-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2611-2615
doi:10.5923/j.ajmms.20241410.35
Received: Sep. 25, 2024; Accepted: Oct. 16, 2024; Published: Oct. 23, 2024

Analysis of Angiographic Examination and Endovascular Intervention Methods in Patients with Varicose Veins of the Esophagus and Stomach
Umarov Zafarbek, Fuzail Ahmed, Pillappagari Hampi, Bhoomika Sarkar
Department of Surgical Diseases and Transplantology, Tashkent Medical Academy Urganch Branch, Urganch, Uzbekistan
Correspondence to: Umarov Zafarbek, Department of Surgical Diseases and Transplantology, Tashkent Medical Academy Urganch Branch, Urganch, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

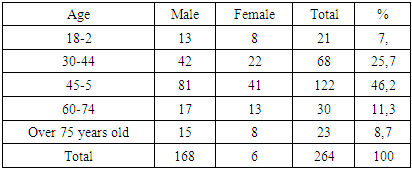
In 2017-2023, examination and treatment data of 264 patients with bleeding from varicose veins of the esophagus and stomach, who underwent endovascular and endoscopic interventions at the clinic of the Tashkent Medical Academy, were analyzed. All patients were divided into 2 groups according to treatment method: control group I (n=128) and main group II (n=136). Unlike the control group, the main group included 74 patients who underwent endovascular and endoscopic interventions after scheduled angiographic examination along with conservative treatment. Including 63.3% men, 36.3% women from 26 to 75 years old. For the objective distribution of patients by age groups, the classification of age groups adopted at the special symposium held in Kiev in 2002 and at the workshop of the Regional Bureau of the World Health Organization (163) was used, and is presented in Table 2.1. The purpose of the study: to improve results by angiographic examination and endovascular interventions in the complex treatment of patients with complications of portal hypertension and rebleeding from varicose veins of the esophagus and stomach.
Keywords: Esophageal and gastric varicose veins, Angiography, Minimally invasive, Staged, Liver cirrhosis, Portal hypertension and liver failure
Cite this paper: Umarov Zafarbek, Fuzail Ahmed, Pillappagari Hampi, Bhoomika Sarkar, Analysis of Angiographic Examination and Endovascular Intervention Methods in Patients with Varicose Veins of the Esophagus and Stomach, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2611-2615. doi: 10.5923/j.ajmms.20241410.35.
1. Introduction
- The most serious and often fatal complications of portal hypertension (PH) in the world are bleeding from varicose veins of the esophagus and stomach, "... it was determined that 60% of patients with varicose veins experience major bleeding..." [1,2,3]. Although modern methods of treatment of patients with portal hypertension have been discovered, the mortality rate after bleeding from varicose veins of the esophagus and stomach (VVES) is more than 25% in the first two months [4,5,6]. These indicators should encourage us to conduct new research and improve results.The purpose of the study: to improve results by angiographic examination and endovascular interventions in the complex treatment of patients with complications of PH and rebleeding from VVES.Tasks of the research:1. Retrospective analysis of PH patients with bleeding complications from VVES.2. To determine the causes of rebleeding in the near and long term.3. Study of liver-spleen angioarchitectonics with angiographic examination and endovascular interventions.
2. Material and Methods
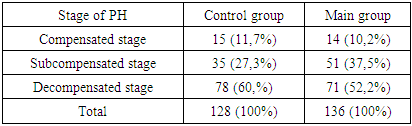
- In 2017-2023, examination and treatment data of 264 patients with bleeding from VVES, who underwent endovascular and endoscopic interventions at the clinic of the Tashkent Medical Academy, were analyzed.All patients were divided into 2 groups according to treatment method: control group I (n=128) and main group II (n=136). Unlike the control group, the main group included 74 patients who underwent endovascular and endoscopic interventions after scheduled angiographic examination along with conservative treatment. The total number of patients was 264, including 63.3% male and 36.3% female aged 26 to 75 years. For the objective distribution of patients by age groups, the classification of age groups adopted at the special symposium held in Kiev in 2002 and at the workshop of the Regional Bureau of the World Health Organization (163) was used, and is presented in Table 2.1.
|
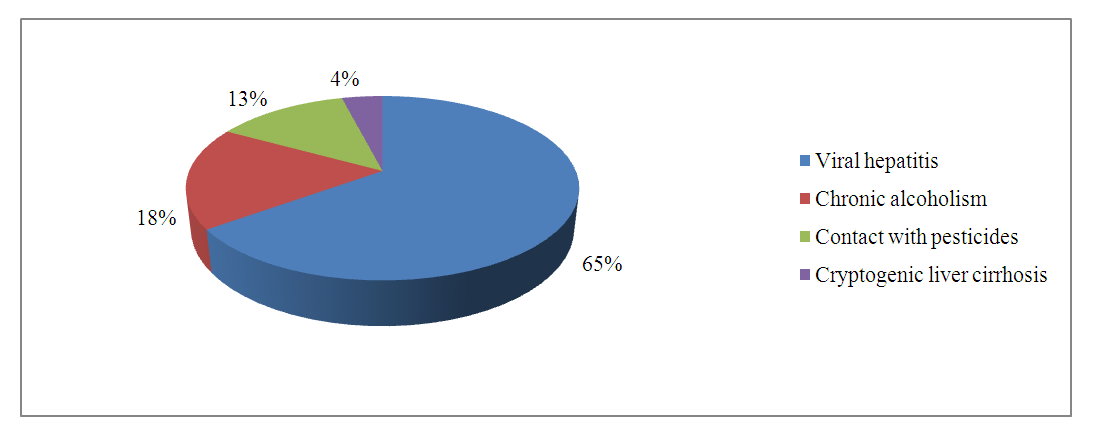 | Figure 2.1. Distribution of patients with the most common etiological factor of LC |
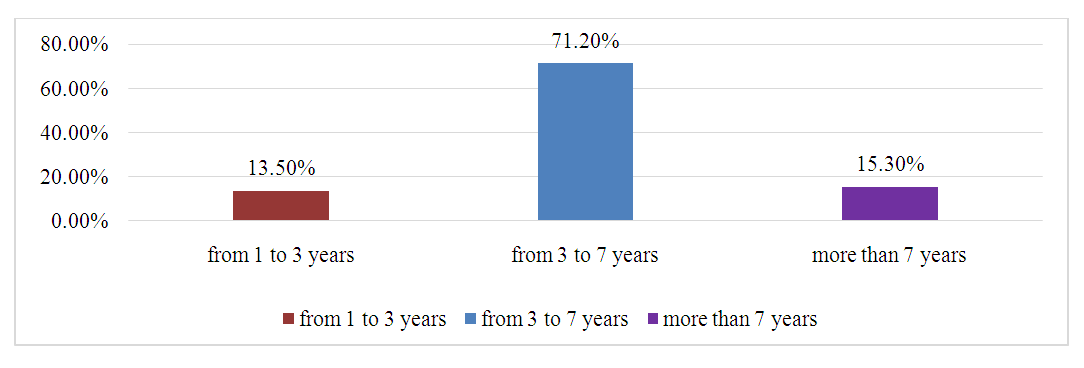 | Figure 2.2. Duration of LC |
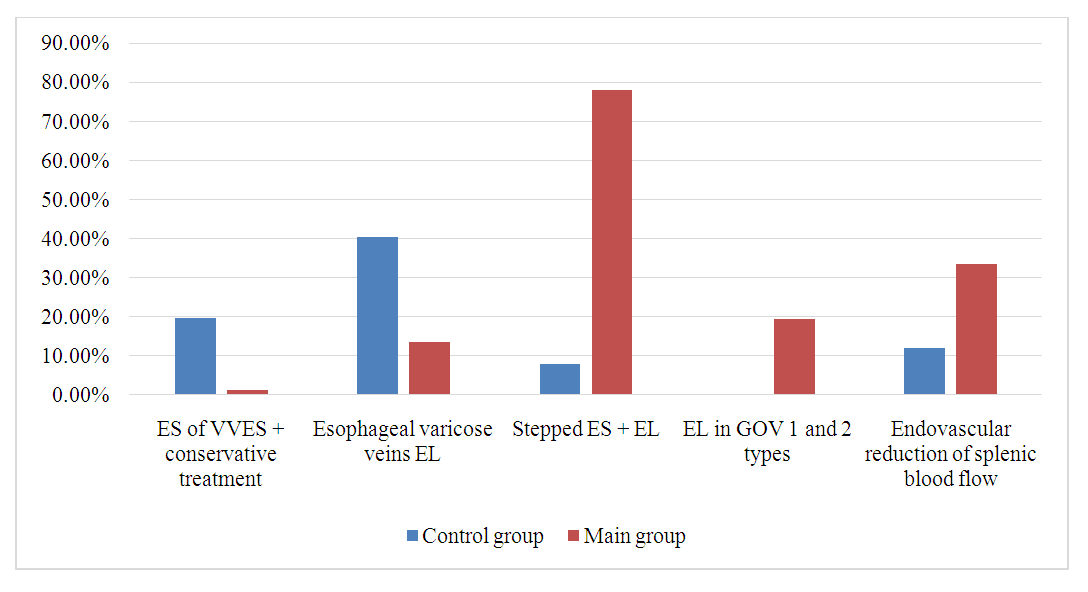 | Figure 2.3. Description of miniinvasive interventions in the control and main groups of patients |
|
 | Figure 2.4. Catheterization of the SA before ESA followed by arterio-graphy |
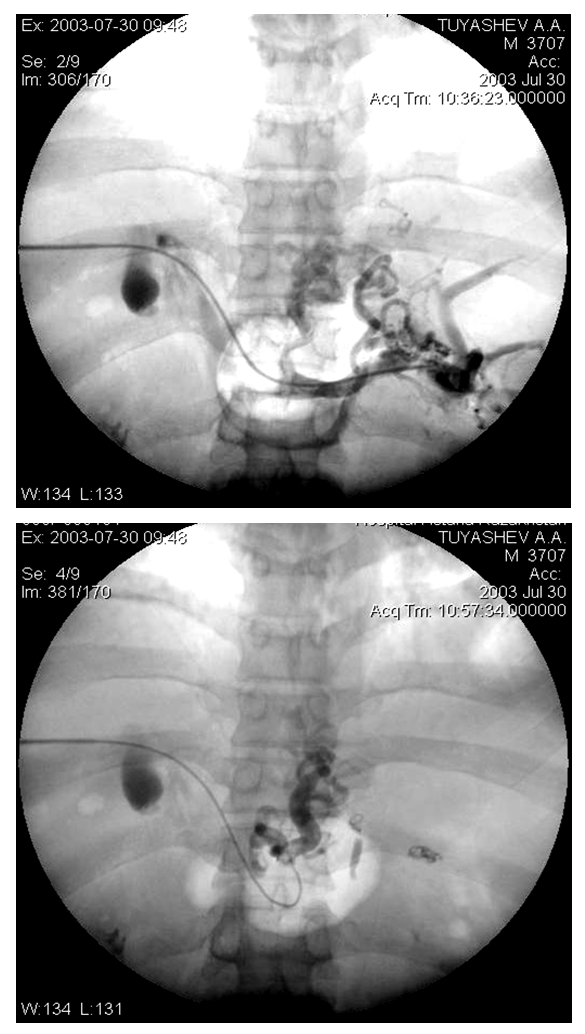 | Figure 2.5. Percutaneous transhepatic portography of esophageal and gastric varices with contrast conglomerate |
3. Results of Our Research
- The main reason for urgent surgical procedures in the control group patients of our study is the duration of bleeding. The use of staged endovascular and endoscopic treatment methods and CVP of 80 mm. A decrease from (53±7.7 mm Hg) helped stop bleeding in high-risk patients (7.3%), and conservative measures were effective only in 78.5% of patients in the control group (р<0.05). In the control group, 7.% of patients died of bleeding during the first days of admission, while in our main group of patients, the cause of death was progressive LF (2.4%, r<0.05).In the control group, long-term placement of the obturator-probe to stop bleeding caused supralaryngeal edema in .5% of patients, inflammation of the mucous membrane in 27 (47.4%), and the development of bedsores in the cardioesophageal zone in 5.2%. This not only complicated the performance of endoscopic hemostasis methods, but also caused excessive bleeding from the hemostasis areas in 16 (17.0%) patients of the control group. This condition required long-term pressure with the distal end of the device in the field of hemostasis and reinsertion of the obturator-probe in 8.8% of patients, as well as repeated endoscopic hemostasis methods in 7.0%, which also negatively affected the results of hemostasis. In the main group of patients, due to submucosal infiltration along the varicose veins of the cardiac department with a low CVP, it was possible to slightly reduce the expression of the tension of the esophageal varices, and it was easier to carry out sclerotherapy, which reduced the frequency of bleeding at the needle injection site by 6.7%.In the main group of patients, immediate hemostasis was achieved in 7.3% of cases; The main reason for the appearance of ulcers after ES is the presence of sclerosant outside the veins. This happens when there is active bleeding from the puncture site of the vessel and sclerosant is injected paravasally or additionally into the vascular bed. In the main group, the formation of ulcers was observed in 10.3% due to aseptic inflammation and tissue necrosis in the area of the gastric cardia, and in the control group, it was observed in 30.8%.In all cases, the use of endoscopy was accompanied by obvious inflammatory events in the cardioesophageal region and caused temporary dysphagia and pain during feeding. Dysphagia was observed in 64.2% of the control group and 55% of the main group.In the main group, a comprehensive approach to the use of endoscopy combined with additional endovascular intervention and selection of patients for conservative treatment reduced the incidence of LF from 18.5-22.3% to 13.6-17.2%. All patients with LF corresponded to Child-Pugh classes B and C, had ascites syndrome and high bilirubin levels.
4. Conclusions
- 1. Optimizing the selection of endovascular and endoscopic methods for the treatment and prevention of bleeding from VVES, combined with the developed step-by-step tactics of mini-invasive and traditional interventions, the percentage of long-term good and satisfactory results from 31.% to 54.% and reduction of bleeding allowed to reduce the frequency of total mortality from 56.0% to 28.5% (R<0.001).2. The hyperdynamic state of the SA and the increase in arterial perfusion of the spleen are directly related to the degree of PH and VVES. Thus, in patients with II-degree VVES, the diameter of the SA was 0.72±0.11 cm, the blood flow velocity was 127±14.1 cm/s, the VVES were In the III degree, it was 0.1±1.73 cm and 144±15.7 cm/s.3. Implementation of a tactical algorithm for the treatment and prevention of bleeding from VVES in patients with LC increased the two-year survival rate from 35.4±8.0% to 68.5±8.1% (median survival) improved from 13 months to 22 months (r<0.001).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML