-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2663-2667
doi:10.5923/j.ajmms.20241410.45
Received: Oct. 8, 2024; Accepted: Oct. 22, 2024; Published: Oct. 28, 2024

Issues of Diagnosis, Treatment and Rehabilitation of Patients with Alcohol Intoxication in the Post-Intoxication Period
Khusenov O. N.1, Stopnitsky A. A.2
1Department of Internal Medicine, Bukhara State University, Bukhara, Republic of Uzbekistan
2Senior Researcher, Scientific and Clinical Department of Toxicology, Republican Scientific Center for Emergency Medical Care, Tashkent, Republic of Uzbekistan
Correspondence to: Khusenov O. N., Department of Internal Medicine, Bukhara State University, Bukhara, Republic of Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: to study the effectiveness of the developed scoring system for early diagnosis of cognitive and metabolic disorders, as well as a complex of drug hepatoprotective therapy and psychosocial correction in patients with alcohol intoxication during the post-intoxication period. Materials and methods: We examined 280 patients aged 18 to 60 years who were admitted with alcohol intoxication due to binge drinking at the Republican Scientific Center for Emergency Medical Care and its Bukhara branch in 2019-2023. Of these, 238 were men - 85% and 42 women - 15%., average age 41.4±5.6 years. The study was divided into 2 stages: Stage 1 – study of the state of liver function, cognitive functions and the impact of their disorders on alcoholism in patients with alcohol intoxication during the post-intoxication period. At this stage, 150 patients were examined, admitted in 2022-2023, who received standard drug therapy, at the end of which all patients on the 5th day underwent a study of ammonia and lactate levels in the blood, a study of cognitive functions using the MMSE and the Reitan test, and an assessment of severity their violations using the scale we developed. Also on day 5, problematic alcohol consumption was assessed using the AUDIT test. Stage 2 to study the effectiveness of the developed measures of complex drug and psycho-social therapy for patients with alcohol intoxication in the post-intoxication period. At this stage, the data of 223 patients who received treatment in 2019-2023 were studied. The patients were divided into 3 groups: Group I 93 patients with mild and moderate cognitive-metabolic disorders who were treated in the toxicology department in 2022-2023 and who, after discharge from the toxicology department, received additional complex hepatoprotective therapy: the antihypoxant cytoflavin 1 tablet 2 times a day, ammonia-binding drug L-ornithine-L-aspartate 1 powder 3 times a day and ademetionine 750 mg 2 times a day for 7 days. After the end of treatment, standard FBI (Family Brief Intervention) interventions were carried out on the 7th, 30th day, after 6 and 12 months. Group II - 48 patients who were treated in the toxicology department in 2021, who also underwent standard FBI (Family Brief Intervention) interventions on the 7th day after discharge from the hospital, also on the 7th, 30th day, after 6 and 12 months without preliminary hepatoprotection. Group III (archival) - 82 patients who were treated in the toxicology department in 2019-2020 and did not receive any medication or psycho-social assistance after discharge from the hospital. Results: The development of a scoring system for cognitive-metabolic disorders in patients with alcohol intoxication in the post-intoxication period, based on laboratory and screening research methods, made it possible to determine in more detail the timing and strategy for drug and psychosocial correction of patients. Conclusion: The complex of drug hepatoprotective therapy and psychosocial correction we have developed for patients with alcoholism who have suffered alcohol intoxication significantly reduces the craving for repeated drinking of alcoholic beverages and improves the quality of life of this category of patients.
Keywords: Cognitive functions, Hepatic encephalopathy, AUDIT test, FBI (Family Brief Intervention)
Cite this paper: Khusenov O. N., Stopnitsky A. A., Issues of Diagnosis, Treatment and Rehabilitation of Patients with Alcohol Intoxication in the Post-Intoxication Period, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2663-2667. doi: 10.5923/j.ajmms.20241410.45.
Article Outline
1. Introduction
- The dynamics of disorders associated with the use of psychoactive substances in Uzbekistan is characterized by an increase in alcohol dependence with a constant decrease in drug abuse [1]. According to available data, more than 90% of all patients with alcohol intoxication are admitted to the toxicology departments of the RSCEMP and its branches as a result of a combination of acute and chronic alcohol intoxication, i.e. binge drinking [1,2]. alcohol intoxication against the background of previous alcoholism, we noticed that all patients had disorders of the liver function, primarily detoxification, which was manifested by an increase in the level of free ammonia in the blood [1,2,3,4]. There was also a significant clinical deterioration in the patient's condition with its increase and a significant positive effect from appropriate hepatoprotective, ammonia-binding therapy [1,4]. However, despite the change in the tactics of intensive care for this category of patients in the toxicology departments of our country, the very strategy of the emergency medical care system does not imply a complete cure of patients after binge drinking, but only withdrawal from a critical condition [1]. The average duration of hospitalization of patients admitted with alcohol intoxication is 5.2±1.2 days, which is absolutely insufficient for the complete recovery of the body of such patients, including liver functions [1,2,6]. Withdrawal is also partially preserved, which increases the risk of renewed alcohol abuse. At the same time, the overwhelming majority of patients, after being discharged from the toxicology department, for various reasons, refuse to continue treatment in narcological clinics, thereby the problem of alcoholism itself is not resolved. Therefore, there is an urgent need to create a set of treatment measures and improve the rehabilitation of people who abuse alcohol in the post-intoxication period [1,5,8]. Personality disorders caused by alcohol abuse do not develop in isolation. For many people suffering from chronic alcohol abuse disorders, interaction with relatives determines the patterns and dynamics of their alcohol problems [9,7,16]. Moreover, the interaction of family members with a person suffering from alcoholism can either consolidate and aggravate the problem, or significantly help in solving it. Family therapy is offered when the patient shows signs that substance abuse is strongly influenced by the behavior of family members or communication with them [9,10,12,13]. Thus, short-term interventions and total family intervention are effective mechanisms to reduce alcoholism of the population, because Uzbekistan is an Islamic state and the family is of great importance, the word of parents is often absolute and children respect their parents very much. However, these methods are effective only in patients without cognitive deficits [1,15,16]. At the same time, the works of domestic and foreign authors have proven that the majority of patients admitted to emergency hospitals with alcohol intoxication are discharged with persistent intellectual disorders of varying severity, due to metabolic disorders, hypoxia, and toxic liver damage [14,15,16]. As a result, there is an urgent need to identify latent cognitive disorders in patients at the time of discharge from toxicology departments, which will allow determining the timing of psychosocial interventions, as well as the need for additional medical support [4,7].The aim of the study was to study the effectiveness of the developed point system for early diagnosis of cognitive and metabolic disorders, as well as a complex of hepatoprotective drug therapy and psychosocial correction in patients with alcohol intoxication in the post-intoxication period.
2. Research Methods
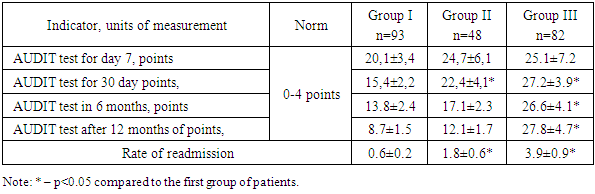
- 280 patients aged 18 to 60 years who were admitted with alcohol intoxication against the background of binge drinking to the Republican Scientific Center for Emergency Medical Care and its Bukhara branch in 2019-2023 were examined. Of these, 238 were men - 85% and 42 women - 15%, the average age was 41.4±5.6 years. The study was divided into 2 stages:Stage 1 – study of the state of liver function, cognitive functions and the impact of their disorders on alcoholization in patients with alcohol intoxication in the post-syntoxication period. At this stage, 150 patients admitted in 2022-2023 who received standard drug therapy, at the end of which all patients on the 5th day underwent a study of the level of ammonia and lactate in the blood, the study of cognitive functions using the MMSE and the Reitan test, and the assessment of the severity of their disorders using the scale developed by us. Also, on the 5th day, the problem alcohol consumption was assessed using the AUDIT test.Stage 2 to study the effectiveness of the developed measures of complex drug and psycho-social therapy of patients with alcohol intoxication in the post-intoxication period. At this stage, the data of 223 patients who received treatment in 2019-2023 were studied. The patients were divided into 3 groups: group I: 93 patients with mild and moderate cognitive and metabolic impairment who were treated in the toxicology department in 2022-2023 and who, after being discharged from the toxicology department, received additional complex hepatoprotective therapy: antihypoxant cytoflavin 1 tablet 2 times a day, ammonia-binding drug L-ornithine-L-aspartate 1 powder 3 times a day and ademetionine 750 mg 2 times a day for 7 days. After the end of treatment, standard FBI (Family Brief Intervention) interventions were performed on the 7th, 30th day, 6th and 12th months later.Group II – 48 patients treated in the toxicology department in 2021, who also underwent standard FBI (Family Brief Intervention) interventions on the 7th day after discharge from the hospital, as well as on the 7th, 30th day, after 6 and 12 months without prior hepatoprotection.Group III (archival) – 82 patients who were treated in the toxicology department in 2019-2020 and did not receive any medication and psycho-social assistance after discharge from the hospital. All patients on the 7th day, 30th day, 6 and 12 months after discharge from the hospital underwent an assessment of problematic alcohol consumption using the AUDIT test. The rate of readmissions within a year of hospital discharge was also examined. To conduct research at both stages, permission was obtained from the Ethics Committee of the Republic of Uzbekistan No9/4-1829. Patients suffering from significant concomitant chronic diseases (coronary artery disease, thyrotoxicosis, hypertension), with poisoning of other etiologies, under the age of 18 years, and pregnant women were excluded from the study.
3. Results of the Survey and Their Discussion
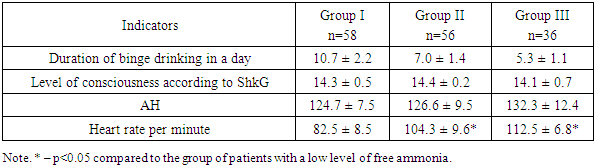
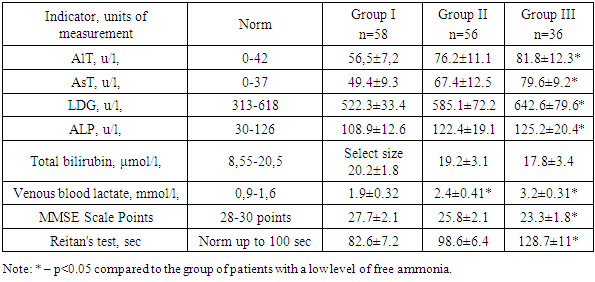
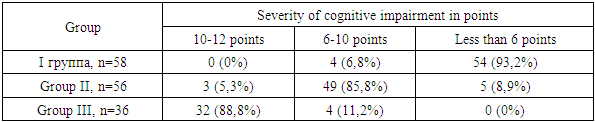
- In the course of stage I, all patients were divided into three groups depending on the level of free ammonia on day 5 according to the clinical guidelines "Russian consensus of hyperammonemia in adults from 2019":Group I, n=58 - with a relatively low level of free ammonia, mild hyperammonemia (< 100 μmol/l). Group II, n=56 - with an average level of free ammonia, hyperammonemia of moderate severity (100-200 μmol/l).Group III, n=36 – with a high level of free ammonia, severe hyperammonemia (over 200 μmol/l).After stratification of patients according to the level of free ammonia, we obtained the following results (Table 1).
|
|
|
|
|
4. Findings
- 1. The development of a point assessment system for cognitive-metabolic disorders in patients with alcohol intoxication in the post-intoxication period, based on laboratory and screening research methods, made it possible to determine in more detail the timing and strategy of drug and psychosocial correction of patients. 2. The complex of hepatoprotective drug therapy and psychosocial correction developed by us for patients with alcoholism who have suffered alcohol intoxication significantly reduces the craving for repeated use of alcoholic beverages and improves the quality of life of this category of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML