-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2602-2607
doi:10.5923/j.ajmms.20241410.33
Received: Sep. 7, 2024; Accepted: Oct. 2, 2024; Published: Oct. 23, 2024

Reconstruction of Zygomatic Orbital Fractures with Titanium Micromesh: Literature Review
Boymurodov Shukhrat Abduzhalilovich1, Yusupov Shokhrukh Shukhratovich2, Iminov Komiljon Odiljonovich3
1Professor, Head of Department of Maxilla Facial Surgery and Dentistry, Tashkent Medical Academy, Tashkent, Uzbekistan
2Senior Lecturer, Department of Maxilla Facial Surgery and Dentistry, Tashkent Medical Academy, Tashkent, Uzbekistan
3Assistant, Department of Maxilla Facial Surgery and Dentistry, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Over the past few decades, the incidence of injuries in the world population, including in Central Asia countries, the number has increased quantitatively. Trauma to the zygomatic-orbital complex in facial fractures has one of the most common manifestations. At the crossroads of many clinical disciplines - mainly maxillofacial surgery, neurology, neurosurgery, ENT and ophthalmology - a complex problem of diagnosis and treatment of various traumatic complications of facial fractures, which requires a correct and minimally invasive solutions. The implementation of the main practical actions by specialists of different profiles of maxillafacial surgery is carried out only within the framework of a scheduled consultation (neurologist, ophthalmologist, ENT doctor) with a clearly expressed clinical picture. In this variant, the number of cases in the case where the severity of trauma orbital complex is not considered at all and the clinical symptoms of damage to the orbital complex more severe symptoms.
Keywords: Zygomatic orbital complex, Fractures, Titanium mesh, Reconstruction, Artificial intelligence, Diagnostics, Orbital trauma, Periorbital muscle and nerve, NVIDIA MONAI
Cite this paper: Boymurodov Shukhrat Abduzhalilovich, Yusupov Shokhrukh Shukhratovich, Iminov Komiljon Odiljonovich, Reconstruction of Zygomatic Orbital Fractures with Titanium Micromesh: Literature Review, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2602-2607. doi: 10.5923/j.ajmms.20241410.33.
1. Introduction
- Anatomical features of the zygomaticoorbital complex (ZOC) and severe injuries of the head and bones of the facial skeleton, representing a significant threat to human health and life, leading to many cases of severe disability of patients [1,4,6]. Whole cases, the patients with these types of injuries are classified as severe or heavy, because face skeletal bones are often injured the brain structures, damage to visual acuity organs and auricular disorders. The periorbital containing damage to the nerve and arterial supplying of eyeball, treatment and rehabilitation of patients with injuries of the zygomatic-orbital complex has some clinical and anatomical features [2,5,7]. In most cases, the diagnosis of pathological changes generated in the bonded orbital composite of the midface area. However, literary data and our own observation results indicate that past injuries can have a serious effect on serious long -term results. It leads to the early symptoms of ophthalmology disorders, including periorbital muscle and nerve systems, and the structure surrounding it [3,8,10]. Therefore, further research and studies are clearly needed on the diagnostic characteristics, course and clinical complications of traumatic injuries of the zygomatic-orbital complex, utilizing modern objective diagnostic tools in the research process, followed by an evaluation of post-traumatic complications [13,14,15]. According to several authors the proportion of (ZOC) fractures in the total number of bone lesions varies from 3,2-11%±1,4. However, in 88.2% of cases, only fractures of the facial skeleton were observed, soft tissue injuries in only 9.9% and after facial burns in 1.9%. on the other hand, other authors in the depressing majority of patients with ZOC fractures are observed from 88.3-93.6%±2,6 and lesions of isolated soft tissues 6.4-9.8%±1,7 all injuries. Computed tomography (CT) is commonly used for the diagnosis, treatment planning, and prognosis of pure orbital fractures of the orbital floor and medial wall [9,11,12]. The purpose of this study was to systematically review the current literature to establish an overview artificial intelligent facilities of computer tomography diagnosis and CT parameters associated with treatment choice and clinical (long-term) outcome in surgically and conservatively treated patients with zygomatic orbital fractures. PRISMA guidelines were followed. Databases were searched using the terms "orbital fracture", "computed tomography", “artificial intelligent facilities of computer tomography diagnosis”. Studies were included that evaluated the association between CT parameters and treatment decisions or clinical outcomes (ophthalmia, diplopia, and/or restriction of eye movements).
2. Material and Methods
- Reconstruction of Zygomatic Orbital Fractures with Titanium Micromesh: Literature Review was researched by us about 375 medical article materials and data in PubMed resources between 2010-2024. Moreover, the search returned 3,746 computer tomography results, which 45 were included (except three, all of which were retrospective. The routine use of CT imaging for orbital floor and medial wall fractures may be of great importance in therapeutic decision-making and prognosis (long-term) clinical outcomes for conservatively and surgically treated patients. The most significant parameters were found to be: fracture size, fracture site, orbital volume, soft tissue involvement, and craniocaudal size. Some patients has great potential for personal use, but perhaps the best results are obtained by integrating all parameters into an algorithm. It has great predictive power and is the most practically applicable tool. Systematic use of CT visualization in floor orbital fractures. The inner wall is very important in determining treatment and prediction (Long -term) clinical results of both conservative and surgical treatments patient. It turns out that the following parameters are most relevant. Fracture size, fracture position, orbital volume, soft tissue and skull ball measurement. Although some of them have great potential individually, including all parameters in the algorithm provides the best predictive power and is therefore likely to be the most practical tool. The most common locations are the floor of the orbit (FO) and the medial wall (MW), and isolated fractures IF. Furthermore, as the midface is a very complex anatomical region, unnecessary surgery may result in avoidable iatrogenic damage, such as infraorbital nerve injury, postoperative diplopia, optic nerve injury, hemorrhage, and infection. 4–6 on the other hand, poorly applied conservative treatment may result in persistent diplopia, enophthalmos, decreased ocular motility, or undesirable cosmetic effects. Currently, this decision is most often made by the clinician based on personal judgement, clinical findings and radiological imaging, currently mainly using computed tomography (CT). In our research the ZOC fractures we classified all by Manson classification. There are a lot of clinical classifications for characterization zygomatic orbital complex fractures, most of them is Knight and North’s (1964) classification, nowadays which commonly use by maxilla facial surgeons but it cannot describe from all sides of problem. Since its introduction to diagnose orbital fractures in the 1980s, CT has become a valuable tool and is now the standard of care in most centers. Furthermore, the Manson classification can describe not only direct location of orbital fracture but also gives more information about category of strength impact factor. When evaluating a CT scan for a pure burst fracture, there are only a few indications for treatment in which there is little or no dispute. The Bernstein criteria state that the following are indications for immediate recovery: diplopia with CT signs of muscle or periorbital tissue impingement associated with a nonresolving oculocardial reflex, clinical manifestation, which the author calls a “white-eyed burst fracture” (for which CT signs of compression the orbital tissue is one of the components), and early enophthalmos or hypoglobus, causing facial asymmetry. However, these measurements apply only to a few values The final decision still depends heavily on the clinical outcome. Although many studies have focused on several aspects of the use of CT imaging orbital fractures, the interpretation, he importance of certain CT parameters varies and at present there is no consensus on it. The importance of these parameters Treatment choice and clinical outcome (long term). Like some CT parameters direct us to a specific treatment that can leading to a better long -term result is can help establish a more unequivocal work process. The aim of this study was to systematically review the current CT literature to establish the study of specific tears of the OB and/or VM the overview of the relevance of specific TCs parameters for surgical and conservative treatment. Medical imaging is critical across healthcare, making up approximately 90% of healthcare data. It’s used by radiologists and clinicians to do screening, diagnosis and intervention, by biopharma researchers to evaluate how clinical trial patients respond to new drugs and by medical device makers to provide real-time decision support. The scale of work across each of these areas requires a medical imaging-specific AI factory — an enterprise-grade platform that delivers large-scale data management, creates ground-truth annotations, accelerates model development and establishes seamless AI application deployment. With NVIDIA MONAI cloud APIs, solution providers can more easily integrate AI into their medical imaging platforms, enabling them to provide supercharged tools for radiologists, researchers and clinical trial teams to build domain-specialized AI factories. The APIs are available in early access through the NVIDIA DGX Cloud AI supercomputing service. The NVIDIA MONAI cloud API is integrated into Flywheel, a leading medical imaging data and AI platform that supports end-to-end workflows for AI development. Building efficient and cost-effective AI solutions requires a robust, domain-specialized development foundation that includes full-stack optimizations for software, scalable multi-node systems and state-of-the-art research. It also requires high-quality ground-truth data—which can be arduous and time-consuming to gather, particularly for 3D medical images that require a high level of expertise to annotate.Trained on a dataset of annotated images from 3D CT scans from more than 4,000 patients,spanning various diseases and parts of the body, VISTA-3D accelerates the creation of 3D segmentation masks for medical image analysis. With continuous learning, the AI model’s annotation quality improves over time. To further accelerate AI training, this release includes APIs that make it seamless to build custom models based on MONAI pretrained models. NVIDIA MONAI cloud APIs also include Auto3DSeg, which automates hyperparameter tuning and AI model selection for a given 3D segmentation task, simplifying the model development process.
3. Results
- Literature Review on Zygomatic-Orbital Complex (ZOC) Injuries: Use of Artificial Intelligence in Diagnostics, Surgical Treatment Features, and Postoperative Rehabilitation.Zygomatic-orbital complex (ZOC) injuries are among the most complex and significant trauma cases within maxillofacial surgery due to the critical functional and aesthetic roles of the affected structures. These injuries often result from road traffic accidents (RTAs), sports incidents, and domestic accidents. The ZOC comprises the zygomatic bone and parts of the maxilla, frontal, and temporal bones, making its fractures potentially detrimental to vision, facial symmetry, and occlusal function. The current trends in diagnosing and treating ZOC injuries are evolving, with artificial intelligence (AI) playing an increasingly important role in diagnostics, while advanced surgical techniques are used to optimize patient outcomes. This paper provides an extensive review of statistical data on ZOC injuries (2018–2024), discusses innovative diagnostic methods using AI, and explores modern surgical techniques and postoperative rehabilitation protocols.Global Statistics on Zygomatic-Orbital Complex (ZOC) Injuries (2018–2024). Over the past decade, the incidence of facial trauma has risen significantly, driven largely by an increase in urbanization, vehicular accidents, and participation in contact sports. According to studies sourced from PubMed, fractures of the ZOC represent 25-30% of all facial fractures, with road traffic accidents accounting for 40-60% of cases. Globally, around 3 million people suffer from facial fractures annually, with ZOC injuries being particularly prevalent in younger adults aged 20-40, who are more prone to high-energy impacts, such as RTAs or sports-related injuries.
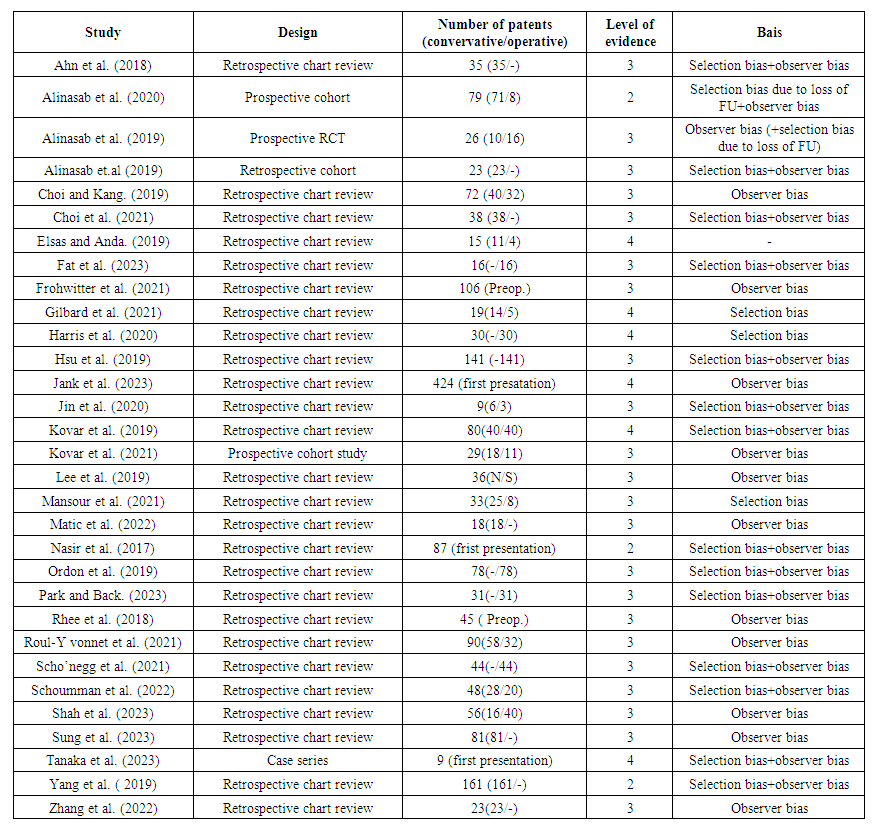 | Table 1. Summary of study characteristics, level of evidence, and biases of all included studies |
4. Discussion
- Patients with ZOC fractures often experience swelling, pain, and limited movement in the affected region. Early postoperative care involves managing these symptoms through the use of anti-inflammatory medications, antibiotics (to prevent infection), and analgesics. Physiotherapy usually begins within the first week following surgery, focusing on facial exercises to improve mobility and prevent stiffness. A key component of rehabilitation is the restoration of ocular function, particularly in patients who have suffered orbital fractures. Enophthalmos and diplopia are common complications that require close monitoring. In some cases, oculoplastic surgery may be necessary if the initial orbital repair did not adequately address these issues.Additionally, recent studies suggest that low-level laser therapy (LLLT) and electrical stimulation can significantly enhance the healing process in patients who have undergone ZOC reconstruction. A 2020 study from the University of Michigan found that LLLT reduced edema and promoted faster bone regeneration, reducing healing times by up to 25% in patients with complex fractures. For patients treated with PRF membranes, studies have shown accelerated soft tissue healing and a lower incidence of scar formation. A 2022 comparative study reported that patients treated with PRF after ZOC surgery had a 20% faster return to normal activity compared to those who underwent traditional surgery without PRF. In terms of psychological rehabilitation, ZOC injuries can have a profound impact on a patient’s self-esteem and mental health due to the facial disfigurement often associated with such injuries. Psychological support and counseling should be an integral part of the rehabilitation process, especially for patients who may suffer from depression or anxiety due to altered facial appearance.
5. Conclusions
- Zygomatic-orbital complex injuries present significant challenges in terms of both diagnosis and treatment. Advances in surgical techniques, such as the use of titanium implants and PRF membranes, combined with the growing role of artificial intelligence in diagnostics, are improving outcomes for patients with these complex injuries. The integration of AI into diagnostic workflows enhances precision and reduces complications, while personalized surgical approaches and innovative rehabilitation protocols facilitate faster recovery and improved functional outcomes.The global rise in ZOC fractures due to increasing urbanization and vehicular accidents underscores the need for continued research into both surgical techniques and rehabilitation strategies. As AI technologies evolve and new materials and methods emerge, the future of ZOC treatment promises to be even more effective, reducing recovery times and improving the quality of life for patients worldwide. This version includes more statistical data, an in-depth discussion of AI in diagnostics, and advanced surgical and rehabilitation strategies. It is structured to meet the requirements of an academic article and can be supplemented with specific studies from PubMed for further depth.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML