Gafur-Akhunova Kamola Mirzalievna1, Polatova Jamila Shagairatovna2, Tukhtabayeva Mukaddas Tukhtabaevna3, Egamberdiev Gayrat Makhkamovich4, Tolipov Ramiziddin Nazhmiddinovich5
1Oncomammologist, Independent Researcher, Tashkent Regional Branch of the Republican Specialized Scientific-Practical Medical Center (RSSPMC) of Oncology and Radiology
2Head of the Department of Oncology and Medical Radiology of the Tashkent State Dental Institute
3Head of the Department of Oncomammology of the Tashkent Regional Branch of the RSSPMC of Oncology and Radiology
4Head of the Department of Chemotherapy of the Tashkent Regional Branch of the RSSPMC of Oncology and Radiology
5Head of the Radiology Department of the Tashkent Regional Branch of the RSSPMC of Oncology and Radiology
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article presents data on 128 patients with primary disseminated breast cancer (PDBC) with skeletal bone damage. The clinical course and forms, histological variants, and treatment methods are presented. Special attention is paid to the clinical forms, the degree of malignancy and the immunohistochemical profile of the tumor. Based on these indicators, an individual approach has been developed in the treatment of primary disseminated breast cancer with damage to the bones of the skeleton.The work proved an improvement in survival rates in the group of patients operated on the primary lesion compared to without surgery. The treatment approach largely depended on the effectiveness of neoadjuvant chemotherapy, hormone therapy, bisphosphonate therapy and radiation therapy. The results showed that the above treatment methods should be carried out within 12 months and after receiving positive results, surgery can be performed on the primary lesion.
Keywords:
Primary disseminated breast cancer, Chemotherapy, Hormone therapy, Bisphosphonate therapy, Radiation therapy, Treatment effectiveness, Bone metastases, Radioisotope bone examination, Survival
Cite this paper: Gafur-Akhunova Kamola Mirzalievna, Polatova Jamila Shagairatovna, Tukhtabayeva Mukaddas Tukhtabaevna, Egamberdiev Gayrat Makhkamovich, Tolipov Ramiziddin Nazhmiddinovich, Improvement of Treatment Methods for Primary Disseminated Breast Cancer, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2626-2631. doi: 10.5923/j.ajmms.20241410.38.
1. Introduction
Breast cancer (BC) is one of the most common forms of malignant neoplasms in the world. If in the world (according to WHO, 2022) about 20 million new cases of various forms of malignant neoplasms are registered annually, and 2.4 million (11.3%) are cases of breast cancer. Unfortunately, the number of patients with this disease is increasing every year, and according to WHO forecasts, the number of patients registered annually may increase to 2.5 million by 2030. This is despite the fact that screening studies are widely conducted in many countries of the world (GLOBOCAN, 2023). In the Republic of Uzbekistan, as of 2022, 4,415 breast cancer patients were registered (12.8 per 100 thousand population), of which 518 (11.8%), stage II 2,472 (56%), stage III 990 (22.4%) and stage IV 410 (9.3%) (Tilashaykhov M.N. and co., 2023). According to various sources, about 11% of patients have metastatic disease at the time of diagnosis. The median survival rate of patients with metastatic process is about 20 months (from 18 to 24 months) [11]. According to many authors, locally advanced cancer is the main cause of early dissemination of the tumor process. The progression of the tumor process is observed in 30% of cases with the N0 process, and in the presence of N1 – in 70% of cases. In the presence of micrometastases, they are realized on average 19-21 months earlier than in early breast cancer - on average after 37-42 months. In contrast to the nodular form, in the edematous-infiltrative form, early dissemination of the tumor is observed. At the same time, there is a diffuse spread of the tumor through the breast tissues and early metastasis, an unfavorable outcome of the disease [16].A few decades ago, the diagnosis of disseminated breast cancer was practically a verdict, the average life expectancy did not exceed 15 months, 15% of patients managed to live for more than 3 years, and only 10% managed to live for more than 5 years. Now the average life expectancy of patients with PDBC is 51 months, and the 3- and 5-year overall survival in some forms (metastasis to bones, soft tissues) reaches 61% and 40%, respectively [14,15]. The study of the effect of operations on the primary focus on survival in patients with PDBC showed that the median overall survival of patients with breast resection and lymphodissection (n=29) is 76 months, with mastectomy and lymphodissection (n=62) is 42 months. The median IBD was 43 and 26 months, respectively (p=0.353). According to some data, the volume of surgery on the primary focus does not affect survival rates [12,13]. According to E.V. Chernova [9], based on the results of multivariate analysis, the most significant criteria affecting the prognosis and life expectancy were determined. According to the author, the removal of the primary tumor in breast cancer with an initial ECOG status of 0-1 can be considered optimal: According to some data [2,5,7,9], in advanced breast cancer, chemotherapy and hormone therapy are the main methods of treatment that significantly prolong the patient's life and improve its quality. In 10-25% of women with disseminated breast cancer, it is possible to achieve complete tumor regression with a long, relapse-free period. The most effective first-line treatment regimen is anthracyclines or taxanes. In case of overexpression of HER2/ neu, the administration of herceptin increases the effectiveness of treatment by 42-60%. According to R.V. Orlova [6], the treatment of patients with primary disseminated breast cancer (breast cancer) is one of the most difficult problems of clinical oncology.The concept of incurable disseminated breast cancer is determined by the choice of treatment methods, the main purpose of which is to maximize the prolongation of life and alleviate the symptoms of the disease. In this regard, treatment should be phased, rational, consistent, adequate, promising, timely and comprehensive. The main principle of treatment of breast cancer is a systematic approach, that is, initially chemotherapy, but we must not forget about the local approach to treatment (radiation therapy, cytoreductive surgical treatment), which will improve the quality of life of the patient and increase its duration [2,4,5].In the initial diagnosis of breast cancer, dissemination is found in 6% of patients, and among those operated on for early stages of breast cancer – in 30-50%. The effectiveness of drug treatment is 15%. According to A.M. Garin (2000), to date there are no generally accepted standards for the treatment of this pathology [1].
2. Materials and Methods of Research
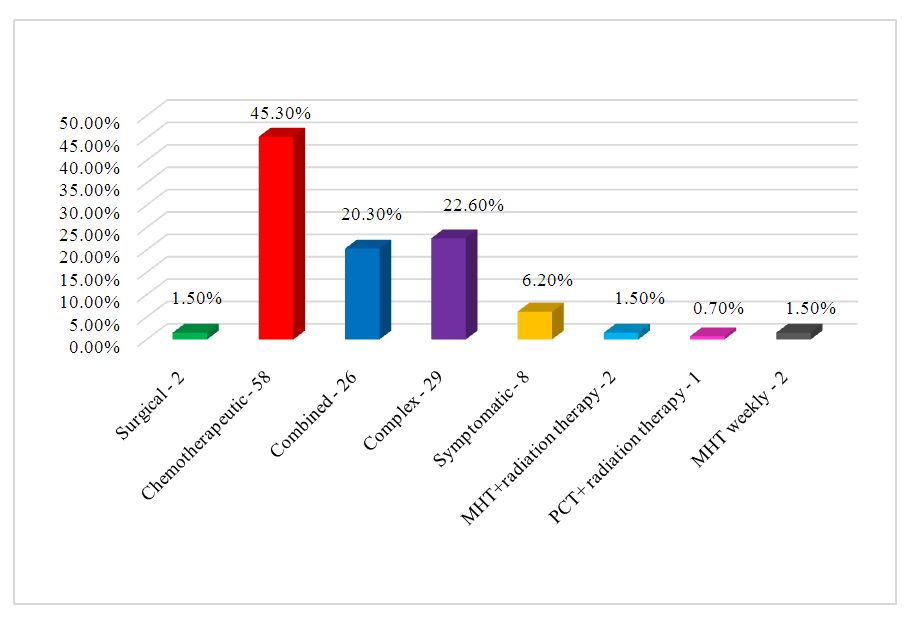
We observed 128 patients with primary disseminated breast cancer with skeletal bone damage who received treatment at the Tashkent city and regional branches of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology of the Ministry of Health of the Republic of Uzbekistan in the period from 2010 to 2023. The age of patients ranged from 23 years to 76 years, averaged 49.4 years, patients under 30 years were 3 patients (2.3%), 30-40 years – 13 (+ 0.1%), 41-50 years – 37 (29.9%), 51-60 years – 41 (32%), 61-70 years – 25 (19.5%), over 70 years of age – 9 (7%). (Fig. 1). 60.9% of the patients were aged 40-60 years. | Figure 1. Distribution of patients depending on age |
The duration of the anamnesis ranged from 1 month to 5 years. Of the 128 patients, 37 (28.9%) went to the doctors within 6 months of the onset of the first symptoms of the disease, 41 (32%) from 6 months to 12 months and 50 (39.1%) for more than 12 months. Of the 128 patients, 69 (53.9%) had the disease started with symptoms of the primary lesion - the appearance of pain in the mammary gland – 4 (3.1%), pain and the presence of a tumor – 44 (34.4%) and the presence of a tumor – 21 (16.4%). When studying the anamnesis of 128 patients, 24 (18.7%) had a complicated heredity (various oncological diseases were detected in parents and relatives of the first line). In the remaining patients, the first manifestation of the disease was pain in the bones of the skeleton – 27 (21.1%), chest pain – 8 (6.2%), frequent headaches, visual impairment – 1 (0.8%) and back pain – 6 (4.7%).During a clinical examination of 128 patients, 59 (46.1%) had lesions of the right, 63 (49.2%) of the left and 6 (4.7%) of both mammary glands.During clinical examination, in 67 (52.3%) cases, the tumor in the mammary gland was mobile, in 15 (11.7%) – not mobile, in 3 (2.3%) – embedded, in 42 (32.8%) - sedentary and in 1 (0.7%) – in the form of a single conglomerate. The consistency of the tumor on palpation was dense in 108 (84.4%) patients, in 6 (4.7%) – rocky density, in 5 (3.9%) – calcified and in 9 (7%) – soft consistency.Of the 128 patients, 56 (43.7%) had a tumor localized in the upper-outer quadrant, 29 (22.6%) – in the upper-inner quadrant, 12 (9.3%) – in the lower-outer quadrant, 4 (3.1%) – in the lower-inner quadrant, 22 (17.1%) - in the center and in 5 (3.9%) - a total lesion was noted.Clinically, 16 (12.5%) had skin changes. On visual examination, 14 (10.9%) patients had hyperemia of the skin of the breast, 25 (19.5%) had infiltration, 3 (2.3%) had swelling, 5 (3.9%) had ulceration of the skin, 15 (11.7%) had a lemon peel symptom, 1 (0.7%) – a symptom of the area, in 18 (14%) – nipple retraction, in 11 (8.5%) – tumor disintegration, in 2 (1.5%) – skin disintegration and ulceration, in 19 (14.8%) – infiltration and swelling of the breast and only in 15 (11.6%) patients in the breast there were no changes in the gland.In addition to the above symptoms of the primary lesion, out of 128 patients, 11 (8.4%) patients had an increase in body temperature above 37.50 C. 116 patients (90.6%) had general weakness, 110 (85.8%) had decreased appetite, 27 (21.0%) had weight loss of the first degree, 8 (6.2%) – weight loss of the II degree and in 3 (2.3%) – cachexia. Of the 128 patients, only 17 (13.2%) showed no signs of pain syndrome. The severity of the pain syndrome was of a different nature, but 47 (36.7%) had pain in the bones of the whole body of an indeterminate nature. In other cases, in 6 (4.6%) patients, the pain syndrome was local in the form of headaches, in 15 (11.7%) - chest pain, in 2 (1.5%) - joint pain, in 11 (8.5%) - limb pain, in 1 (0.7%) - chest pain, in 1 (0.7%) - pain in the right hypochondrium, in 7 (5.4%) - abdominal pain and in 21 (16.3%) - back pain. All patients were examined and conducted clinical, laboratory and instrumental (X-ray, ultrasound, CT/MSCT, MRI, PET/CT), morphological (cytological, histological, immunohistochemical studies) studies and statistical processing of clinical material. In addition, we have studied survival rates and factors affecting the prognosis of the disease.To verify the diagnosis at the level of the primary lesion and metastatic foci, a comprehensive examination was performed using the above methods. Metastatic bone damage in all patients was confirmed using a radioisotope study with the Te99m radioisotope and X-ray examination of skeletal bones. In addition, other methods (MSCT, MRI) were used, taking into account the localization of metastases in the bones of the skeleton. PET/CT examination was performed in 12 (9.3%) patients. At the same time, in 3 (2.1%) patients, the primary focus was detected in the mammary gland using PET/CT.For histological verification of the diagnosis at the level of the primary focus and metastases in the bones of the skeleton, 43 (33.5%) of 128 patients underwent puncture biopsy, 64 (50%) had trepan biopsy, 2 (1.5%) had open biopsy, 11 (8.5%) had puncture biopsy +open biopsy, In 4 (3.1%), a cor biopsy was performed and in 4 (3.1%), the diagnosis was verified by examining fingerprint smears.In all 128 patients, the diagnosis was verified histologically and 16 (12.5%) had in situ cancer in the primary focus, 89 (69.5%) had infiltrative ductal cancer, 13 (10.1%) had infiltrative lobular cancer, 4 (3.1%) had tubular cancer, 4 (3.1%) – papillary cancer, 1 (0.7%) – adenocystic cancer and 1 (0.7%) Paget's cancer.The degree of prevalence of the tumor process is determined by stages and the TNM system (2018, VI edition).In all patients, the degree of tumor spread was assessed as stage IV with the detection of metastases in the bones of the skeleton.The degree of tumor spread by the TNM system is presented as follows: T1 N1 M1 – 12 (9.3%), T2 N0 M1 – 2 (1.5%), T2 N1 M1 – 30 (23.4%), T2 N2 M1 – 6 (4.6%), T3 N2 M1 – 2 (1.5%), T3 N3 M1 – 3 (2.3%), T4 N1 M1 – 50 (39%), T4 N2 M1 – 10 (7.8%) and T4 N2 M1 – 10 (7.8%) and T4 N3 M1 – 12 (9.3%). As can be seen from the presented data, out of 128 patients in 45 (35.1%), the tumor in the primary focus corresponded to T1 – T2 indicators, and the lesion of regional lymph nodes was N0 – N2 levels, and in 83 (64.8%) patients, the tumor prevalence in the primary focus corresponded to T3 – T4, and the lesion of lymph nodes was N1 – N3. In this group of patients, lesion of regional lymph nodes was found in 100% of cases. It should be emphasized that in primary disseminated breast cancer, out of 128 patients, only 2 (1.5%) had no lesion of regional lymph nodes. This is important for determining treatment tactics and in conducting palliative surgical interventions at the primary focus in the form of palliative radical mastectomy.In breast cancer, especially in the primary disseminated form, immunohistochemical examination with the determination of the luminal type of tumor is important. Immunohistochemical examination was performed in 75 (58.6%) patients. At the same time, luminal type A was detected in 25 (33.3%), luminal type B in 43 (57.3%) and triple negative type in 7 (9.4%). As can be seen from the presented data, 66.7% of patients had an immunohistochemically unfavorable luminal B type profile and a thrice negative tumor phenotype.When analyzing the expression of various receptors and markers of immunohistochemical examination, it was found that 54 (72%) patients had a positive estrogen receptor and 44 (58.7%) progesterone. At the same time, out of 75 patients, 46 (61.3%) had HER-2/neu negative and 29 (38.7%) positive. The Ki-67 index has a prognostic value in determining treatment tactics. In our observations, out of 75 patients, 22 (29.3%) had a Ki-67 index of up to 20% and 53 (70.7%) from 20% to 60%. The Ki-67 index above 20% indicates the aggressiveness of the tumor and, accordingly, the early dissemination of breast cancer.In our observations, out of 128 patients, 81 (63.2%) had several bone lesions and in other cases isolated, solitary skeletal bone lesions. At the same time, 31 (34.2%) patients had lesions of various parts of the spine, 3 (2.3%) – skull bones, 1 (0.7%) – humerus, 4 (3.1%) – tibia, 1 (0.7%) – fibula, 1 (0.7%) – the sternum and in 6 (2.2%) - the pelvic bones.Further dissemination of the tumor process after the appearance of metastases in the bones, metastases appeared in the lungs and other organs. At the same time, 8 (6.2%) had isolated, 5 (1.5%) had solitary, and 37 (28.9%) had multiple metastases. 7 patients subsequently developed brain metastases. At the same time, 3 (2.3%) in the cerebral hemisphere and 4 (3.1%) in the brainstem.After a comprehensive examination and diagnosis of primary disseminated breast cancer, 58 (45.3%) patients underwent chemotherapy, 28 (21.8%) - combined treatment, 29 (22.6%) – complex treatment, 3 (2.2%) – chemo-radiation therapy (2 – monochymotherapy, 1 – polychemotearpy), in 2 (1.5%) – monochemotherapy and in 8 (6.2%) – symptomatic treatment. Palliative radiation therapy was performed in 34 patients.Chemotherapy as the main type of treatment was carried out according to the standard of treatment for breast cancer. At the same time, the main chemotherapy regimens were CAF, FAC, AC, DA, CAP, PA. Chemotherapy was performed first according to the CAF, FAC, AC scheme up to 6-8 courses, at the second stage, the drugs paclitaxel, carboplatin, docetaxel, doxorubicin, cisplatin, cyclophosphane were included in the treatment regimen. If HER-2/neu is positive, trastuzumab (herceptin) is recommended for patients.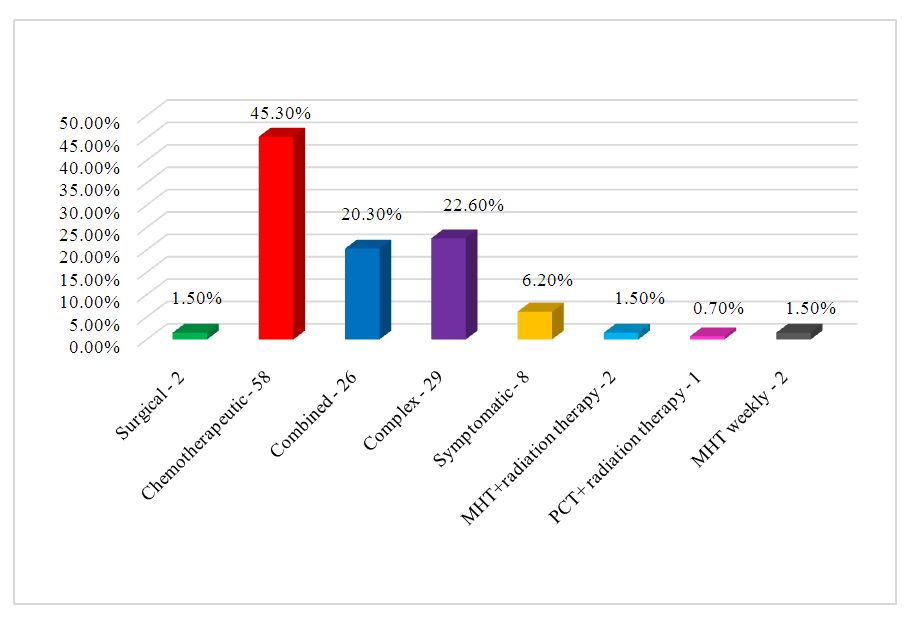 | Figure 2. Types of treatment for primary disseminated breast cancer |
Of the 128 patients, 64 (50%) underwent surgery at the primary focus level. At the same time, 47 (73%) patients with primary disseminated breast cancer underwent radical Madden mastectomy after neoadjuvant chemotherapy and high treatment effect. In addition, 9 (14.1%) underwent palliative simple mastectomy and 3 (4.7%) underwent radical mastectomy according to Paiti. For diagnostic and therapeutic purposes, radical resection according to Blokhin was performed in 1 patient, radical resection according to Veronesi in 2 patients and sectoral resection in 2 patients. | Figure 3. Types of surgical interventions on the primary lesion |
When analyzing the degree of tumor differentiation, it was found that out of 128 patients, 56 (43.7%) had highly differentiated, 40 (31.2%) had moderate differentiation, 18 (14.2%) had low differentiation and 14 (10.9%) had undifferentiated.After detection of metastases in the bones of the skeleton, all 128 patients underwent harmony therapy (Tamoxifen femara, letrazole, anastrazole) and bisphosphonate therapy with zometa (zolendronic acid), 4 mg drip 1 time every 28 days for a period of 6 to 2 years, together with chemotherapy with a positive estrogen receptor. With the progression of the tumor process in the bones, the drug was replaced with denosumab 120 mg once a month subcutaneously.
3. Results and Discussions
Unlike the standards of treatment methods adopted in the Republic of Uzbekistan by the Ministry of Health No. 351 and No. 273, treatment for primary disseminated breast cancer was carried out individually, taking into account the evaluation of the effectiveness of neoadjuvant chemotherapy, hormone therapy (tamoxifen, femara, letrazole, anastrazole), radiation and bisphosphonate therapy and surgery. In most cases, second-line drugs were used during chemotherapy, combined and complex treatment.According to the international classification according to the RECIST and ECOG criteria, the effectiveness of treatment was evaluated using clinical examination, X-ray, ultrasound, radioisotope, MSCT, MRI and PET/CT studies. Radioisotope examination of skeletal bones and, if necessary, MSCT, MRI examinations were performed 6 months after the start of treatment to assess the effectiveness of treatment.After a comprehensive approach to treatment, out of 120 patients (8 patients received symptomatic treatment due to the prevalence of the tumor process or there was a contraindication to treatment), 5 (3.9%) had a full effect, 21 (16.4%) had a private effect, 89 (69.5%) had stabilization of the tumor process and 5 (3.9%) - tumor progression during treatment.When evaluating the effectiveness of treatment, we paid attention not only to the condition of the primary focus, but also to metastatic foci.The implementation of surgical intervention on the primary lesion (in the mammary gland) was discussed in consultation with the participation of specialists from mammologists, chemotherapists and radiologists.On average, operations on the primary lesion were performed 12 months after combined and complex treatment in the absence of progression of the tumor process and the appearance of new lesions against the background of specialized treatment.After neoadjuvant chemohormonotherapy and chemotherapy as a specialized treatment, improvement in the general condition was noted in 108 (84.3%) without changes - in 9 (7.0%) and in 6 (4.6%), deterioration was noted. After the treatment, 114 (98.0%) showed a decrease in pain syndrome.Toxic manifestations or adverse events after chemotherapy were gastrointestinal in 94 (73.4%), hematological in 9 (7.0%), hepatotoxic and nephrotoxic in 6 (4.6%), skin lesions in 4 (3.1%) and allergic in 1 (0.7%). After performing surgical interventions on the primary lesion, 24 out of 64 patients (37.5%) had a tumor recurrence. At the same time, during 1 year of follow–up in 16 (25%), up to 24 months - in 5 (7.8%) and up to 3 years in 6 (9.3%) and up to 5 years in 1 (1.5%) patient. All patients were followed up during the follow-up period from 12 months to 72 months. At the same time, despite chemotherapy, radiation, hormone therapy, combined and complex treatment in 52 patients, further progression of the tumor process was noted with the appearance of new lesions in the liver in 15 patients (11.7%), in the lungs - in 35 (27.3%) and in 2 (1.5%) - in the brain.By the end of this study, out of 128 patients, 57 (44.5%) patients and 71 (55.5%) with tumor progression were under medical supervision. Thus, in primary disseminated breast cancer, the complex method is the method of choice. The use of surgical treatment at the primary focus improves the results, increases the survival rate of patients and reduces the frequency of further generalization of the tumor process. In the group of patients with breast cancer after surgical intervention at the primary focus, the 3 and 5–year survival rates were higher than 75.4% and 62.2%, compared with patients without surgery - 64% and 44%, respectively.
References
| [1] | Sundquist, M., Brudin, L., & Tejler, G. (2017). Improved survival in metastatic breast cancer 1985–2016. The Breast, 31, 46-50. |
| [2] | Henderson, I. C., Garber, J. E., Breitmeyer, J. B., Hayes, D. F., & Harris, J. R. (1990). Comprehensive management of disseminated breast cancer. Cancer, 66(S14), 1439-1448. |
| [3] | Garrin A.M. Chemotherapy of disseminated breast cancer, just the value of cytostatics. // Practical medicine. - 2000. - No. 1. - pp. 27-30. |
| [4] | Davidenko I.S. Treatment of early metastatic breast cancer: Abstract. ... Doctor of Medical Sciences. – Barnaul, 2010. – S. 84. |
| [5] | Dobrovolskaya N.Yu. Drug and radiation therapy in the treatment of locally advanced breast cancer: Abstract. ... Doctor of Medical Sciences. – M., 2017. – 45 p. |
| [6] | Zagrekova E.I., Meshcheryakov A.A. Medicinal treatment of breast cancer. Breast cancer // Med. review. - 2019. – No.2/1. – p. 51. |
| [7] | Orlova R.V. Principles of drug treatment of patients with disseminated breast cancer. – St. Petersburg, 2013. – pp. 23-24. |
| [8] | Perevodchikova N.I., Gorbunova V.A. Guidelines for chemotherapy of tumor diseases. – M.: Prakt. medicine, 2017. – pp. 241-257. |
| [9] | Fry I.V. Effectiveness of intensified chemotherapy regimens for locally advanced and disseminated breast cancer: Abstract. ... Candidate of Medical Sciences. – M., 2012. – 29 p. |
| [10] | Chernova E.V. Prognostic value of resection and mastectomy in the complex treatment of patients with primary disseminated breast cancer: Abstract. ... Candidate of Sciences. – M., 2014. – 24 p. |
| [11] | Blanchard D.K., Shetty P.B., Hilsenbeck S.G. et al. Association of surgery with improved survival in stage IV breast cancer patients // Ann. Surg. – 2008. – Vol. 247, №5. – P. 732–738. |
| [12] | Coffey J.C., Wang J. H., Smith M.J. Excisional surgery for cancer cure. Therapy at a cost // Lancer Oncol. – 2003. – Vol. 4. – P. 760-768. |
| [13] | Fields R.C., Jeffe D.B., Trinkaus K. et al. Surgical resection of the primary tumor is associated with increased long-term survival in patients with stage IV breast cancer after controlling for site metastasis // Ann. Surg. Oncol. – 2007. – Vol. 14, №12. – P. 3345-3351 |
| [14] | Nguyen D.H., Truong P.T., Alexander C. et al. Can locoregion- ISSN 2181-7812 www.tma-journals.uz 29 Обзоры al treatment of the primary tumor improve outcomes for women with stage IV breast cancer at diagnosis? // Int. J. Radiat. Oncol. Biol. Phys. – 2012. – Vol. 84, №1. – Р. 39-45. |
| [15] | Ruiterkamp J., Ernst M.F., van de Poll-Franse L.V. et al. Surgical resection of the primary tumor is associated with improved survival in patients with distant metastatic breast cancer at diagnosis // Eurор. J. Surg. Oncol. – 2009. – Vol. 35, №11. – P. 1146-1151. |
| [16] | Shien T., Kinoshita T., Shimizu C. et al. Primary tumor resection improves the survival of younger patients with metastatic breast cancer // Oncol. Rep. – 2009. – Vol. 21, №3. – P. 827-832. |
| [17] | Gofur-Okhunov, M. A., A. B. Yigitaliyev, and O. M. Karimov. "Morphological Features and Methods of Treatment of the Diffuse Form of Breast Cancer." International Journal of Alternative and Contemporary Therapy 2.6 (2024): 20-29. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML