-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(11): 2711-2715
doi:10.5923/j.ajmms.20241411.06
Received: Oct. 9, 2024; Accepted: Nov. 1, 2024; Published: Nov. 7, 2024

Factors Leading of Obstructive Jaundice Syndrome and Its Complications in Ekderly Patient
Muhammadsohib Shavkatovich Kodirov1, Uktam Nurmamatovich Turakulov2, Shavkat Nomanovich Kodirov3
1Assistant, Department of General Surgery and Transplantology, Andijan State Medical Institute, Uzbekistan
2Republican Specialized Scientific-Practical Medical Center of Surgery named after Academician V. Vakhidov, Associate Professor, Doctor of Medical Sciences, Department of Surgery No.1, Center for the Development of Professional Skills of Medical Workers (CDPSMW)
3Doctor of Medical Sciences, Head of the Department of Endosurgery Endourology and Dentistry, Andijan State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study focuses on obstructive jaundice syndrome in elderly patients, a condition characterized by blocked bile flow, often due to gallstones, malignancies, or strictures. The elderly population is particularly susceptible to severe forms and complications of the syndrome due to age-associated physiological decline and multiple comorbidities. Key diagnostic methods include non-invasive imaging like ultrasonography and MRCP, as well as invasive techniques such as ERCP. These methods help identify the cause and guide treatment options, which range from minimally invasive procedures to surgical interventions. Complications such as cholangitis, liver failure, and sepsis are common, significantly impacting patient outcomes. The article discusses the importance of early diagnosis and personalized treatment strategies to manage the disease effectively and reduce associated risks. Understanding these factors is essential for optimizing therapeutic approaches and improving the quality of care for elderly patients with obstructive jaundice.
Keywords: Elderly patients, Minimally invasive methods, Obstructive jaundice must be included
Cite this paper: Muhammadsohib Shavkatovich Kodirov, Uktam Nurmamatovich Turakulov, Shavkat Nomanovich Kodirov, Factors Leading of Obstructive Jaundice Syndrome and Its Complications in Ekderly Patient, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2711-2715. doi: 10.5923/j.ajmms.20241411.06.
1. Introduction
- Obstructive jaundice is a severe condition frequently observed in elderly patients, often resulting from a variety of biliary and pancreatic disorders. With aging, anatomical, physiological, and pathological changes increase the vulnerability of the biliary system, leading to higher incidences of diseases that obstruct bile flow. This condition not only impacts the quality of life but also poses significant challenges in surgical treatment due to complications such as infection, cholangitis, and biliary cirrhosis. Recent studies indicate a rise in the prevalence of gallstones, tumors, and inflammatory diseases as primary causes of obstructive jaundice, highlighting the need for timely diagnosis and effective management strategies. In particular, the rising rate of iatrogenic injuries following laparoscopic procedures has added complexity to treating these patients. This paper aims to explore the underlying factors of obstructive jaundice in elderly patients, examine common complications, and provide insights into evolving treatment approaches based on current clinical data and global trends.In surgery, among liver and extrahepatic bile duct diseases, one of the most severe conditions is obstructive jaundice caused by blockage of the common bile duct [1]. Obstructive jaundice syndrome encompasses a large group of diseases and is clinically caracterized by increased bilirubin levels in the blood, resulting in yellow discoloration of mucous membranes, sclera, and skin due to impaired patency of the major bile ducts [2].Recent literature shows that patients with obstructive jaundice comprise 18-20% of cases within liver and bile duct diseases [3].
2. Methods
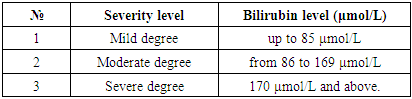
- Main Causes of Obstructive JaundiceThe primary causes of obstructive jaundice include:1) Anatomical anomalies (congenital conditions): common bile duct cysts, bile duct atresia, hypoplasia, and duodenal diverticula;2) Various benign conditions: choledocholithiasis, bile duct strictures due to inflammation, acute papillitis, and narrowing of the major duodenal papilla;3) Parasitic and inflammatory diseases: acute cholecystitis, cholangitis, acute and chronic pancreatitis, alveolar and echinococcosis;4) Tumors: cancer of the major duodenal papilla, pancreatic head cancer, lymphomas and metastases at the liver hilum, bile duct papillomatosis, and intrahepatic and extrahepatic bile duct cancer;5) Iatrogenic injuries to the bile ducts.Among the mentioned conditions, the main causes of obstructive jaundice are: choledocholithiasis, which accounts for 47-68%; pancreatic cancer and pancreatic diseases (acute and chronic pancreatitis, cysts) making up 23-33%; and tumors, both benign and malignant, of the major duodenal papilla and bile ducts, constituting 17%. For patients under 30, gallstone disease is primarily responsible for obstructive jaundice; for those aged 30-50, gallstone disease and tumors contribute equally; while in individuals over 55, tumor-related conditions predominate [4].The number of patients with obstructive jaundice is increasing globally, including in Uzbekistan [5]. According to research, gallstone disease has been identified in 10% of the world’s population [6]. Among these patients, 10-20% experience choledocholithiasis accompanied by obstructive jaundice. In the Commonwealth countries, the complication rate of choledocholithiasis with obstructive jaundice has doubled every decade. By the late 20th century, more than 5 million cases of gallstone disease were identified in Germany, while over 15 million patients in the United States were treated for gallstone disease, with 10% of cases occurring in the working-age population. Gallstone disease and its complication with obstructive jaundice are more commonly observed in women than in men, with a ratio ranging from 3:1 to 8:1 in some countries. The incidence increases with age, affecting up to 30% of individuals over 70.According to data from the World Health Organization, in recent years, there has been an observed increase in the incidence of tumors in the pancreatoduodenal region worldwide, with complications involving obstructive jaundice occurring in 50-80% of cases. In the United States, this indicator shows that bile duct cancer accounts for 20% over the past 25 years. In Italy, the incidence of cancer in the head of the pancreas has increased from 2.9% to 11.9%, equating to one in every 100,000 people. The increase in post-surgical obstructive jaundice after gallstone disease treatment is mainly due to iatrogenic injuries to the bile ducts, with 90% of these cases occurring following cholecystectomy (more frequently after laparoscopic cholecystectomy). Iatrogenic injuries often lead to cicatricial stenosis of the external bile ducts in 82-97% of cases. Following cicatricial stenosis, obstructive jaundice is observed in 70-92% of cases. The clinical manifestation of obstructive jaundice after iatrogenic injury to the common bile ducts can arise anywhere from a few days up to 10 years or even longer. Obstructive jaundice may lead to various purulent-septic complications, such as acute cholangitis, liver abscesses, and biliary sepsis in the abdominal cavity [7]. Obstructive jaundice is complicated by cholangitis in 20-40% of cases, often involving the proximal part of the bile ducts in up to 40% of cases.Obstructive jaundice is characterized by manifestations such as cholestasis, cholemia, and acholia.In cholestasis, there is an accumulation of hepatotoxic substances in the liver, leading to mitochondrial dysfunction and a breakdown of the liver cells’ antioxidant defense mechanisms. Mitochondrial dysfunction results in increased production of free radicals and oxidative stress. In cholemia, due to the relaxation of venous walls (vasodilation), peripheral resistance decreases, reducing the volume of circulating blood, which disrupts the function of the reticuloendothelial system. In acholia, pathogenic microbes accumulate in the small and large intestines, allowing bacteria and endotoxins to spread through the portal vein, triggering an inflammatory syndrome. Alongside liver changes, this condition causes pathological changes in blood circulation and hemodynamics within various organs and tissues.One of the main causes of renal failure is the decrease in blood flow to the kidney and glomerular apparatus, leading to bilirubin deposition in the renal tubules. A characteristic of obstructive jaundice is the reduction in the body’s energy metabolism, resulting in impaired glucose and substrate metabolism in various tissues and leading to hypoxia throughout the body, which significantly increases postoperative mortality due to these profound pathomorphological changes.Prolonged obstructive jaundice can cause liver and kidney failure, which disrupts the blood coagulation system and impairs the function of hepatocyte cells, weakening the body’s ability to combat infection, ultimately leading to the spread of infection within the bile ducts and throughout the body.Mortality rates following obstructive jaundice are reported to be as high as 20-60% according to various authors.One of the primary causes of mortality in patients with obstructive jaundice is liver failure and the development of endogenous infection. This condition arises from the accumulation of unsaturated fatty acids, lactate and pyruvate, bilirubin and bile acids, autolytic dead tissue, and enzymatic substances, as well as aromatic amino acids, carbohydrates, uremic toxins, cortical tissue, and ammonia, leading to metabolic disruption and accumulation of toxic substances in the body. Due to endogenous and exogenous factors, structural, morphological, and functional imbalances occur, reducing the number of immunocompetent cells and impairing their function, creating a cytokine system imbalance. Studies indicate that patients with obstructive jaundice exhibit an impaired immune system, leading to secondary immunodeficiency. The disintegration of the immune system significantly affects disease progression, and at various stages of treatment for obstructive jaundice, patients develop purulent inflammatory complications.In obstructive jaundice, liver failure differs from liver failure due to liver cirrhosis, often presenting subtly and in the form of encephalopathy.Thus, despite advances in medicine with new diagnostic methods and treatment options, obstructive jaundice remains a relevant and significant socio-economic issue.Currently, there are numerous classifications of obstructive jaundice, with recent classifications distinguishing two major groups based on etiological factors:A. Benign (congenital bile duct anomalies, choledocholithiasis, narrowing of the major duodenal papilla, pancreatitis, cystic changes in the pancreas, bile duct strictures due to scarring and trauma, duodenal diverticula, cholangitis, parasitic liver diseases, peri-choledochal lymphadenitis, duodenostasis).B. Malignant tumors (primary liver cancer, Vater’s papilla tumor, cancer of the pancreatic head, extrahepatic bile duct tumors, liver metastases).C. Obstructive jaundice can be classified based on its course: progressive, resorptive (intermittent)- suprahepatic obstructions (proximal block) - ultrasound examination reveals dilation of the intrahepatic bile ducts; there are no structural or volumetric changes detected below the obstruction in the intrahepatic bile ducts, and a relaxed gallbladder is observed.- subhepatic obstructions (distal block) - ultrasound examination shows dilation of the common bile ducts and an enlarged gallbladder with wall changes; in rare cases, changes in the intrahepatic bile ducts are detected.According to the classification suggested by many researchers, including E.I. Galperin (2014), the degrees of obstructive jaundice are categorized based on clinical laboratory tests, primarily according to the bilirubin levels in the blood:- Mild degree - up to 85 μmol/L- Moderate degree - from 86 to 169 μmol/L- Severe degree - 170 μmol/L and above.
|
3. Results and Discussion
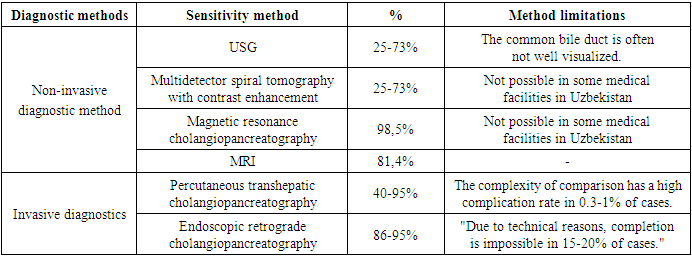
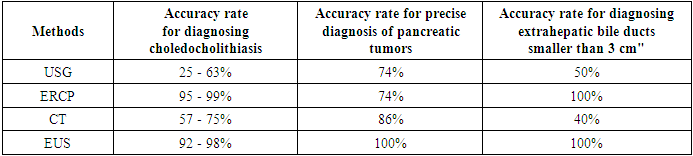
- Improving the characterization of obstructive jaundice is crucial in clinical practice and diagnostics to enhance surgical procedures, optimize their selection, and reduce postoperative complications. Over the past two decades, hepatobiliary surgery has achieved numerous breakthroughs in diagnosing obstructive jaundice, relying on technological advancements in modern medicine. However, even today, there are cases where the causes and treatment of obstructive jaundice cannot always be determined in modern surgery. Etiological gaps are still observed in 10-42% of cases of obstructive jaundice, leading to liver failure and the degradation of hepatocytes.In 54% of patients with obstructive jaundice, complications such as gastrointestinal bleeding, purulent cholangitis, liver abscesses, biliary sepsis, encephalopathy, and other adverse effects may be observed. Unfortunately, the mortality rate among patients after this condition remains high at 14-27% [8]. It is essential to note that in treating patients with obstructive jaundice, the severity of the disease, duration of jaundice, underlying cause, location of the mechanical obstruction, and comorbidities in the elderly are significant factors. Often, such patients, after ambulatory treatment, approach infectious disease hospitals without timely diagnosis, delaying their referral to surgical departments. By this time, their condition may have worsened, and they might experience bilirubinemia with two to three weeks of intoxication.Two primary factors contribute to diagnosing obstructive jaundice: identifying damage causing obstruction to the liver and the bile duct, and the obstructing factor. Examining the clinical manifestations and laboratory indicators of obstructive jaundice forms the basis for differentiating hyperbilirubinemia in 40-85% of patients. Table 2 and Table 3 provide details on non-invasive and invasive diagnostic methods for identifying the causes of obstructive jaundice, as well as shortcomings in studying sensitivity.It should be noted that for high-accuracy diagnosis of obstructive jaundice, the use of X-ray computed tomography, magnetic resonance imaging, ultrasound (US), and endoscopic examination methods is limited in many medical facilities. Considering these factors, ultrasound is usually the first method performed in diagnosing obstructive jaundice. This examination is highly informative due to its safety, the possibility of repeated use, and its minimal harmful effects.In ultrasound (US) examination for obstructive jaundice, one of the main indicators is the dilation of the bile ducts, which can appear in either a localized area or throughout the entire biliary tract [9]. Additionally, US allows clear visualization of the biliary obstruction's location, aiding in identifying its causes. This precision is crucial for surgical decision-making, helping determine the appropriate procedure and extent of surgery to remove the obstruction in the common bile duct.
|
|
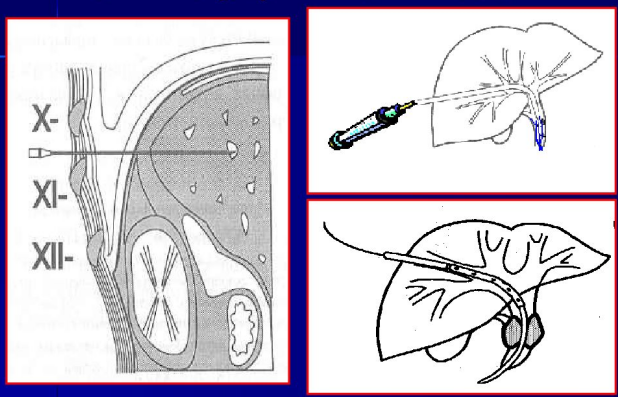 | Figure 1. Percutaneous transhepatic cholangiography (PTC) |
4. Conclusions
- Obstructive jaundice syndrome in elderly patients is associated with multiple complex factors, including bile duct obstructions due to stones, tumors, and anatomical variations, which are often compounded by age-related physiological changes. These factors contribute to a higher incidence of complications such as biliary infections, liver failure, sepsis, and gastrointestinal bleeding, which significantly increase morbidity and mortality rates in this population. Timely diagnosis through advanced imaging techniques, alongside tailored therapeutic strategies, is crucial for managing obstructive jaundice in elderly patients. Early intervention can reduce the severity of complications, improve patient outcomes, and decrease healthcare burdens associated with this condition in an aging population.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML