, the state of its front edge, and the medium and coarse-grained echostructure of the liver parenchyma in patients with OP and LS.In some cases, magnetic resonance computed tomography (CT) was used in the development of AP and LC and differential diagnosis with other diseases of the hepatobiliary tract. The examination was carried out on the third generation ST-MAX 640 device manufactured by General Electric (USA) "General Electric". Diffuse liver enlargement, parenchymal density was emphasized in chronic hepatitis. JTs are characterized by changes in shape and size. The density of the parenchyma is often non-uniform, the spleen is enlarged, and the diameter of the portal and splenic vessels is increased. Determination of free fluid in the abdominal cavity is an important additional information. At the same time, it should be remembered that small and soft pigment stones are not clearly visible during conventional CT, and in some cases they are not even detected, but the degree of accuracy is high when performing MRPXG.Endoscopy. "FUJIFILM", Japan) to determine the presence of varicose veins of the esophagus and the degree of their expansion.The condition, expression, duration of varicose veins of the esophagus and stomach, degree of inflammatory-degenerative changes of mucous membranes A. G. According to Schertsinger (1988), the risk of bleeding was determined: level 1 of VCV expression - 0.1-0.2 cm, level 2 - 0.3-0.4 cm and level 3 - 0.5 cm and more.The examination was carried out with the patient lying on the left side. All patients underwent a videoesophagogastroduodenoscopy, using a videogastroscope, in which the mucous membranes of the esophagus, stomach and duodenum were evaluated. Initially, the PENTAX-34 K fibroduodenoscope was used, and from 2020, the Japanese "FUJIFILM" videoduodenoscope was used.MRI magnetic resonance imaging is understood as a process that accurately describes the structure of soft tissues, bones, or in a word, all organs in the human body by using a strong magnetic field, high-frequency pulses and a computer system.The MRXPG method is a special type of magnetic resonance imaging (MRT) and is a modern diagnostic method that clearly depicts the hepatobiliary system, including the liver, gallbladder, bile ducts, and pancreas, and is currently the gold standard. This method is a non-invasive examination method that describes the bile ducts using magnetic resonance computed tomography without contrast agents. This examination provides information about the presence of stones, strictures and tumors in the area that obstruct the normal flow of bile by showing the discharge of bile at a specific time.The processing of the research results was carried out by statistical methods with the determination of relative indicators, average values: the arithmetic mean (M), the mean (m ±) and the standard error of the medians, 25 and 75 percent, the significance level of the confidence interval was 0.05.According to the t-test, the statistical significance of the differences in the mean values and relative values of the main and two control groups was checked. Differences are considered significant if the confidence interval significance level is less than 0.05 (p < 0.05) and 0.01 (r < 0.01). The homogeneity of the main and control groups of the observation was checked using the Wilcoxon test (with the number of variants 6 or more). A comparative analysis of variables was performed using the non-parametric Wilcoxon-Manna-Whitney test.In our work, we took only patients with moderately severe and severe advanced AP, because about 70% of patients recover from a mild condition in 24-48 hours. In these investigations, we paid special attention to the impact of LC, which is a comorbidity of patients in the main group, on the course of the disease.At the time of the patients' visit to the hospital, 90 (75%) of the patients in the control group and 91 (71%) of the patients in the II - main group developed a tumorous form of AP. A total of 181 (73%) cases of swelling in both groups. In the selection of patients, mild forms of OP and patients whose disease regressed within 48 hours were not included. Control group patients were treated according to the accepted standard. In order to correct JTs in the main group of patients and reduce complications, hepatoprotectors (Glutathione, Remaxol, Ulinastatin) and enteral nutrition Nutricomp Standard (B. Brown company) were recommended along with standard treatment.In the second week, sterile pancreonecrosis was 18(15%) in the control group, 15(12.5%) in the main group, and 33(13.3%) in both groups. Infected pancreatic necrosis accounted for 12 (10%) in the first group without JTs, compared to 22 (17.2%) in patients with primary LS A total of 34 (13.7%) in the binary group did (Table 9.)Out of 120 patients in the control group, 24 (20%) had OTC and its complication choledocholithiasis. 62 (52%) had an alcoholic etiology and 34 (28%) had an alimentary cause.Out of 128 patients in the main group of patients - 45 (35%) were caused by OTC and its complication choledocholithiasis. 53(42%) had alcoholic etiology and 30(23%) had alimentary cause.In patients of the main group, when there was an indication for surgery, as much as possible, 17 (13.3%) of them tried to perform laparoscopically in a minimally invasive way.It can be seen that in the main group of patients, that is, in patients with various degrees of developed JTs, OTC, which came as a cause of OP, is statistically 2 times more accurate than in the control group. The rest of the etiological causes of OP have almost similar indicators.It appeared as follows in the section of the stages of the disease and in the section of the complications of the disease.In the control group: 4 (3.3%) patients died of pancreatogenic shock in the initial inflammatory stage of the disease, 11 (9.1%) patients died of sterile pancreonecrosis (2 patients with, 4 patients with hepatorenal syndrome, 5 patients with fermentative peritonitis POE). In the period of infected pancreonecrosis, i.e. in the 3-4 weeks of the disease, 6 (5%) patients died (4 from purulent peritonitis and sepsis, and 2 from purulent inflammation of the parapancreatic cell, erosive bleeding from blood vessels) (Table 8.).In the main group: 3 (2.3%) patients died of pancreatogenic shock in the initial inflammatory form of the disease, 8 (6.2%) patients died in the case of sterile pancreonecrosis (5 patients from kidney-liver failure and 3 patients from). 12 (9.3%) patients died during the period of infected pancreonecrosis (7 from purulent peritonitis and sepsis, 2 from purulent inflammation of the parapancreatic cell, 2 from erosive bleeding from blood vessels, 3 from) during 3-4 weeks of the disease.Thus, although the background disease JTs in the main group of patients, the rates of complications and mortality in the groups were statistically the same. Although our study shows that among hospitalized OP patients, patients with LC had a higher in-hospital mortality rate, we believe this is related to complications of LC and portal hypertension. In the main group of patients, 3 patients died from CVV bleeding.We hypothesized that the high mortality rate may be related to the complications of LC and portal hypertension, which is associated with a higher rate of gastrointestinal bleeding, shock, and sepsis in LC patients.The influence of LS on the pathophysiology of OP is multifaceted. Healthcare providers should consider these interactions when diagnosing and treating OP in patients with LC In the background of LC, diagnostic problems in patients with OP were reviewed and therapeutic strategies used for effective treatment of OP were studied.
4. Conclusions
The effectiveness of Ulinastatin, Glutathione, Remaxol and early enteral nutrition in the main group of patients, in the prevention and treatment of complications, in compensated patients with Cirrhosis of the Liver Child-Pugh A was especially evident. 37(30.8%) patients in the control group developed IES, and 7(5.5%) developed Acute Pancreatitis on the background of Compensated Liver Cirrhosis (Child-Pugh A class) in the main group. In Child-Pugh classes V and C, liver cirrhosis worsens the course of acute pancreatitis.Gallstone disease (biliary etiology) as a cause of Acute Pancreatitis was observed in the main group of patients, that is, in patients with cirrhosis of the liver of various degrees, compared to patients without cirrhosis.When acute pancreatitis develops against the background of liver cirrhosis, endoscopic probing of the small intestine and early feeding of patients through this probe reduces IES syndrome, its complications, and the best way to feed patients is artificial feeding through the intestine. This is done through a nasogastric and nasoenteral probe, which is inserted endoscopically into the initial part of the intestine.
References
| [1] | Abu-Zidan F.M., Bonem M.Dj.D. i Windsor Dj.A. (2000). Severity of acute pancreatitis: multifactorial analysis of markers of oxidative stress and modified criteria Glasgow. British Journal of Surgery, 87(8), 1019–1023. https://doi.org/10.1046/J.1365-2168.2000.01464. X. |
| [2] | Akopyan V.S. Clinical and morphological changes in the liver of patients with acute abdominal pain in chronic alcohol intoxication. Diss... cand. Med. science - M., 2001. |
| [3] | Aleksandrov D.A., Gromov M.S., Stetsyuk O.A., Tataurov A.V. Differentiated surgical tactics in destructive pancreatitis. // Surgery. -2002. - No. 11. -p. 58-62. |
| [4] | Alexandrova I.V., Pervakova E.I., Vasina E.I., Ray S.I. Complex extracorporeal correction of hepatic insufficiency. // 5th international conference "Actual aspects of extracorporeal blood transfusion and intensive therapy" Moscow, May 25-26, 2006. - Moscow, 2006. - 34-35. |
| [5] | Alimkhajiev A.S. Prognosis of acute pancreatitis based on an integrated assessment of endotoxicosis: Diss.cand. Med. science // GOUVPO "Voronezh State Medical Academy" (GOUVPO "VGMA"). -2005, 83 p. |
| [6] | Ahn BO, Kim H, Lee G. i dr. The effect of taurine on acute pancreatitis in mice. Pharmacology 2001; 63: 1-7. |
| [7] | Andreev G.N. The result of laparoscopic surgery in cirrhosis of the liver. / Andreev G.N. A.S. Ibadildin // Abstracts of the 1st All-Russian Congress on Endoscopic Surgery. - Moscow 1998. - P. 3. |
| [8] | Andreev G.N., Tashev I.A., Apelbaum L.S. Diagnosis and treatment of chronic and diffuse inflammatory bowel disease. V. Novgorod: Viscount. 2003. 162 p. |
| [9] | Andreev, G.N. Endochirurgicheskaya correction of cirrhosis of the liver / G.N. Andreev, I.A. Tashev // Clinical medicine: mejvuz. sb. - Almaty, 1998. - S. 62-64. |
| [10] | Andryushchenko L. V., Kunovsky V. V., Andryushchenko V. P. Clinical and pathomorphological manifestations of the syndrome of intestinal insufficiency and acute necrotic pancreatitis. - Kharyuvska khyppri Yes School, 2010. - No. 3 (41). - P. 5 - 7. |
| [11] | Andryushchenko V. P, Andryushchenko D. V., Kogut L.M. Anti-secretory drugs for the treatment of acute pancreatitis: dosage forms for implementation - emergency medicine, 201 3. - No. 6 (53). - S. 71-74. |
| [12] | Bagnenko S.F., Tolstoy A.D., Krasnorogov V.B. Acute pancreatitis (Diagnostic and treatment protocols). -2004. |
| [13] | Barkvist E., Kirton O., Windsor D. The effect of antioxidant and splanchnic-directed therapy on the stoic uncorrected level of mucous membrane of the stomach and the patient with traumatic trauma. Traumatology care Inf Grit Tsar 1998; 44: 355-60. |
| [14] | Vlasov A. P., Shibitov V. A., Geraskini V. S. i dr. // Fundamental research. - 2012. - No. 2. - P. 271-275. |
| [15] | Gabrielyan N.I., Lipatkova V.I., Experience of using a screen of medium-sized molecules in the blood for the diagnosis of nephrological diseases in children. // Laboratory work. - 1084. - No. 3. - P. 138-140. |
| [16] | Gain Yu.M., Leonovich S. I., Alekseev S.A. Enteral insufficiency syndrome in peritonitis: theoretical and practical aspects, diagnosis and treatment. Minsk: Molodechno 2001; 266. |
| [17] | Galimova, S.F. Chronic hepatitis V: risk factors and treatment / S.F. Galimova, M. Yu. Nadinskaya, M.V. Maevskaya // Clinical perspectives of gastroenterology, hepatology. - 2001. - #4. - P.2 - 6. |
| [18] | Gelfand B.R. Infusion-transfusion therapy in clinical medicine, - M., 2009. -256. |
| [19] | Klimovich I.N. Diagnosis of puti enlargement and treatment of hepatorenal syndrome and acute abdominal surgical pathology: Avtoref.dis. d.m.n.- Volgograd, 2007. -50s. |
| [20] | Clinical recommendations: Acute pancreatitis. Russian Society of Surgeons, Association of Non-Pancreatobiliary Surgeons of the CIS Countries. 2015. |
| [21] | Features of the course, clinical manifestations and tactics of surgical treatment of complications of gallstone disease in liver cirrhosis / F.G. Nazyrov, Kha. A. Akilov, A.V. Devyatoe, Sh.T. Urakov // Annaly of surgery. - 2001. - No. 2. - S. 68 - 70. |
| [22] | Evaluation of functional liver reserves and prediction of hepatic insufficiency during surgical treatment of patients with cirrhosis / V.A. Siplivyy. // Kharkov surgeon. school - 2005. - #1. - P. 262-265. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML