-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2655-2658
doi:10.5923/j.ajmms.20241410.43
Received: Oct. 2, 2024; Accepted: Oct. 22, 2024; Published: Oct. 25, 2024

Vaginal Vault Prolapse After Total Hysterectomy
Shomirov D. A., Nadkrkhanova N. S., Dauletova M. J.
Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Total hysterectomy is one of the most common surgical interventions in gynaecology, the frequency of which varies from 30% to 60%, according to various authors. Moreover, the number of performed extirpation of the uterus has been steadily growing every year. The most common indications for uterine extirpation are uterine fibroids, abnormal uterine bleeding that cannot be treated conservatively, as well as cervical and endometrial cancer.
Keywords: Total hysterectomy, Obesity, Uterine fibroids, Prolapse
Cite this paper: Shomirov D. A., Nadkrkhanova N. S., Dauletova M. J., Vaginal Vault Prolapse After Total Hysterectomy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2655-2658. doi: 10.5923/j.ajmms.20241410.43.
Article Outline
1. Introduction
- Genital prolapse is a multi-factorial disease, which necessitates the reasonable choice of a standardized treatment method, on the one hand, and an individual method of surgical correction, on the other hand, for each patient. Vaginal vault prolapse after total hysterectomy is a condition in which vaginal vault, the bladder, and the anterior wall of the rectum form hernial bulging into vaginal canal, extending beyond vaginal opening at the later stages of the postoperative period [1,7]. This condition is not only medical, but also a serious socio-economic and psychological problem that significantly reduces the quality of life of a woman. The significant proportion of vaginal vault prolapse among gynecological nosology in departments of operative gynecology, even in highly specialized hospitals, is 19.9-49.6% [2,7,9].Only a comprehensive approach will improve the results of surgical treatment of patients with genital prolapse, reduce the frequency of relapses of this disease and the risk of immediate and long-term adverse results of surgery [2,4,7].The problem is compounded by the fact that almost 2/3 of women with this complication are obese women, who have a number of technical difficulties during the total hysterectomy due to the pronounced fat layer [2]. However, the tendency towards obesity among women has been increasing recently.For example, in the United States, the frequency of hysterectomies among laparotomic (abdominal) gynecological operations is 36%, in Russia from 32.5% to 38.3%, in Sweden 38%, in the UK-25% [3,4].Vaginal vault prolapse, as a rule, is accompanied by various unpleasant symptoms that cause a woman to experience severe discomfort. Often this process is accompanied by severe pain, urine retention or, conversely, urinary incontinence, frequent urination, problems with defecation [3-10]. With complete vaginal prolapse after hysterectomy, the mucous membrane of its walls is subject to severe injuries, which leads to the development of infectious diseases, abscess, and even tissue death [5,9,12].Existing methods of surgery do not always radically eliminate the pathology, which makes it necessary to develop new methods of surgery.Purpose of the study: to develop effective methods of surgical prevention and correction of vaginal vault prolapse in obese women who have undergone total hysterectomy.
2. Materials and Methods
- The study group consisted of 141 women with uterine fibroids more than 12 weeks and obesity that underwent total hysterectomy with abdominal access.At the first stage, there was a comprehensive clinical and laboratory examination of all patients who were admitted for planned surgical treatment for uterine fibroids and with obesity in the Republican specialized scientific practical medical center of obstetrics and gynecology.Indications for the operation were determined by a diagnosis made on the basis of a comprehensive clinical laboratory examination. In this study the following research methods were used: clinical (interview, examination, gynecological status), laboratory (examination of general blood and hematocrit before surgery and during the second day after the surgery) and special (examination of the blood clotting sequence). The cultures of the cervical canal, vagina, and urethra were examined.Patients in the hospital underwent additional examinations, which included ultrasound (trans-vaginal and abdominal access), Doppler study, computed tomography (CT scan), magnetic resonance imaging (MRI), etc.
3. Research Results
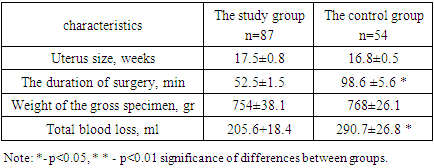
- Taking into account the method of surgical intervention, all the patients were divided into 2 groups. The main group of 87 women who underwent total hysterectomy operations with laparotomic access using advanced technology attaching the ligamentous apparatus to the vaginal vault, in which the top of the vagina was left open during the operation. The control group consisted of 54 patients who underwent total hysterectomies with laparotomic access using the traditional method. All operations were performed for the purpose of surgical treatment of uterine fibroids more than 12 weeks.The subjects of both groups were comparable in terms of socio-biological characteristics and severity of the disease. The study groups included patients with obesity and uterine fibroids more than 12 weeks requiring surgical treatment, aged 45 to 52 years, with an average age of 49.4±1.78 years. The decision on the scope of surgical treatment was made individually in each case.87 operations were performed (the main group) - total hysterectomy with laparotomic access using advanced technology. The essence of the method is to apply a direct clamp simultaneously with the capture of the sacro-uterine ligaments, cardinal ligaments and vascular bundle at an angle of 45 degrees with respect to the conductive axis of the uterus body, which makes it possible to combine the stages of surgery, thereby shortening its duration, reducing the volume of blood loss. Subsequent fixation of sacro-uterine, cardinal, circular ligaments with the side walls of the vagina on each side and simultaneous application of a twisted suture on the front and back walls of vaginal vault is performed with a single thread. Moreover, the beginning of the suture begins with ligation of the vascular bundle on one side, followed by the capture of the cardinal, Sacro-uterine ligaments and the transition to the back wall of vaginal vault (the beginning of the needle injection into vaginal vault begins from inside to outside, i.e. from the vaginal mucosa). The opposite side is sewn in reverse order. After ligation of the vascular bundle, it is necessary to fix circular ligament with the transition to the anterior wall of vaginal vault (performed by a similar technique). It is necessary to finish suture by fixing circular ligament on the opposite side.Thus, the proposed improved technique of total hysterectomy operation with abdominal access prevents vaginal vault prolapse in obese women. Because when suture is fixed, the size of the Douglass space decreases due to its stretching and lifting, which prevents the further formation of enterocele in obese women. This method preserves the physiological horizontal axis of the vagina in relation to the levators (levatoris ani externa), due to this, sexual function is not disturbed.The duration of total hysterectomy surgery using advanced technology varied from 45 to 75 minutes, with an average of 52.5+1.5 minutes.With the traditional method of abdominal total hysterectomy, the duration of the operation varied from 90 to 110 minutes, 98.6 ±5.6 minutes, (p<0.05). Thus, in the study group, it averaged 52.5+1.5 minutes, which was significantly shorter than in the control group - 98.6 ±5.6 minutes, (p<0.05).As can be seen from table 1, the size of the uterus according to ultrasound data and the weight of gross specimen in the compared groups were identical.
|
|
4. Discussion
- As with any surgical intervention, after extirpation of the uterus, early and late postoperative complications are possible. The most common early complication after extirpation of the uterus is a temperature reaction and suppuration. This type of complication is caused by the frequent accumulation of a small amount of exudate in the Douglas space. In the proposed method of forming vaginal vault, the possibility of accumulation of exudate in the postoperative period is excluded, due to the creation of a natural "drainage" of the paravesical and parametral spaces. Leaving the top of the vaginal open, we did not observe such complications, which contributed to the earliest possible discharge from the hospital. The improved technique of suturing the anterior and posterior walls of the vagina, vault of Sacro-uterine, round and cardinal ligaments, allows minimizing the number of postoperative complications.To confirm the effectiveness of the improved method of suturing vaginal vault we have analyzed the various characteristic features of early postoperative period in patients who underwent surgery of total hysterectomy using improved methods and traditional methods such as: number of bed-days after surgery, the number of days with increased body temperature, the figures of maximum rise of a body temperature and the number of women with culcit and granuloma.The vast majority of patients who underwent surgery using the improved method 92.1% - were in the hospital after the operation for up to 5 days, while women operated using the traditional method-66.3%.Also, in patients who underwent surgery using an improved technique, granulomas were not observed, which occurred in every third operated by the traditional method.Thus, the obtained results show the advantage of using the improved method of creating artificial drainage of the postoperative wound: reducing complications in the form of culcit, the formation of granulomas, reducing the number of days with fever, reducing drug use, reducing patients ' stay in hospital and increasing the turnover of beds.Restrictions in the process of sexual life are absent in the group of women operated on by improved technology due to the fact that during the operation, the ligaments were attached to vagina vault, which formed the top of the vagina, the physiological horizontal axis of the vagina in relation to the levators (levatoris ani externa) is preserved, which creates the possibility of normal sexual life. In the course of a traditional total hysterectomy, the vagina is shortened, which makes it difficult to have sex.When observed for 2 years after the operation using an improved technique, during which vaginal vault was fixed with Sacro-uterine, cardiac, and circular ligaments, there was no vaginal vault prolapse. Whereas, in women who underwent surgery using the traditional method, vaginal vault prolapse was observed in 17 patients, including cystocele in 9 cases, rectocele in 3 cases, and enterocele in 5 cases.Long-term results were studied from 2 months to 2 years; the majority of women operated on the improved technology were satisfied with the results of operations. Everyone noted an improvement in the quality of life related to health.The proposed parameters of the method allow achieving the set technical result: reducing the risk of early and late postoperative development in hospitals of any level.
5. Conclusions
- Thus, our proposed improved technique of total hysterectomy operation prevents vagina vault prolapse in obese women. Because when the seam is fixed, the size of the Douglass space decreases due to its stretching and lifting, which prevents the further formation of enterocele in obese women. This method preserves the physiological horizontal axis of the vagina in relation to the levators (levatoris ani externa), due to this, sexual function is not disturbed.In the proposed method of forming the vagina vault, the possibility of accumulation of exudate in the postoperative period is excluded, due to the creation of a natural "drainage" of the paravesical and parametral spaces.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML