-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2668-2671
doi:10.5923/j.ajmms.20241410.46
Received: Aug. 29, 2024; Accepted: Sep. 22, 2024; Published: Oct. 29, 2024

Surgical Treatment of Non-Specific Spondylitis Using Osteoinduction Materials and Stabilizing Systems of the Lumbar Spine
Abdiev Sh. E., Sattarov A. R., Kobilov A. O., Saidov S. S.
National Center for Rehabilitation and Prosthetics for Persons with Disabilities, Tashkent, Uzbekistan
Correspondence to: Saidov S. S., National Center for Rehabilitation and Prosthetics for Persons with Disabilities, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The material of our work was made up of patients operated on for non-specific spondylitis of the spine of the lumbar spine at the National Center for Radiological and Psychiatric Surgery of the Ministry of Health of the Republic of Uzbekistan in the Self-supporting Department in the period 2018-2022. All patients underwent decompressive-stabilizing operations using titanium transpedicular fixation systems. In our practice, there were mainly hemolytic staphylococcal infections. Decompressive-stabilizing operations gave patients the opportunity for early activation and reduced hospital stay.
Keywords: Nonspecific spondylitis, Decompressive and stabilizing operations, TPF systems, Ceftriaxone REO, Ciprofloxacin, Aviflox
Cite this paper: Abdiev Sh. E., Sattarov A. R., Kobilov A. O., Saidov S. S., Surgical Treatment of Non-Specific Spondylitis Using Osteoinduction Materials and Stabilizing Systems of the Lumbar Spine, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2668-2671. doi: 10.5923/j.ajmms.20241410.46.
1. Relevance
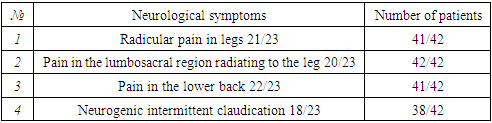
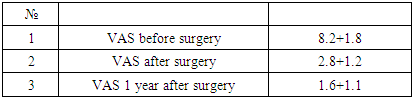
- Inflammatory diseases of the spine (spondylitis) can occur after any common infectious disease. Spondylitis are primary and secondary, can be acute and chronic. In the clinical picture of spondylitis, there are significant differences due to the localization of the inflammatory process in the spine and the prevalence of bone destruction. The most common symptom is pain and fever, followed later by neurological and septic complications.Spondylitis can be nonspecific (purulent), caused by various bacteria and specific (tuberculosis, syphilis, gonorrhea, actinomycosis, brucellosis).Hematogenous osteomyelitis of the spine (spondylitis) is a serious disease that is difficult to recognize, often at a later date, when destruction (destruction) of the vertebral bodies is already taking place. Most often, the lesion is located in the thoracic and lumbar spine, rarely in the cervical. Damage to the vertebral bodies, and sometimes the arches, can occur as a metastasis in furunculosis, tonsillitis, dental caries, after operations on the abdominal cavity, kidneys and pelvic organs. Local infection has been observed during lumbar spinal block, lumbar puncture, anesthesia, and disc surgery.For the diagnosis of spondylitis, radiography, computed tomography, magnetic resonance imaging, scintigraphy, and laboratory data are used.For radical treatment, a surgical operation is necessary – posterior internal fixation of the spine, and in case of severe destruction of the vertebrae and the formation of purulent streaks, anterior operations with resection of the vertebral bodies and sanitation of the pathological focus. In the future, antibiotic therapy and dynamic observation are carried out. Unfortunately, the refusal of active surgical tactics of treatment sometimes leads to irreparable complications.The urgency of the problem of treatment of nonspecific osteomyelitis of the spine is explained by the increase in the frequency of this type of pathology over the past decades, the emergence of new clinical forms of infectious lesions of the spine, new antibiotic-resistant strains of microorganisms, as well as the severity of the course and high rates of unsatisfactory anatomical and functional outcomes.In the section of surgery devoted to surgical infection, one of the leading places, due to the difficulties of diagnosis, the severity of the course, the complexity of the radical sanitation of the purulent focus, the peculiarities of the location of the spine surrounded by vital anatomical structures and adverse outcomes, is given to hematogenous osteomyelitis of the spine, ranging from 2 to 12% of all forms of acute hematogenous osteomyelitis of bones. Vertebral osteomyelitis is more common in men, with a male to female ratio of 1:5–2:1 [7]. The number of patients with osteomyelitis of the spine in the population ranges from 2 to 4 cases per 100 thousand people. in year. However, some authors believe that the number of cases is currently increasing, which is due to two factors: an increase in the susceptibility of the population and a large number of identified patients due to better diagnostics [4]. A distant focus of infection in hematogenous osteomyelitis is identified in less than half of the cases. According to E. Mylona et al., infections of the genitourinary system, skin, gastrointestinal tract, respiratory system, and oral cavity are most common. Other predisposing factors often cited by researchers include diabetes mellitus, injecting drug use, malignancy, renal failure, rheumatological disease, cirrhosis of the liver, and previous spinal surgery [1].Undoubted success in the treatment of nonspecific osteomyelitis of the spine associated with the use of antibiotics. Changed the structure of lesions of nonspecific inflammatory diseases of the spine. There are more patients among the elderly, and the clinical picture has become more blurred, much more often there is a subacute or chronic course with minimal symptoms or without them at all [5,7]. According to the results of epidemiological studies in recent years, the composition of osteomyelitis pathogens has changed significantly, there has been a tendency to increase the number of patients with hematogenous osteomyelitis caused by gram-negative microflora - Enterobacter., Pseudomonas aeruginosa, etc., pathogens related to opportunistic microflora (E coli, Staph, epidermidis, etc.) [1,7]. In connection with the widespread use of computed tomography (CT), magnetic resonance imaging (MRI), skeletal scintigraphy, the possibilities of diagnosing spondylitis have significantly expanded. However, many problems related to the early diagnosis and treatment of hematogenous osteomyelitis of the spine are still far from satisfactory resolution. So, according to most researchers, the average time to make a diagnosis after the onset of the disease is 3 months, and the percentage of diagnostic errors reaches, according to various data, from 30 to 85 [2,3,6,8]. The results of a study of large groups of patients showed that when installing multi-axial structures, the frequency of bone fusion does not differ from that in the study of systems with a fixed screw position [1]. The complications associated with installing multi-axis systems are identical to those associated with installing mono-axial systems. The screw spin frequency is similar for both systems. This is more common in designs with a shorter length by 2 segments (screws) [1]. Multi-axis systems are most useful for multi-level stabilizations that use 3 or more screws on the same rod. In such cases, these systems allow the screw to be positioned in the most secure and secure connection to the rod. The need for rod contouring is reduced, each screw can be placed parallel to the upper endplate, which allows maximum fixation of the screw in the vertebral body and minimizes the aggravation of neurological symptoms [1].The aim of the work is to improve the results of surgical treatment of nonspecific spondylitis of the lumbar spine with the use of osteoinductive materials and the use of TPF systems.Materials and methods - the material of our work was 42 patients operated on at the National Center for Radiological and Psychiatric Surgery of the Ministry of Health of the Republic of Uzbekistan in the Self-supporting Department in 2018-2022 for non-specific spondylitis of the lumbar spine of the lumbar spine. The material included 20(47,6%) women and 22(52,4%) men. The average age of the patients was 48,1±1,9 years. The indications for surgical treatment were the presence of pain, conduction and segmental disorders, and the presence of bone destruction of the vertebral bodies. Nonspecific spondylitis of the lumbar spine occurred in all 42 patients. All patients underwent decompressive-stabilizing operations from the posterior approach of the lumbar spine.Spondylitis consisted of decompression of the neurovascular structures of the spinal canal by interlaminectomy, discectomy (in the presence of discitis) with sanitation of the inflammatory focus, followed by stabilization of the TPF system; spondylodesis with MESh (filled with bongraft) followed by TPF stabilization with systems of consisting and multi-axial screws from the posterior and anterolateral approaches. In neurology, there was radicular pain in 41 patients, pain in the lower lumbar region transmitted to the leg in 42 patients, pain in the lower back in 42 patients and neurogenic intermittent claudication in 38 patients. Stabilization was carried out at two levels for 18 patients and the rest of the patients at three levels. Clinical manifestations are presented in table 1.
|
2. Results and Its Discussion
- All patients received good results and stable stability immediately in the postoperative period, which allowed them to be activated early. When conducting control postoperative radiological studies, we found a strong stabilization of the operated segment of bone formations and no signs of residual inflammation. When conducting control radiographic studies after 12 months. The position of MESh and multiaxial transpedicular systems was stable. The systems ensured reliable immobilization of stabilized spinal segments. Damage to the TPF systems did not occur in more than one observation, we never detected displacement of screws from the vertebral bodies.Clinical result in patients after surgery, one patient had reflex pain, which was stopped with muscle relaxants, 9 patients had moderate pain (the patient periodically took painkillers), the rest of the pain disappeared and the patients returned to an active lifestyle. Results in the postoperative period: good results in 29 (69.05%) patients, satisfactory in 13 (30,95%) patients.
|
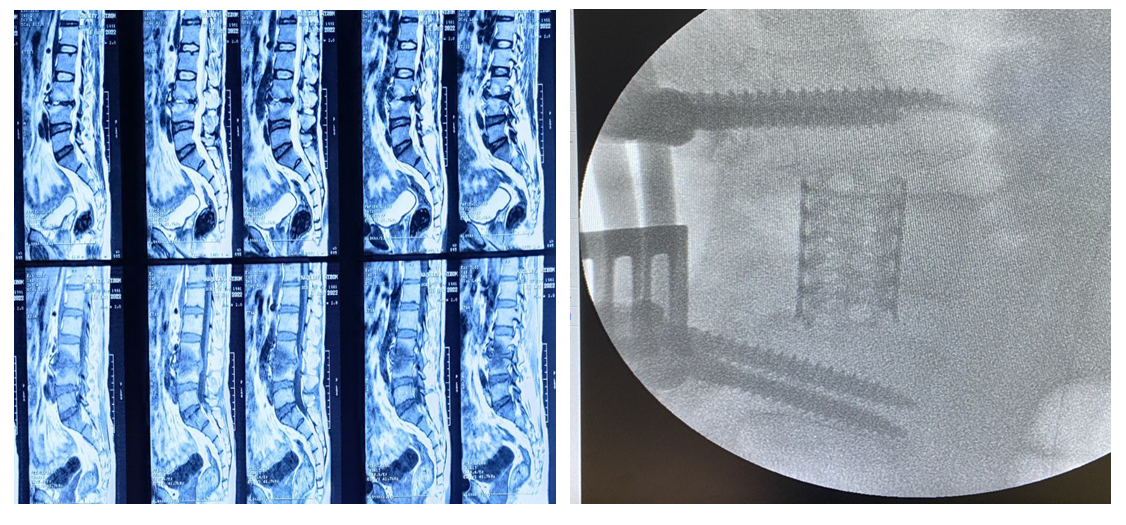
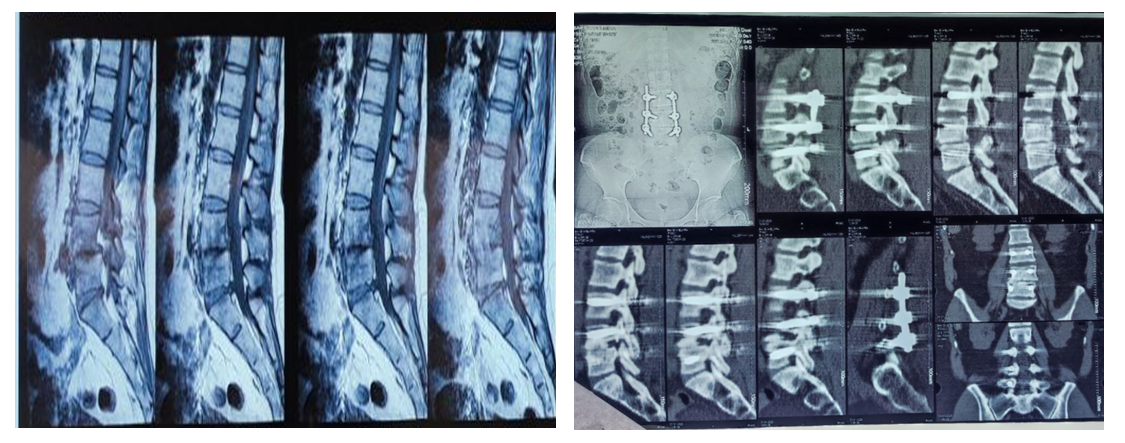 | Figure 1. Patient A 51l Spondylodiscitis at the level of VL4-5, operated on for the stabilization of the TPF system at the level of VL3-4-5 on both sides |
3. Conclusions
- Corporectomy with debridement of the inflammatory focus and MESh fusion (filled with a bongraft) and stabilization with a TPF system (multi-axial screws) makes it possible to diversify the position of the screws. This feature minimizes the need for rod contouring, reduces metal fatigue, reduces operating time, and makes it possible to thoroughly sanitize the inflammatory focus and early activation of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML