Saidzhalilova D. D., Madolimova N. Kh.
Department of Obstetrics and Gynecology, Tashkent Medical Academy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article discusses the impact of adenomyosis on the course of pregnancy and the risk of perinatal complications, such as premature birth, fetal hypoxia, intrauterine growth retardation, and placental insufficiency [9]. Adenomyosis is a disease characterized by the proliferation of the endometrium into the muscular layer of the uterus, which can lead to changes in its structure and functionality, especially during pregnancy [7]. The aim of the study is to study prognostic factors that allow early detection of the risks of complications in women with adenomyosis. The article also discusses modern methods of prevention aimed at minimizing adverse perinatal outcomes and provides recommendations for pregnancy management in the presence of adenomyosis, taking into account the individual characteristics of patients and the use of the latest therapeutic approaches.
Keywords:
Adenomyosis, Perinatal complications, Pregnancy, Prognosis, Prevention, Premature birth, Fetal hypoxia, Placental insufficiency, Intrauterine development
Cite this paper: Saidzhalilova D. D., Madolimova N. Kh., Adenomyosis and Perinatal Complications, Their Prognosis and Prevention, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2701-2706. doi: 10.5923/j.ajmms.20241411.04.
1. Introduction
Relevance and relevance of the dissertation topic. WHO recognizes the significance of the problem of endometriosis and its negative impact on the reproductive health, quality of life and overall well-being of women. Endometriosis affects approximately 10-15% of women of reproductive age worldwide (WHO 2021), up to 50% of women among them are diagnosed with infertility. According to WHO estimates (WHO, 2023), at least 190 million women and adolescent girls worldwide currently suffer from this disease during reproductive age, although some women may suffer after menopause. Addressing these issues is currently the main objective of efforts to combat endometriosis.If the monthly fertility rate of healthy women of reproductive age is 15-20%, then endometriosis reduces it many times: to 2-10% [4]. In addition, 30-50% of women with this disease cannot bear a child even if pregnancy occurs. Achieving favorable gestational and perinatal outcomes in women with adenomyosis is an extremely important task. Over the past decades, studies have been conducted to study the relationship between endometriosis and adverse pregnancy outcomes for the mother and fetus [2,8]. There is evidence that absolute regression of endometrioid foci does not occur during gestation. Nevertheless, to fully understand the pathophysiological subtleties, we turned to evidence-based data.Children born to mothers with deep foci of endometriosis were more often born prematurely and underweight than in the control group. The results of the study by colleagues Fujii T., Wada-Hiraike O., Nagamatsu T. from Japan (2016) were quite interesting. A higher rate of miscarriage was recorded in patients with adenomyosis. In 2017, Zullo F. et al. published a meta-analysis of 24 studies involving 1.9 million women. They showed that cases of abnormally located placenta, SORP and cesarean section were higher in pregnant women with endometriosis, but no increase in the incidence of pregnancy-induced hypertension (PIH) or PE was found. The meta-analysis showed that the incidence of preterm birth and malposition of the placenta were higher in pregnant women with endometriosis both in natural conception and in the ART groups [3].Russian researchers Adamyan L.V. and her team (2022) found that every fourth woman with endometriosis (23.6%) suffers from habitual miscarriage, and in most of them (97.2%), gestation is interrupted in the first trimester [1].The above allows us to conclude that women of reproductive age with endometriosis need a special approach to planning and managing pregnancy, as well as those who, due to endometriosis-associated infertility, make numerous and unsuccessful attempts to become pregnant [6].From the standpoint of a systemic approach, taking into account significant parameters, this task has not been solved in Uzbekistan before. The absence of prognostic criteria for the pathological course of pregnancy in adenomyosis seems to be the most important unsolved problem, on which the choice of pregnancy management tactics largely depends.The aim of the study is to determine the pathogenetic role of adenomyosis in the development of obstetric and perinatal complications for the development of a method for pregravid preparation and prediction of complications during gestation.
2. Materials and Methods of the Study
The study was conducted in several stages. At the first stage, in order to determine the frequency and structure of obstetric and perinatal complications in 103 women with various forms of adenomyosis aged 25 to 35 years (average age - 29.6 ± 4.2 years), who underwent outpatient treatment in the department of the polyclinic of the 9th obstetric complex and the private clinic NS Medical, Tashkent for the period from 2021-2023. Depending on the form of adenomyosis, women were divided into groups: Group 1 consisted of 82 women with diffuse adenomyosis, including 69 women with AM grade 1-2 and 13 women with AM grade 3; Group 2 - 21 women with focal adenomyosis. The control group consisted of 112 women without adenomyosis.At the second stage after the therapy of adenomyosis there was pregnancy planning. When pregnancy occurred in 66 (64.1%) of the studied women with adenomyosis, the level of trophoblastic β-1-glycoprotein was determined in the dynamics of gestation, with various obstetric and perinatal complications and its prognostic significance was determined. Depending on the management, the pregnant women were divided into subgroups. Subgroup 1 consisted of women (n = 45), of which 34 women had the diffuse form of AM and 11 with the focal form, who were prescribed micronized progesterone at a dose of 400 mg per day until the 16th week of pregnancy and acetylsalicylic acid 75 mg per day from the 12th to the 36th week of pregnancy as a preventive measure against gestational complications. Subgroup 2 consisted of pregnant women (n = 21), of which 13 women had the diffuse form of AM and 8 with focal AM, who were managed traditionally. The comparison group consisted of 42 pregnant women without adenomyosis.Clinical methods of examination included collection of anamnesis with study of patient complaints, assessment of menstrual and reproductive function, study of pregnancy and childbirth outcomes, somatic and gynecological anamnesis data. In some cases, according to special indications, patients consulted related specialists. Objective examination included examination, gynecological examination with determination of the form and severity of adenomyosis. Study of the level of trophoblastic β-1-glycoprotein was performed in blood serum in the dynamics of gestation.The obtained data were statistically processed using the applied programs for mathematical and statistical analysis "IBM SPSS Statistics 23". Statistical methods included: determining the mean value of the sample (M), the standard error of the mean (m), the reliability of differences - according to the Mann-Whitney criterion. The level of reliability p<0.05 was taken as statistically significant changes.
3. Research Results
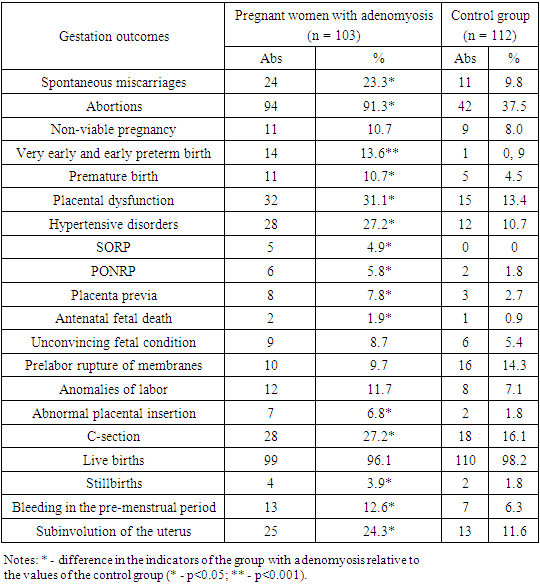
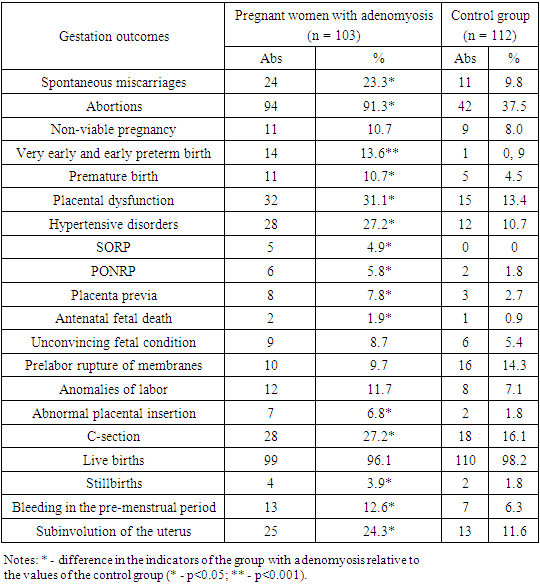
The study of the reproductive history showed that women with a history of adenomyosis had the fourth pregnancy in 12.6% and the third birth or more in 19.4%, which is 2 and 3.1 times less in the control group, respectively. Artificial abortions (Table 1) were performed by patients in all clinical groups. Analysis of the abortion frequency in the group of women without adenomyosis showed lower rates (37.5%). Spontaneous termination of pregnancy in patients with adenomyosis was noted in 23.3% of patients, which was 2.4 times more often than in the control group (9.8%). The most frequent complications of the second half of pregnancy were very early and early premature births, the frequency of which in the group of women with adenomyosis was 13.6%, which is 15.1 times higher than in the control group. The incidence of premature birth was 24.3% in the group of pregnant women with adenomyosis, which is 4.5 times more common than in women without adenomyosis (5.4%). Pregnant women with adenomyosis had a history of significantly high incidence (31.1%) (p<0.05) of placental dysfunction and hypertensive disorders – 27.2%. It is well known that one of the outcomes of placental dysfunction is PORP, which was noted in 4.9% of women with adenomyosis. This pathology was not observed in the group of women without adenomyosis. Such serious pregnancy complications as PONRP and placenta previa were noted in 5.8% and 7.8% of women with adenomyosis, respectively. Whereas in the control group of women without adenomyosis they were 1.8% and 2.7%, respectively, which was 3.2 and 2.9 times more frequent.Table 1. Outcomes of previous pregnancies in women with adenomyosis
 |
| |
|
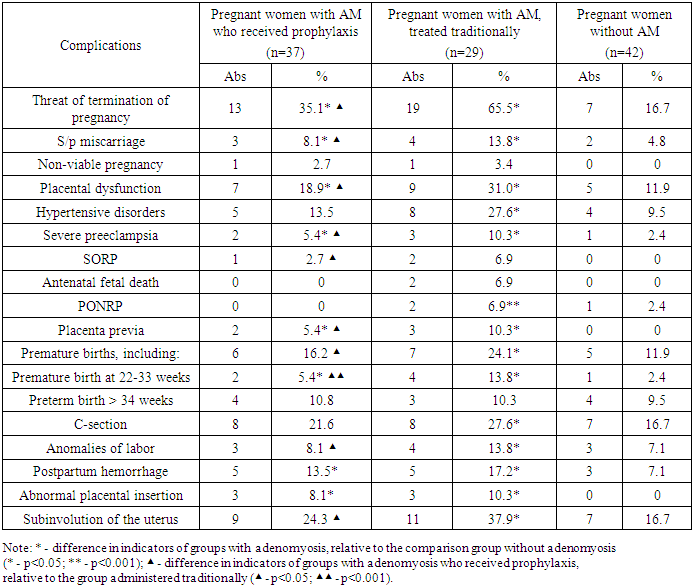
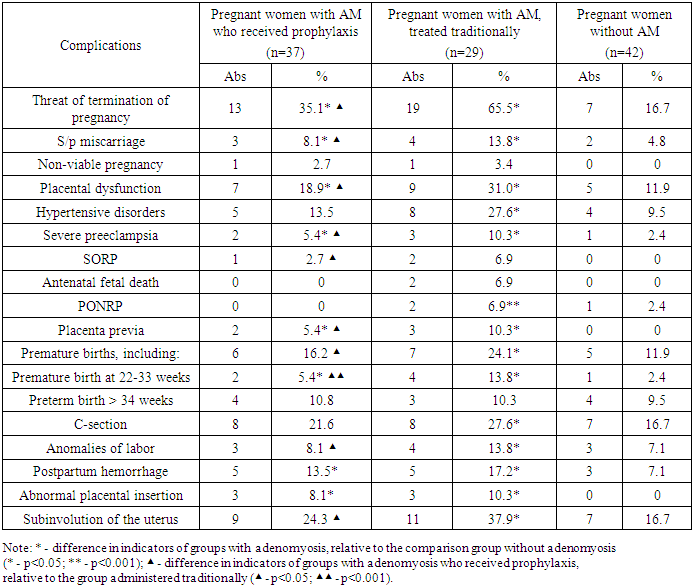
A study of the course of labor in the anamnesis of women with adenomyosis showed a higher frequency of complications such as weakness of labor - 11.7% of women in labor; dense placental attachment - 6.8% (p < 0.05), 3.7 times higher than the general population indicator and the indicator of the control group (1.8%); hypotonic bleeding in the early postpartum period - 12.6%, subinvolution of the uterus - 24.3%.Thus, the frequency of complications of the gestational period, childbirth and postpartum period in women with adenomyosis was 62.1%, which is 3.4 times more often than in women without adenomyosis (17.9%). We have found that the chances and risks of developing obstetric and perinatal complications are significantly increased in pregnant women with adenomyosis. The identification of a group with an unfavorable prognosis is the basis for defining these women as a high-risk group for developing obstetric and perinatal complications during subsequent pregnancies and implementing appropriate treatment and preventive measures in them. The chances and relative risk of developing obstetric complications are high in women with adenomyosis, the structure of which consisted of: spontaneous miscarriages (OR = 2.8; RR = 2.4), very early and early premature births (OR = 17.5; RR = 15.6), premature births (OR = 2.6; RR = 2.2), placental dysfunction (OR = 2.9; RR = 2.4), hypertensive disorders (OR = 3.1; RR = 2.5); SORP (OR = 5.7; RR = 5.6), placenta previa (OR = 3.1; RR = 2.7) and abnormal placental attachment (OR = 4.0; RR = 3.5), as well as bleeding in the postpartum period (OR = 2.2; RR = 2.1) and subinvolution of the uterus (OR = 2.4; RR = 2.0).Given the high rate of adenomyosis recurrence (32.4%) after traditional therapy, we decided to improve the method of introducing women with this pathology. At stage I, adenomyosis therapy was performed with dienogest-containing COCs (Zhanin, diaenogest 2 mg/day) for 6 months (for greater leveling of foci and contraception) in combination with the drug Indole-3-carbinol (I3C) in a continuous mode (200 mg/day) for a year/until pregnancy, affecting another epigenetic link in the pathogenesis of adenomyosis. Indole-3-carbinol (I3C) is a substance of natural origin with antitumor specific epigenetic activity. In adenomyosis, the mechanism of indole-3-carbinol is to reduce estrogen-dependent and estrogen-independent proliferation, suppress inflammation, stimulate apoptosis, stabilize the genome by inhibiting DNA methylation and suppressing DNA methyltransferase, and suppress proliferation and neoangiogenesis processes [10].The evaluation of the effectiveness of the treatment of adenomyosis was based on such indicators as the pain and duration of menstruation, Doppler parameters of the uterine vessels, the frequency of pregnancy, the course and complications of subsequent pregnancy [5].The next stage of the study was pregnancy planning with the elimination of pathology symptoms and improvement of blood circulation in the uterine vessels after the treatment of adenomyosis. In order to reduce the recurrence of adenomyosis after the end of therapy with dienogest-containing COCs, we prolonged therapy with indole-3-carbinol in a continuous mode (200 mg/day) for another 6 months, or until pregnancy (if it occurred earlier), as well as progesterone support during pregnancy to prevent obstetric complications during pregnancy.Within a year after the end of therapy, 66 out of 103 women (64.1%) became pregnant, while with the diffuse form of adenomyosis, pregnancy occurred in 47 out of 82 women (57.3%), which is 1.6 times less often than with focal adenomyosis (90.5%) (19 out of 21).To prevent miscarriage in women with adenomyosis, micronized progesterone was prescribed at a dose of 400 mg per day until the 16th week of pregnancy and acetylsalicylic acid 75 mg per day from the 12th to the 36th week of pregnancy.Depending on the management, 66 pregnant women with AM were divided into groups. Group A consisted of 37 women who received prevention of complications, including 26 women with diffuse AM and 11 women with focal AM. Group B consisted of 21 women who did not receive prevention of complications, including 21 with diffuse AM and 8 with focal AM.Analysis of the pregnancy course in women with adenomyosis showed that in the group of pregnant women who received prophylaxis, a more favorable pregnancy course was noted, as evidenced by a smaller number of gestation complications than in the group without prophylaxis of complications (Table 2). In women with adenomyosis, the threat of miscarriage was observed in more than half of the women (65.5%), whereas in pregnant women with prophylaxis, the threat was 1.9 times less (35.1%). The threat of termination of pregnancy was complicated by spontaneous miscarriages and premature births in 13.8% and 24.1% of women with adenomyosis, who were treated traditionally, and were higher than the rates of pregnant women with prophylaxis by 1.7 (8.1%) and 1.5 (16.2%) times. A distinctive feature of pregnant women with adenomyosis, managed traditionally, was the presence of a greater number (13.8%) of very early and early premature births, the frequency of which was 2.6 times higher than in the group of women receiving prophylaxis.Table 2. Features of the course of pregnancy in women with adenomyosis, depending on the management
 |
| |
|
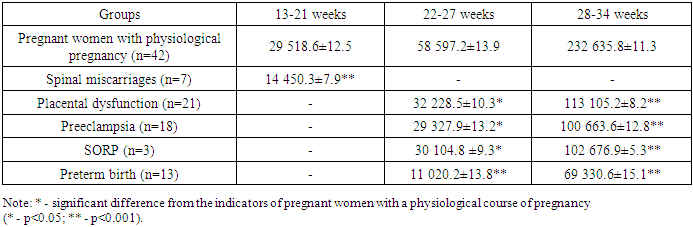
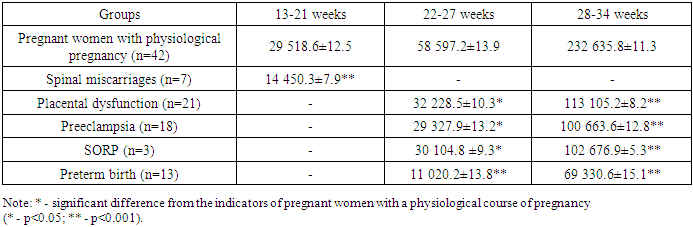
Placental dysfunction with impaired fetal hemodynamics was observed in the group of pregnant women with adenomyosis in 31.0% of pregnant women, which exceeded the values in the group of women receiving prophylaxis by 1.6 times (18.9%) and in the group of women without adenomyosis by 2.5 times (12.2%).In pregnant women with adenomyosis, without prophylaxis of obstetric complications (Table 2), a significant (p<0.05) increase in the frequency of hypertensive disorders was noted – 27.6% with the development of severe preeclampsia in 10.3% of women. Whereas this complication in the group of women with adenomyosis who received prophylaxis (13.5%) was 2 times less frequent and did not differ from the indicators of the control group (10.9%).It should also be noted that antenatal fetal death (6.9%) was observed only in the group of women with adenomyosis who did not receive prophylaxis. Such serious obstetric pathologies as placenta previa and placenta previa were more often observed in the group with adenomyosis who were not managed comprehensively, and accounted for 6.9% and 10.3%, respectively. Placenta previa was also observed in the group of women who received indole-3 carbinol and prophylaxis, but 1.9 times less frequently (5.4%).The study of the course of labor showed that 13.8% of women in labor with adenomyomas developed weakness of labor, which is 1.7 times more common than the indicators of the group receiving indole-3-carbinol and prevention of gestational complications. The postpartum period in women with adenomyosis was also characterized by high rates of uterine subinvolution (37.9%), which was 1.6 times higher than the indicators of the group of women with adenomyosis treated comprehensively (24.3%).The frequency of timely births was significantly higher in the group of women with adenomyosis who received indole-3 carbinol before pregnancy and micronized progesterone and acetylsalicylic acid before 16 weeks of gestation (χ2=6.37; P<0.05), while the frequency of premature births was significantly lower by 1.5 times (χ2=3.52; P<0.02), and the frequency of fetal loss by more than 1.5 times (χ2=3.69; P<0.05).Taking into account all of the above, the advantage of a comprehensive approach to the management of pregnant women with adenomyosis, based on treatment with the prevention of relapses (indole-3 carbinol) and complications of gestation (micronized progesterone and acetylsalicylic acid), becomes clear [5].Due to the non-specificity of clinical manifestations of pregnancy complications against the background of adenomyosis, preclinical diagnostics of pathology during pregnancy is difficult. One of the methods for predicting complicated gestation before its clinical manifestation is determining the level of trophoblastic β-1–glycoprotein (TBG) in the blood of pregnant women. We examined pregnant women of the main group (n=66), which were divided into subgroups depending on the management: subgroup 1 consisted of 37 pregnant women with adenomyosis, who received prophylaxis with micronized progesterone and acetylsalicylic acid, and subgroup 2 – 29 pregnant women with adenomyosis, who were traditionally managed. The comparison group - 42 pregnant women without adenomyosis.In the development of the threat of premature birth (TPB) in pregnant women with adenomyosis, even with prophylaxis, the concentration of TBG was 25859.1±9.3 ng/ml, which was 2 times lower than the values in the group with the physiological course of gestation. Whereas in the development of TPB in pregnant women without prophylaxis of complications, the level of TBG sharply decreased by 3.6 times and was 11020.2±13.8 ng/ml (Table 3). A strong inverse correlation (r=-0.95, p=0.0034) was established between the level of TBG at 32-34 weeks and clinical symptoms of termination of pregnancy. In the group of pregnant women with the threat of premature birth due to adenomyosis, who received conservation therapy, after the elimination of the symptoms of the threat of labor, the level of TBG was up to 103995.9±15.1 ng/ml, but did not reach the values of the group without TPB.Table 3. Changes in the level of trophoblastic β-1–glycoprotein in the development of pregnancy complications (ng/ml)
 |
| |
|
Despite the preservation therapy, 24.1% of pregnant women in the main group with adenomyosis developed premature birth, and 16.2% of women with adenomyosis who received prophylaxis, which is 1.5 times less often. Therefore, by changing the level of TBG in patients with the threat of premature birth, it is possible to judge the effectiveness of the preservation therapy, which is confirmed by the data of the correlation analysis (r = 0.85, p = 0.019).The study of TBG during labor showed a sharp decrease in its level, which averaged 72698.7±6.3 ng/ml, which was 3.2 times lower than the values before labor. This can be explained by premature reduction of the placenta observed during premature labor. At the same time, in pregnant women with adenomyosis, the processes of placenta reduction were significant than in the group with preterm labor without adenomyosis.The study of the TBG level in other gestation complications established the dependence of the marker level on the type of obstetric and perinatal complications and the gestational age. At the same time, in the sequence of the dynamics of the decrease in TBG in the blood serum of pregnant women with various complications, the degree of expression of the indicators were distributed in the following order: 1st place was taken by spontaneous miscarriages and premature births, 2nd place - SORP and PE, 3rd place - placental dysfunction. This in turn will allow, based on the study of the TBG level, to predict obstetric complications in women with adenomyosis at the preclinical stage.
4. Conclusions
1. The frequency of obstetric and perinatal complications in adenomyosis was 62.1% and the most common were spontaneous abortions (23.3%), placental dysfunction (31.1%), hypertensive disorders (27.2%), premature birth (24.3%), placenta previa (7.8%), perinatal losses (29.1%), as well as postpartum hemorrhage (12.6%), subinvolution of the uterus (24.3%).2. The odds and relative risk of developing obstetric complications are high in women with adenomyosis, the structure of which included: spontaneous abortions (OR = 2.8; RR = 2.4), very early and early preterm labor (OR = 17.5; RR = 15.6), preterm labor (OR = 2.6; RR = 2.2), placental dysfunction (OR = 2.9; RR = 2.4), hypertensive disorders (OR = 3.1; RR = 2.5); placenta previa (OR = 5.7; RR = 5.6), placenta previa (OR = 3.1; RR = 2.7) and abnormal placental attachment (OR = 4.0; RR = 3.5), as well as postpartum bleeding (OR = 2.2; RR = 2.1) and uterine subinvolution (OR = 2.4; RR = 2.0).3. A direct correlation was found between the level of trophoblastic β-1–glycoprotein in the blood serum of pregnant women and the development of gestational complications in women with adenomyosis. When the values of trophoblastic β-1–glycoprotein are below the standard values at the corresponding time periods (13-22 weeks – 29,518.6±12.5 ng/ml, 23-24 weeks – 58,597.2±13.9 ng/ml, 32-33 weeks – 232,635.8±11.3 ng/ml), the risk of spontaneous abortion and placental dysfunction is predicted to be 2 times; preeclampsia and PORP – 2.3 times; the development of very early and early premature labor – 5.3 times and premature labor – 3.6 times (p<0.001). The proposed method gives a probability of a correct prognosis in the 2nd trimester of 90%, in the third trimester - up to 95.5% of cases.4. Among the pathomorphological signs of pregnancy complications in women with adenomyosis, clearly interconnected processes leading to placental destruction stand out. Characteristic changes in placentas during the development of pregnancy complications against the background of adenomyosis were placental hypoplasia, acute and chronic circulatory disorders, dystrophic and ischemic processes, as well as marginal attachment of the umbilical cord in combination with false nodes of the umbilical cord.5. Comprehensive pre-conception preparation with epigenetic therapy due to the leveling of foci of adenomyosis and preclinical prediction and prevention of complicated pregnancy reduced the frequency of complications of pregnancy and childbirth (χ2=6.37; P<0.05), the frequency of premature births by 3 times (χ2=3.52; P<0.02) and perinatal fetal loss by more than 3 times (χ2=3.69; P<0.05).
References
| [1] | Adamyan L.V., Serov V.N., Sukhikh G.T., Fillipov O.S. Clinical recommendations. Obstetrics and gynecology. Endometriosis: diagnosis, treatment and rehabilitation. // Problems of reproduction. - 2017. No. 6. - P. 553-605. |
| [2] | Zayratiants O.V., Andreeva E.N., Adamyan L.V., Sonova M.M., Urumova L.T., et al. Endometriosis: new experience of non-hormonal drug therapy. // Problems of reproduction. - 2018. No. 24(6). P. 113-120. https://doi.org/10.17116/repro201824061113. |
| [3] | Mogilnaya G.M., Kutsenko I.I., Simovonik A.N. Morphometric characteristics of cell nuclei in the myometrial transition zone in adenomyosis. // Kuban Scientific Medical Bulletin. - 2016. - No. 3. – P. 88-91. https://doi.org/10.25207/1608-6228-2016-3-88-91. |
| [4] | Orazov M.R. Going through the volumes. Management of patients with endometriosis: updated ESHRE guideline (2022): Fact sheet / M.R. Orazov, O.A. Raevskaya, V.S. Moskvicheva; edited by V.E. Radzinsky - M.: Editorial office of the magazine Status Praesens, 2022. - 16 p. |
| [5] | Saidjalilova D.D., Madolimova N.Kh. Complications of pregnancy and childbirth in patients with endometriosis // XVI International Congress on Reproductive Medicine, 2023, 191-192 Berlac J.F., Hartwell D., Skovlund C.W., Langhoff-Roos J., Lidegaard Q. Endometriosis increases the risk of obstetrical and neonatal complications. // Act. Obstet. Gynecol. Scand. 2017. Vol. 96(6). P. 751-760. https://dx.doi.org/10.1111/aogs.13111. |
| [6] | Hamdan M., Omar S.Z., Dunselman G., Cheong Y. Influence of endometriosis on assisted reproductive technology outcomes: a systematic review and meta-analysis // Obstet. Gynecol. - 2015. - Vol. 125. № 1. - P. 79-88. https://dx.doi.org/10.1097/AOG.0000000000000592. |
| [7] | Еxacoustos C, Lauriola I, Lazzeri L, De Felice G, Zupi E. Complications during pregnancy and delivery in women with untreated rectovaginal deep infiltrating endometriosis. Fertility and Sterility. 2016; 106(5): 1129-1135. e1. https://doi.org/10.1016/j.fertnstert.2016.06.024. |
| [8] | Leyendecker G., Kunz G., Kissler S., Wildt L. Adenomyosis and reproduction. // Best Practice & Research Clinical Obstetrics & Gynaecology. 2016; 20: 523–546. |
| [9] | Petraglia F, Arcuri F, de Ziegler D, Chapron C. Inflammation: alink between endometriosis and preterm birth. // Fertil.Steril. 2018; 98. |
| [10] | Saidjalilova D.D., Madolimova N.Kh., Ayupova D.A. Influence of endometriosis in course of pregnancy and childbirth // Tibbiyotda yangi kun, 8(46), 2022, 74-78. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML